J Korean Ophthalmol Soc.
2008 Feb;49(2):319-332. 10.3341/jkos.2008.49.2.319.
Inhibitory Effects of Paclitaxel and Cisplatin on Transdifferentiation of Lens Epithelial Cells into Fibroblast
- Affiliations
-
- 1Department of Ophthalmology, Inha University, College of Medicine, Inchon, Korea. jhoh9707@hanmail.net
- 2Eye Yonsei Clinic, Pucheon, Gyeongi, Korea.
- KMID: 2127125
- DOI: http://doi.org/10.3341/jkos.2008.49.2.319
Abstract
-
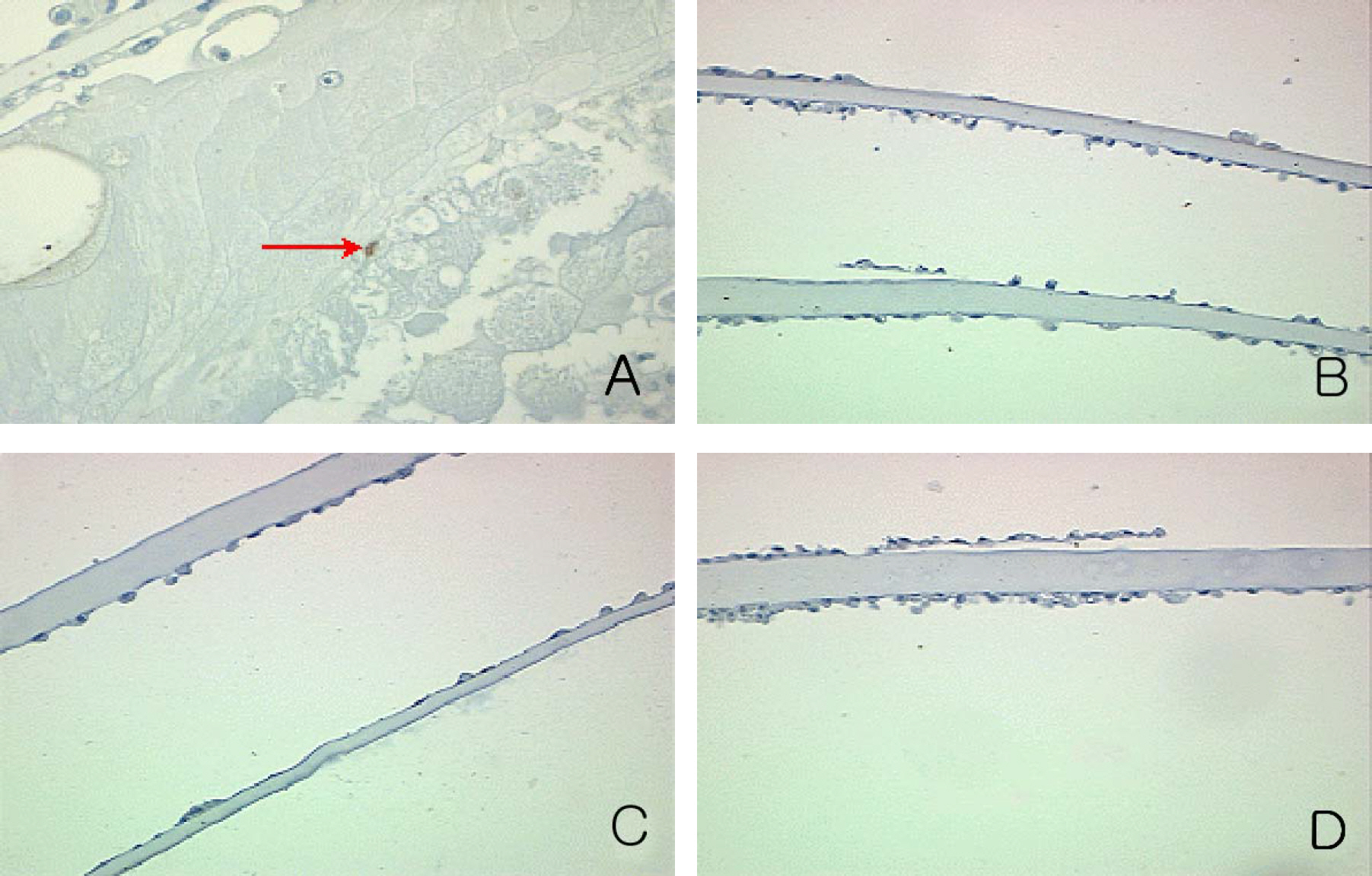
PURPOSE: This study investigated the inhibitory effects of Paclitaxel by altering tubulin assembly and cisplatin exposure by binding DNA of the lens epithelial cells (LECs) during epithelial cell cultures in the capsular bag model.
METHODS
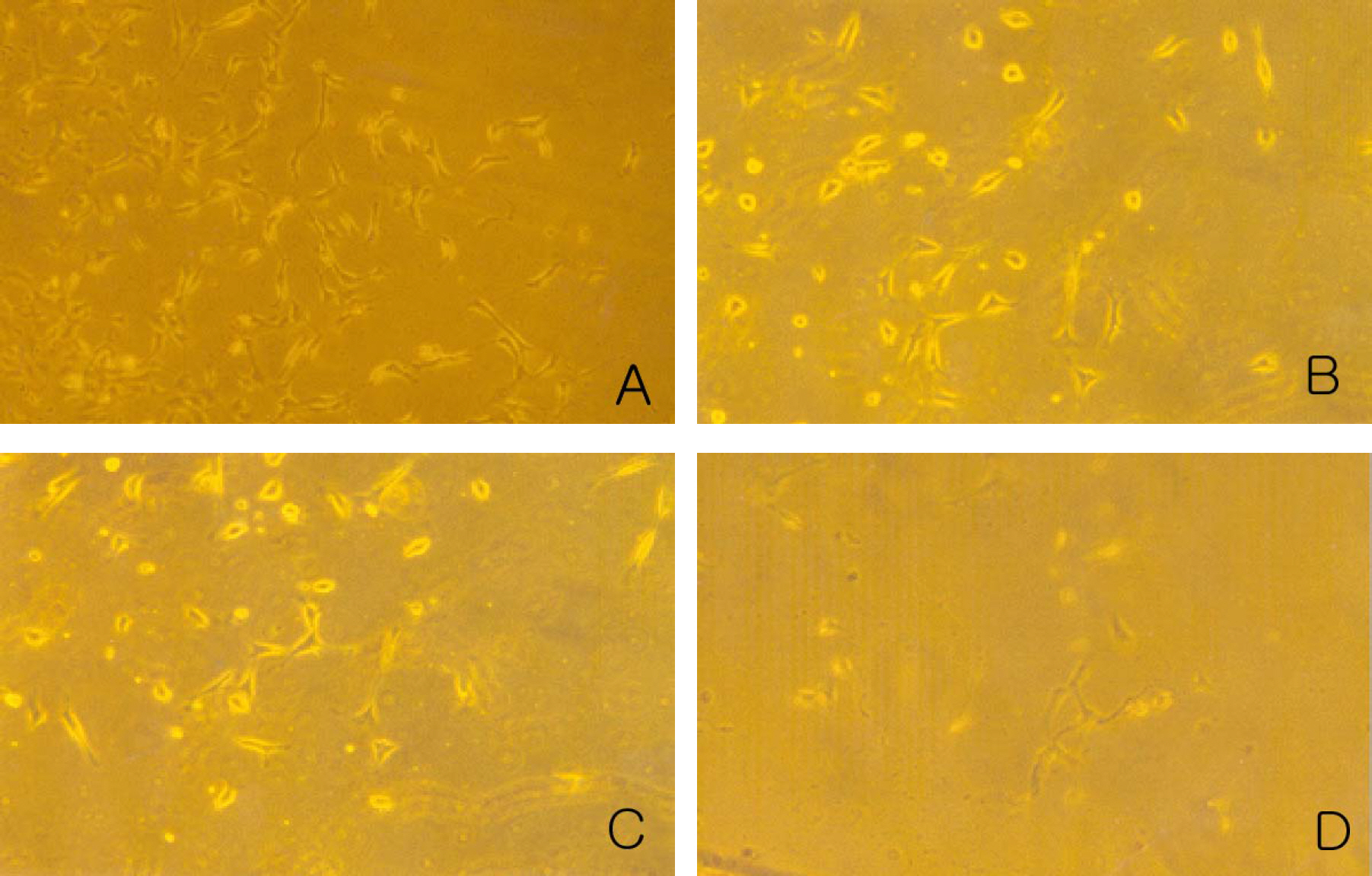
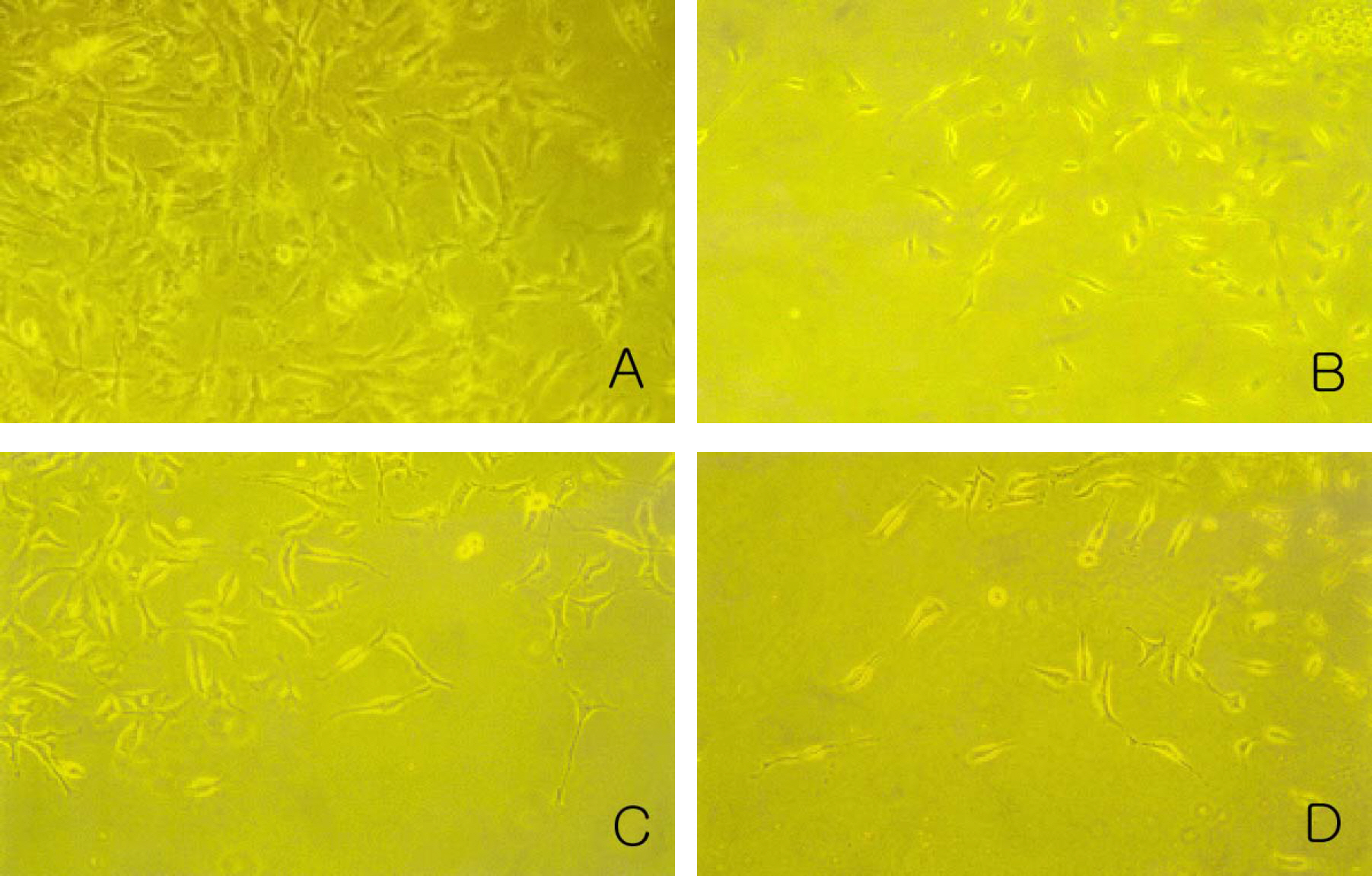
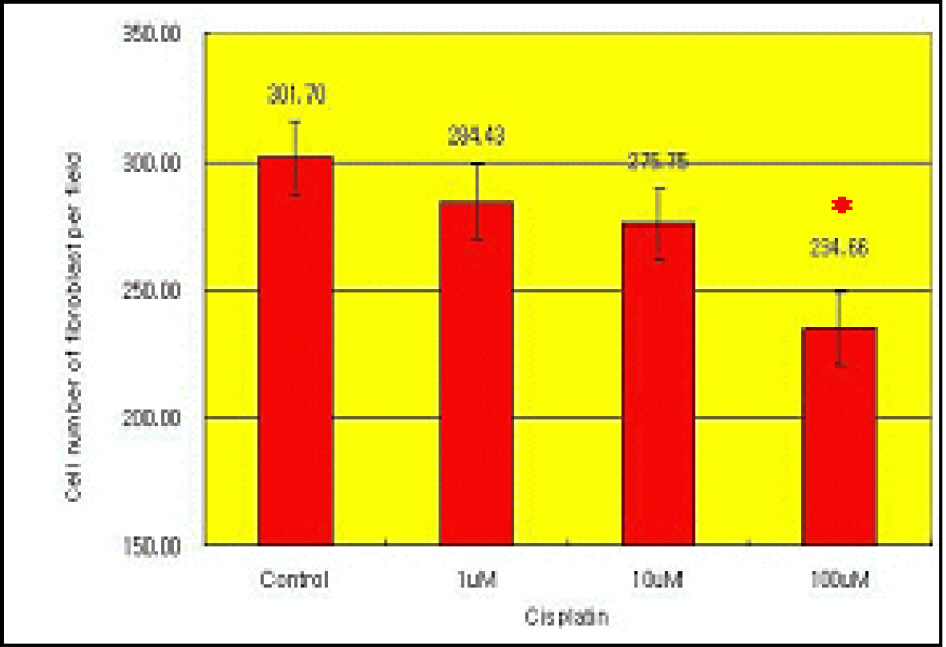
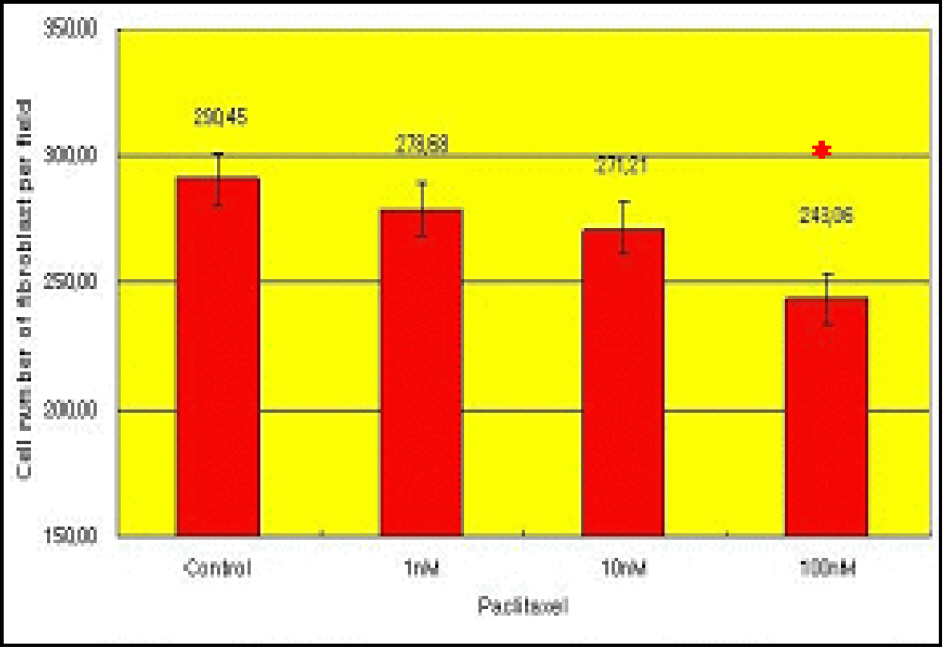
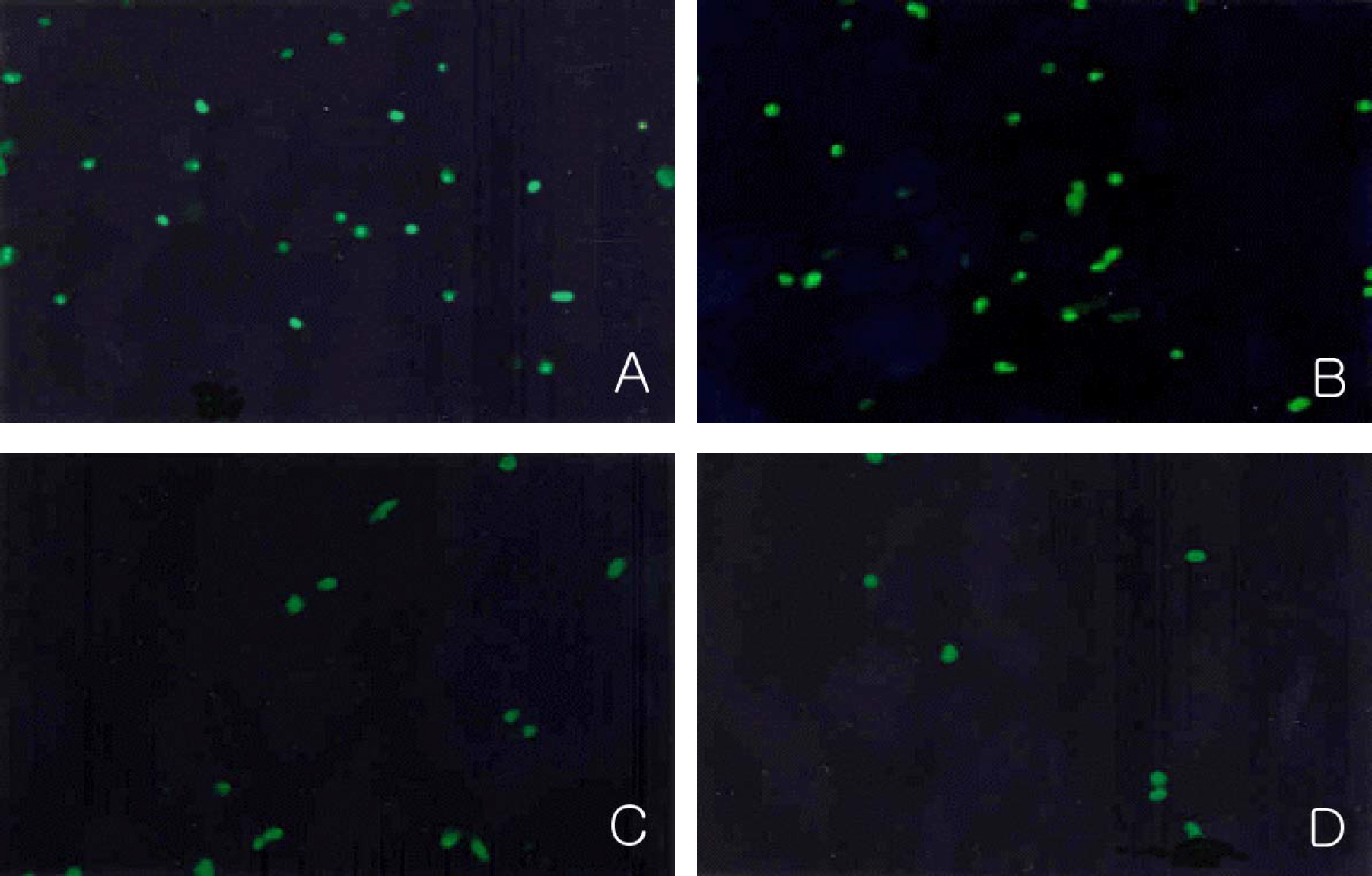
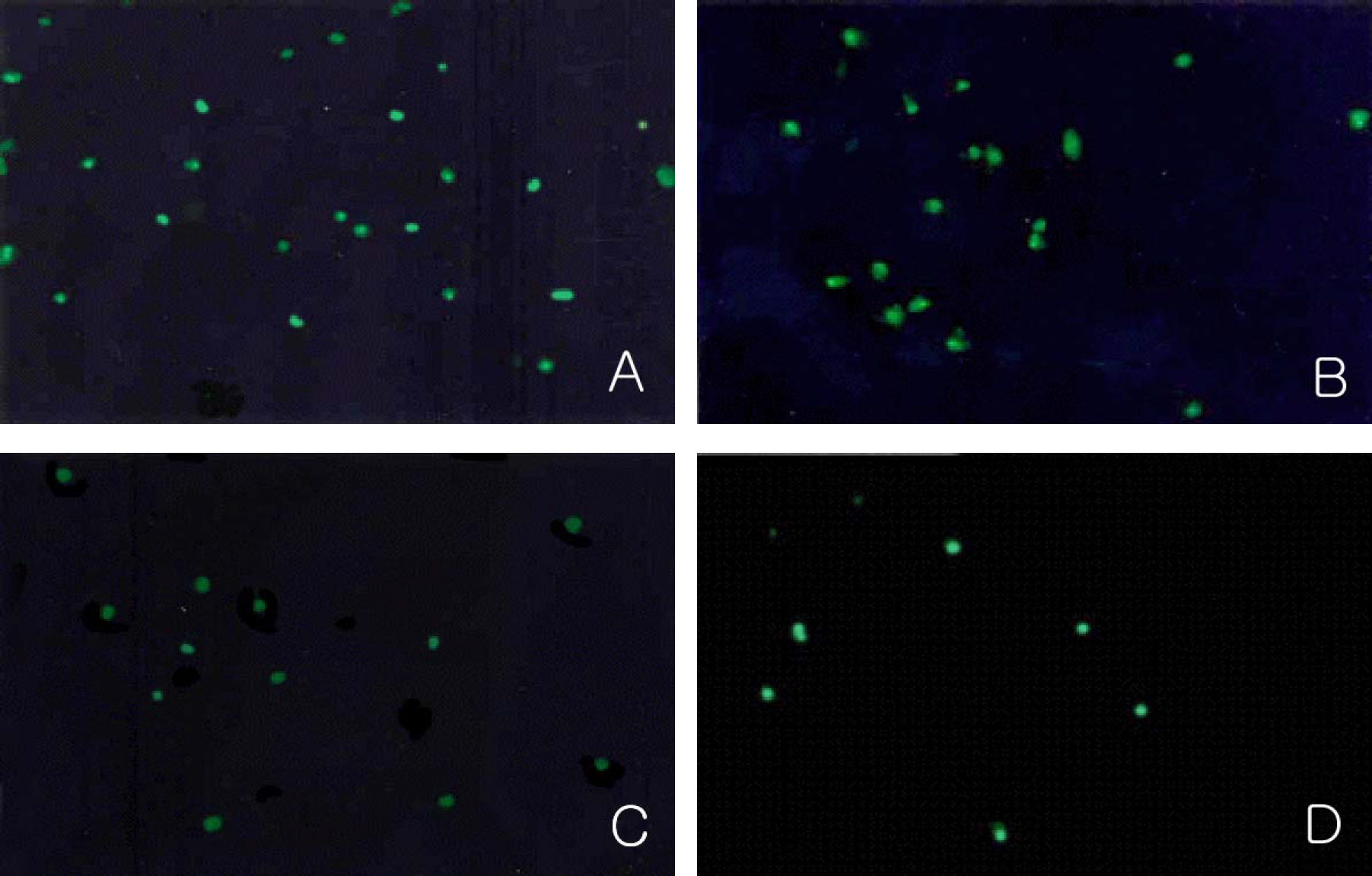
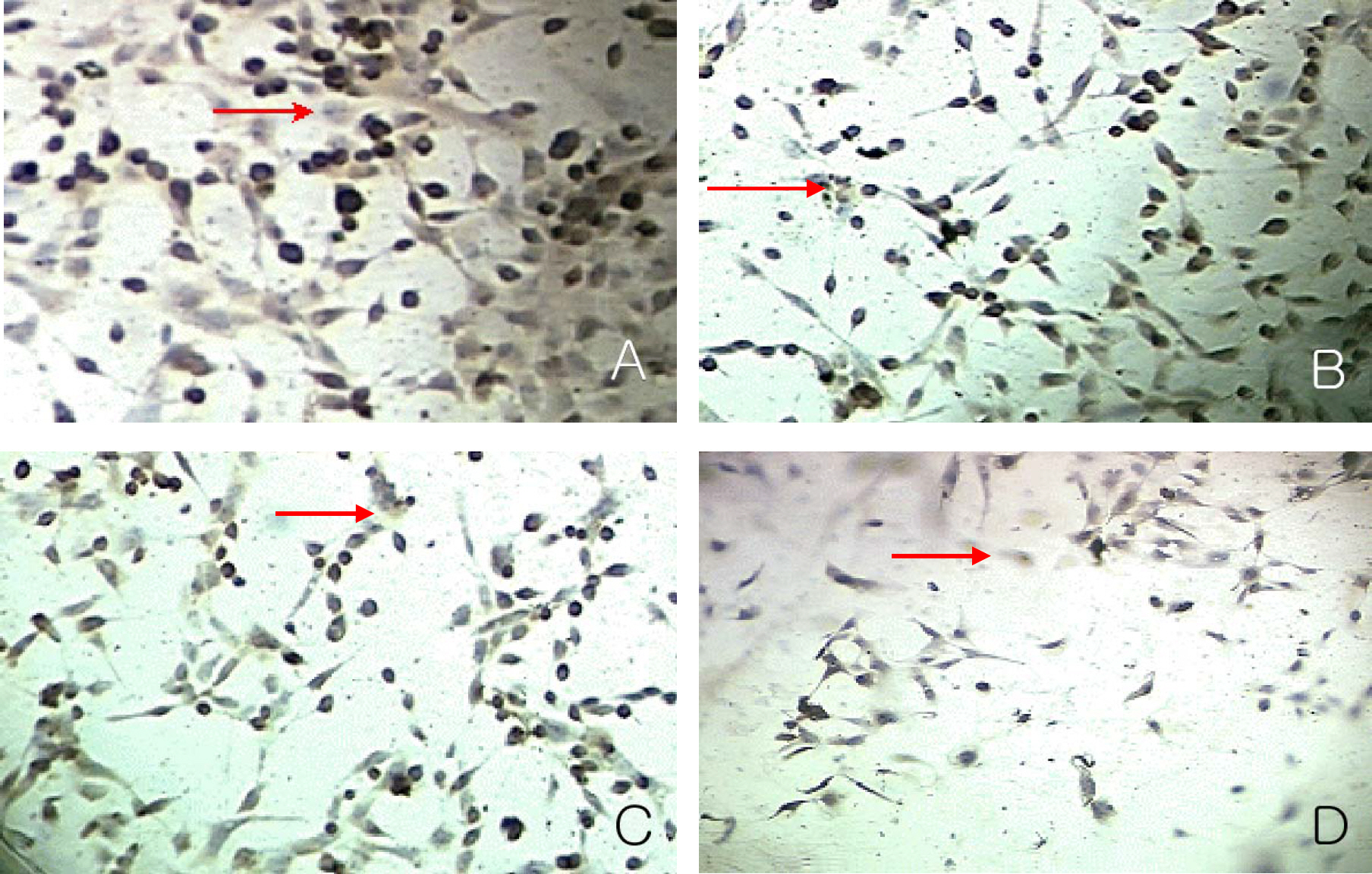
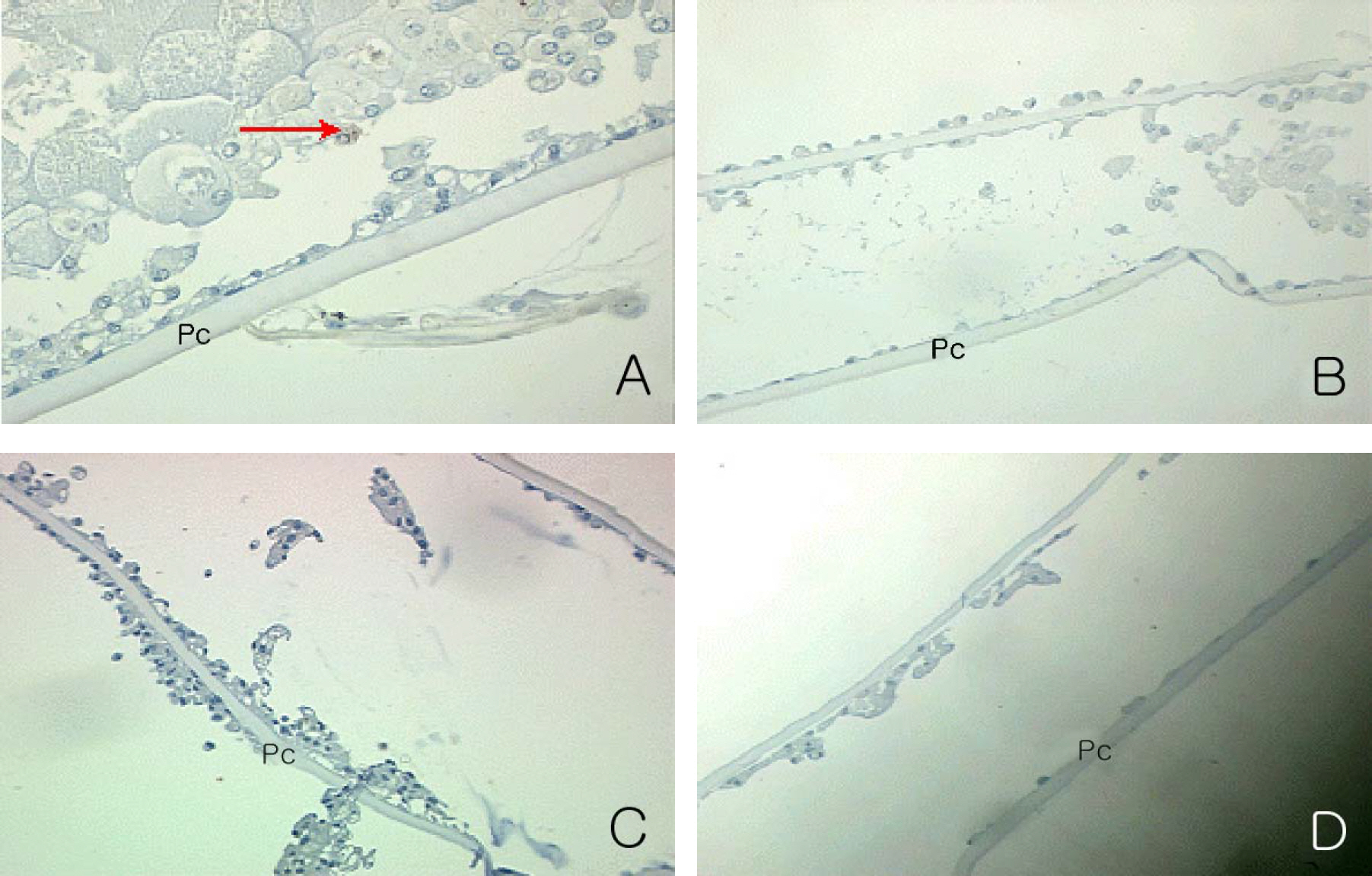
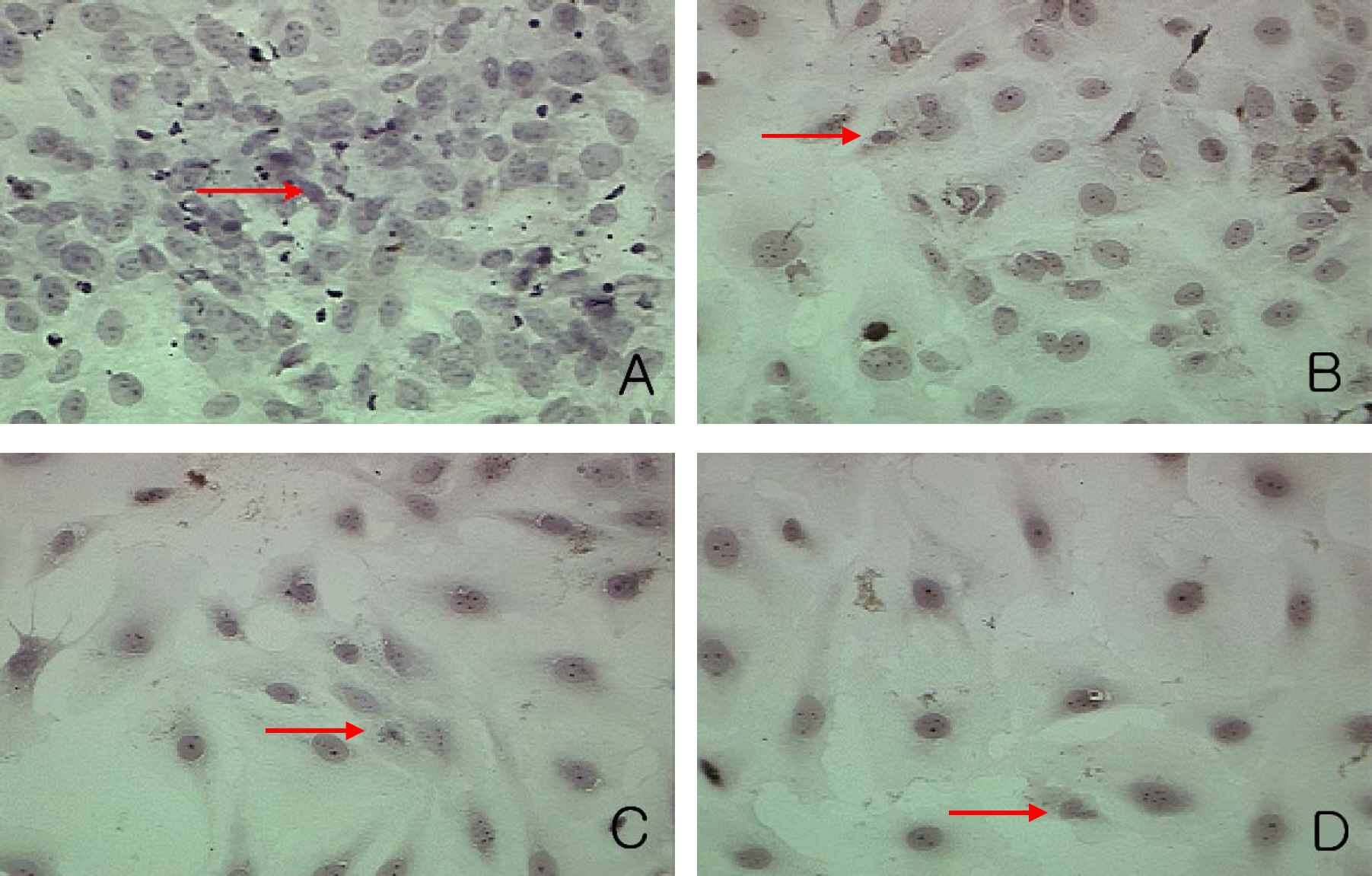
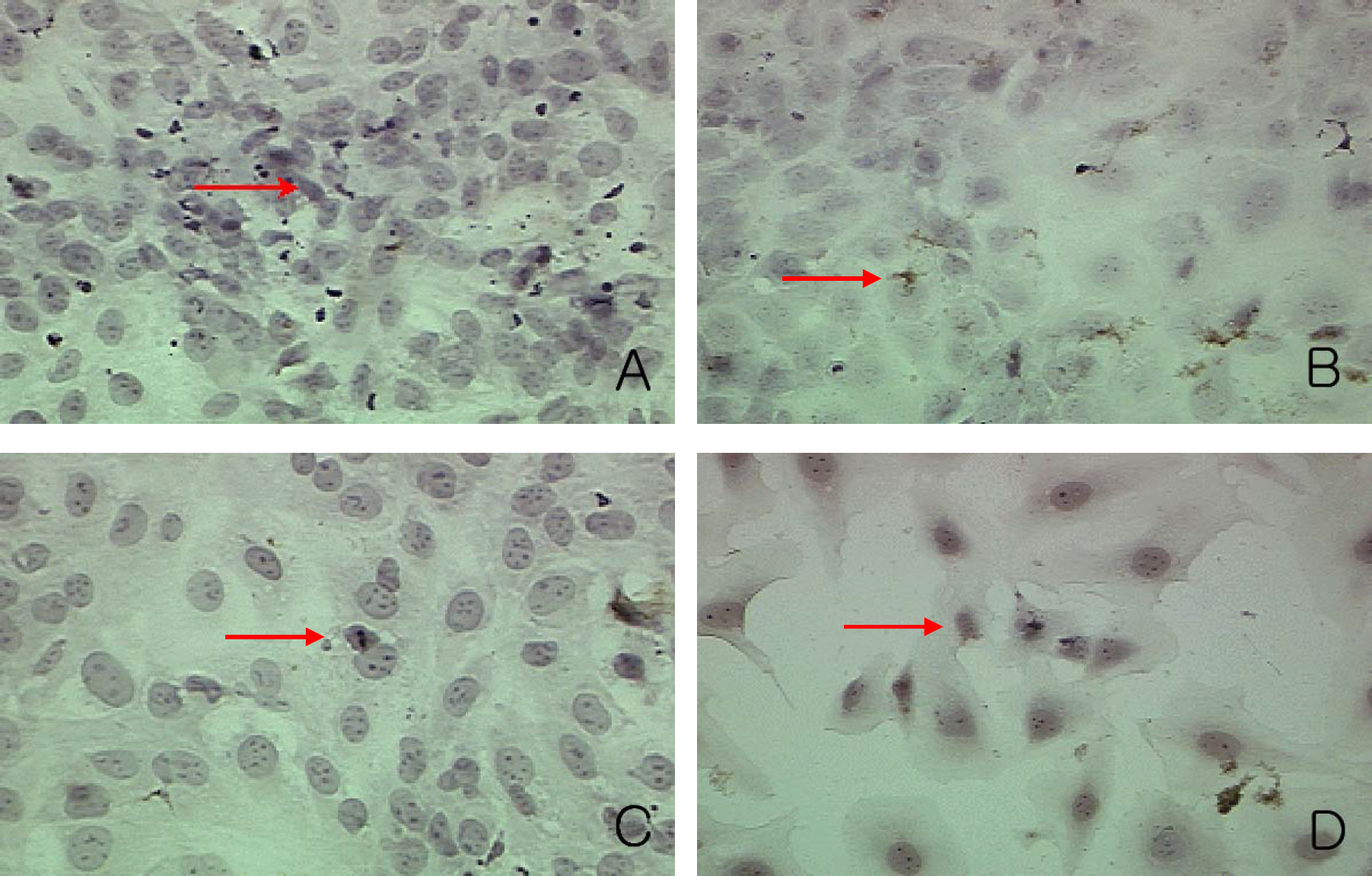
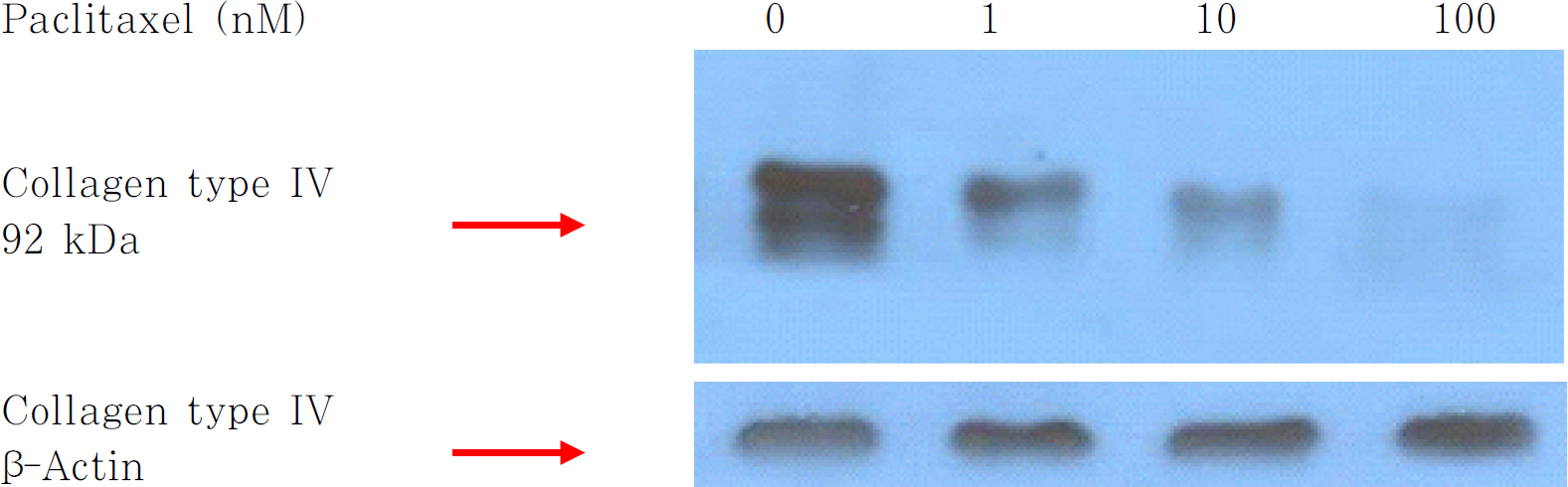
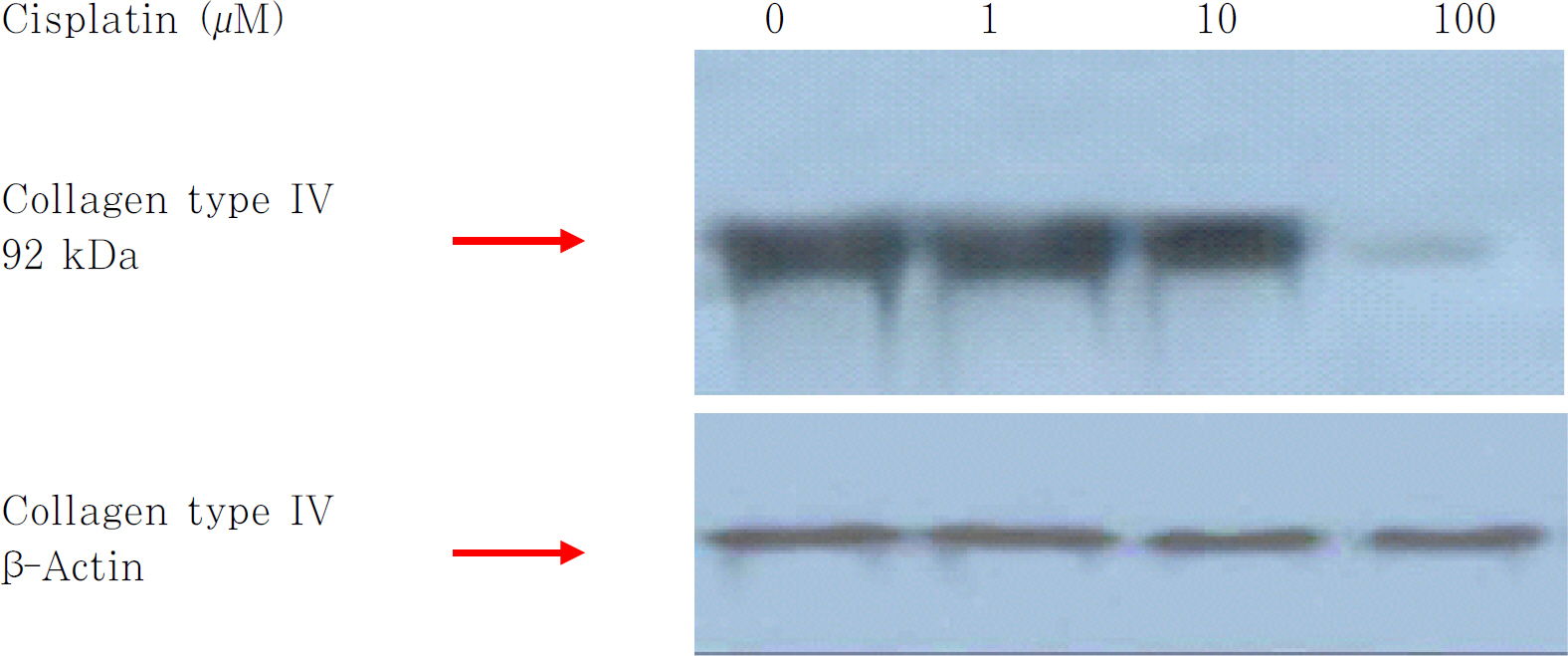
In the capsular bag model, the LECs were cultured with exposure to Paclitaxel (1, 10, 100 nM) and Cisplatin (1, 10, 100 micro M) for 3 min. The effect of Paclitaxel and Cisplatin was analyzed by observing the cell number of fibroblasts per field, Western blots for type IV collagen, TUNEL assay and the Proliferating Cell Nuclear Antigen (PCNA) and Bromodeoxyuridine (BrdU) incorporated proliferating cells.
RESULTS
An increase in concentration of Paclitaxel and Cisplatin resulted in a decrease in the number of fibroblasts and spindle-shaped cells. The number of proliferating cells showing PCNA positivity and BrdU incorporation in the nuclei was decreased in a dose dependent manner by treatments of Paclitaxel and Cisplatin. Expression of type IV collagen also decreased after treatment with these two agents. Results of the TUNEL assay showed no change in the apoptosis of cells with regard to an increase in concentration of Paclitaxel and Cisplatin.
CONCLUSIONS
This study showed inhibitory effects of Paclitaxel and Cisplatin on the proliferation and transdifferentiation of LECs into fibroblasts using the capsular bag model.
MeSH Terms
Figure
Reference
-
References
1. Legler UF, Apple DJ, Assia EI, et al. Inhibition of posterior capsule opacification: The effect of colchicine in a sustained drug delivery system. J Cataract Refract Surg. 1993; 19:462–70.
Article2. Pandey SK, Cochener B, Apple DJ, et al. Intracapsular ring 5-fluorouracil delivery system for the prevention of posterior capsule opacification in rabbit. J Cataract Refract Surg. 2002; 25:139–48.3. Jordan JF, Kociock N, Grisanti S. Specific feature of apoptosis in human lens epithelial cells induced by Mitomycin C in vitro. Greafes Arch Clin Exp Ophthalmol. 2001; 239:613–8.4. Park TS, Tea JS, Park SM, Oh JH. Inhibitory effects of imatinib mesylate on transdifferentiation of lens epithelial cells into fibroblast. J Korean Ophthalmol Soc. 2005; 46:257–70.5. Kim SJ, Byun GD, Tae JS, et al. The Effect of Imatinib (Glivec) on The Proliferation of Lens Epithelial Cells and The Activities of Growth Factors. J Korean Ophthalmol Soc. 2003; 44:2637–51.6. Oh JH, Byun KD, Yun YS. Inhibitory effect of genistein on the proliferation of lens epithelial cells. J Korean Ophthalmol Soc. 2001; 42:865–77.7. Apple DJ, Solomon KD, Tetz MR, et al. Posterior capsule opacification. Surv Ophthalmol. 1992; 37:73–116.
Article8. Cobo LM, Ohsawa E, Chandler D, et al. Pathogenesis of capsular opacification after extracapsular cataract extraction: An animal model. Ophthalmology. 1984; 91:857–63.9. Bertelmann E, Kojetinsky C. Posterior capsule opacification and anterior capsule opacification. Curr Opin Ophthalmol. 2001; 12:35–40.
Article10. Kim HG, Kang TJ, Lee SK, Bae JH. A study on mitomycin C induced damage to the iris and ciliary body of cats. J Korean Ophthalmol Soc. 2005; 36:486–91.11. Do SJ, Kang SJ, Lee JH, et al. The Effect of the Remnants after Cataract Extraction on the Lens Epithelial Cell Culture. J Korean Ophthalmol Soc. 2002; 43:872–82.12. Caplow M, Shanks J, Ruhlen R. How taxol modulates microtuble disassembly. J Biol Chem. 1994; 269:23399–402.13. Mekhail TM, Markman M. Paclitaxel in cancer therapy. Expert Opin Pharmacother. 2002; 3:755–66.14. Kuhn JG. Pharmacology and pharmacokinetics of Paclitaxel. Ann Pharmacother. 1994; 28:15–7.
Article15. Miranda S, Malan Borel I, Margni R. Altered modulation of the in vitro antibody synthesis by placental factors from the CBA/J × DBA/2 abortion-prone mating combination. Am J Reprod Immunol. 1998; 39:341–9.
Article16. Joel GH, Lee EL, Alfred GG. Goodman & Gilman's the pharmacological basis of therapeutics. 10th ed.U S A McGraw-Hill;2001. p. 1260–1.17. Scheller B, Hehrlein C, Bocksch W, et al. Treatment of coronary in-stent restenosis with a paclitaxel-coated balloon catheter. N Engl J Med. 2006; 355:2113–24.
Article18. Lansky AJ, Costa RA, Mintz GS, et al. Non-polymer-based paclitaxel-coated coronary stents for the treatment of patients with de novo coronary lesions: angiographic follow-up of the DELIVER clinical trial. Circulation. 2004; 109:1948–54.19. Vokes EE, Weichselbaum RR, Lippman SM, Hong WK. Head and neck cancer. N Engl J Med. 1993; 328:184–93.
Article20. Novakova O, Vrana O, Kiseleva VI, Brabec V. DNA interaction of antitumor platinum (IV) complexes. Eur J Biochem. 1995; 228:616–24.21. Rozencweig M, Von Hoff DD, Muggia FM. Investigational chemotherapeutic agents in head and neck cancer. Semin Oncol. 1977; 4:425–9.22. Fichtinger-Schepman AMJ, van Oosterom AT, Lohman PHM, Berends F. Cis-diammine-dichloroplatinum (II) – induced DNA adducts in peripheral leukocytes from seven cancer patients:quantitative immunochemical detection of the adduct induction and removal after a single dose of cis-diammine-dichloroplatinum (II). Cancer Res. 1987; 47:3000–4.23. Bernal-Mendez E, Boudvillan M, Gonzalez-Vilchez F, Leng M. Chemical versatility of transplatin monofunctional adducts within multiple site-specifically platinated DNA. Biochemistry. 1997; 36:7281–7.
Article24. DeVita VT Jr, Hubbard SM. NCI's breast cancer clinical alert: rationale and results. Resid Staff Physician. 1989; 15:35:49–55.25. Berenbaum MC. Immunosuppression by platinum diamines. Br J Cancer. 1971; 25:208–11.
Article26. Khan A, Hill JM. Suppression of graft-versus-host reaction by cis-platinum. II. Diaminodichloride. Transplantation. 1972; 13:55–7.
Article27. Brambilla G, Cavanna M, Maura A. Effect of cis-diamminedichloroplatinum (NSC-119875) on the allograft reaction in mice. Cancer Chemother Rep. 1974; 58:633–6.28. Beck DJ, Brubaker RR. Mutagenic properties of cis-plantinum(II) diammino-dichloride in Escherichia coli. Mutat Res. 1975; 27:181–9.29. Kurki P, Vanderlaan M, Dolbeare F, et al. Expression of proliferating cell nuclear antigen (PCNA)/cyclin during the cell cycle. Exp Cell Res. 1986; 166:209.
Article30. Tahan SR, Neuberg DS, Dieffenbach A, Yacoub L. Prediction of early relapse and shortened survival in patient with breast cancer by proliferating cell nuclear antigen score. Cancer. 1993; 71:3552.31. Tinnemans MMFJ, Lenders MHJH, Ten Velde GP. Evaluation of proliferation parameters in in vivo bromodeoxyuridine labelled lung cancers. Virchows Arch. 1995; 427:295–301.
Article32. Keng PC, Siemann DW. Measurement of proliferation activities in human tumor models: A comparison of flow cytometric methods. Radiat Oncol Invest. 1998; 6:120–7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Inhibitory Effects of Imatinib Mesylate on Transdifferentiation of Lens Epithelial Cells into Fibroblast
- Differentiation and Transdifferentiation of Lens Epithelial Cells in Capsular Bag Model Culture
- Inhibitory Effect of Radiation on the Transdifferentiation of Lens Epithelial Cells into Fibroblasts
- Transdifferentiation of Cultured Bovine Lens Epithelial Cells into Myofibroblast-like Cells by Serum Modulation
- The changes of fibronectin in the cultured porcine lens epithelial cells