J Korean Neurosurg Soc.
2015 Jan;57(1):23-31. 10.3340/jkns.2015.57.1.23.
The Influence of Pituitary Adenoma Size on Vision and Visual Outcomes after Trans-Sphenoidal Adenectomy: A Report of 78 Cases
- Affiliations
-
- 1Department of Neurosurgery, Kaohsiung Chang Gung Memorial Hospital, Chang Gung University College of Medicine, Kaohsiung, Taiwan. jihtsunho@yahoo.com.tw
- KMID: 2067087
- DOI: http://doi.org/10.3340/jkns.2015.57.1.23
Abstract
OBJECTIVE
The aims of this study were to investigate the quantitative relationship between pituitary macroadenoma size and degree of visual impairment, and assess visual improvement after surgical resection of the tumor.
METHODS
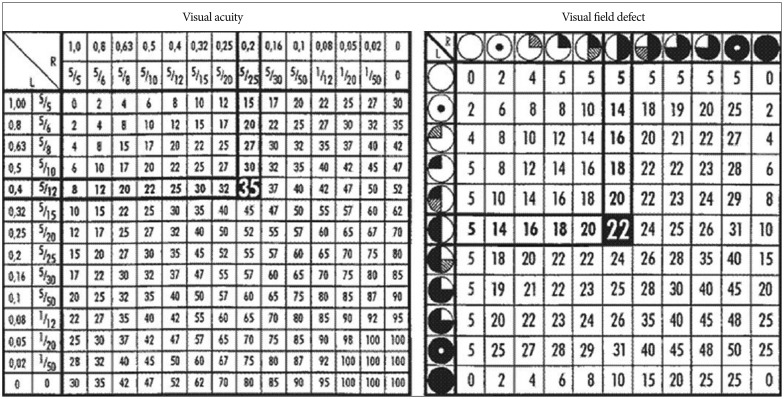
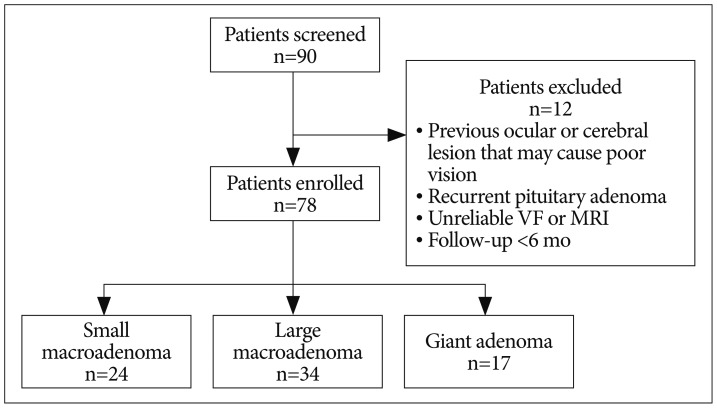
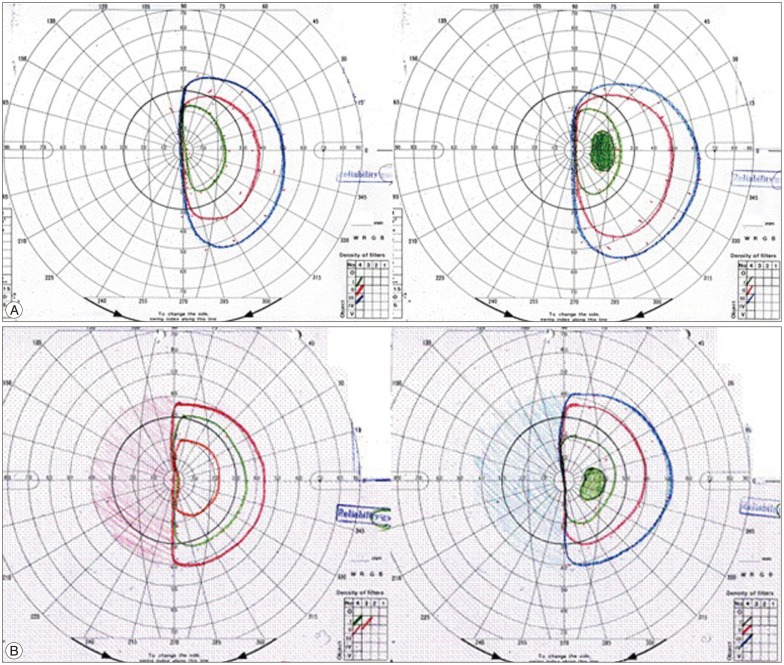
The medical records of patients with pituitary adenoma, who had undergone trans-sphenoidal adenectomy between January 2009 and January 2011, were reviewed. Patients underwent an ocular examination and brain MRI before and after surgery. The visual impairment score (VIS) was derived by combining the scores of best-corrected visual acuity and visual field. The relationship between VIS and tumor size/tumor type/position of the optic chiasm was assessed.
RESULTS
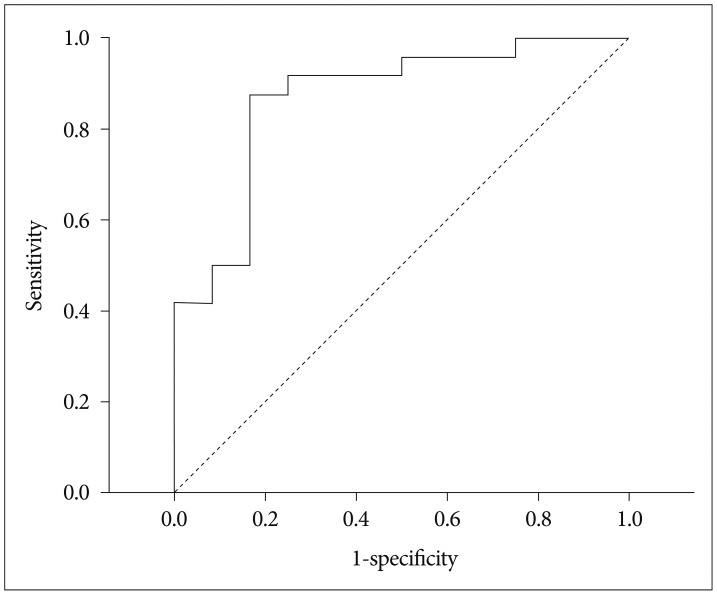
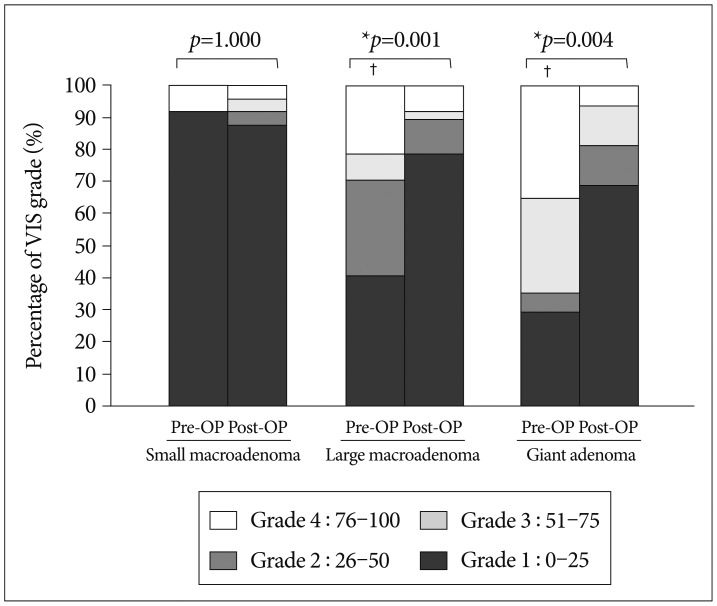
Seventy-eight patients were included (41 male, 37 female). Thirty-two (41%) patients experienced blurred vision or visual field defect as an initial symptom. Receiver operating characteristic curve analysis showed that tumors <2.2 cm tended to cause minimal or no visual impairment. Statistical analysis showed that 1) poor preoperative vision is related to tumor size, displacement of the optic chiasm in the sagittal view on MRI and optic atrophy, and 2) poorer visual prognosis is associated with greater preoperative VIS. In multivariate analysis the only factor significantly related to VIS improvement was increasing pituitary adenoma size, which predicted decreased improvement.
CONCLUSION
Results from this study show that pituitary adenomas larger than 2 cm cause defects in vision while adenomas 2 cm or smaller do not cause significant visual impairment. Patients with a large macroadenoma or giant adenoma should undergo surgical resection as soon as possible to prevent permanent visual loss.
MeSH Terms
Figure
Cited by 2 articles
-
Factors Influencing Visual Field Recovery after Transsphenoidal Resection of a Pituitary Adenoma
Dong Kyu Lee, Mi Sun Sung, Sang Woo Park
Korean J Ophthalmol. 2018;32(6):488-496. doi: 10.3341/kjo.2017.0094.Parasellar Extension Grades and Surgical Extent in Endoscopic Endonasal Transsphenoidal Surgery for Pituitary Adenomas : A Single Surgeon's Consecutive Series with the Aspects of Reliability and Clinical Validity
Sang-Hyo Lee, Jae-Sung Park, Song Lee, Sung-Won Kim, Yong-Kil Hong
J Korean Neurosurg Soc. 2016;59(6):577-583. doi: 10.3340/jkns.2016.59.6.577.
Reference
-
1. Anderson D, Faber P, Marcovitz S, Hardy J, Lorenzetti D. Pituitary tumors and the ophthalmologist. Ophthalmology. 1983; 90:1265–1270. PMID: 6664664.
Article2. Anderson DR. Perimetry: With and Without Automation. ed 2. St. Louis: Mosby;1987.3. Chang EF, Zada G, Kim S, Lamborn KR, Quinones-Hinojosa A, Tyrrell JB, et al. Long-term recurrence and mortality after surgery and adjuvant radiotherapy for nonfunctional pituitary adenomas. J Neurosurg. 2008; 108:736–745. PMID: 18377253.
Article4. Ciric I, Ragin A, Baumgartner C, Pierce D. Complications of transsphenoidal surgery: results of a national survey, review of the literature, and personal experience. Neurosurgery. 1997; 40:225–236. discussion 236-237. PMID: 9007854.
Article5. Cohen AR, Cooper PR, Kupersmith MJ, Flamm ES, Ransohoff J. Visual recovery after transsphenoidal removal of pituitary adenomas. Neurosurgery. 1985; 17:446–452. PMID: 4047355.
Article6. Colao A, Di Somma C, Pivonello R, Faggiano A, Lombardi G, Savastano S. Medical therapy for clinically non-functioning pituitary adenomas. Endocr Relat Cancer. 2008; 15:905–915. PMID: 18780796.
Article7. Ebersold MJ, Quast LM, Laws ER Jr, Scheithauer B, Randall RV. Long-term results in transsphenoidal removal of nonfunctioning pituitary adenomas. J Neurosurg. 1986; 64:713–719. PMID: 3701419.
Article8. Ezzat S, Asa SL, Couldwell WT, Barr CE, Dodge WE, Vance ML, et al. The prevalence of pituitary adenomas: a systematic review. Cancer. 2004; 101:613–619. PMID: 15274075.9. Fahlbusch R, Schott W. Pterional surgery of meningiomas of the tuberculum sellae and planum sphenoidale: surgical results with special consideration of ophthalmological and endocrinological outcomes. J Neurosurg. 2002; 96:235–243. PMID: 11838796.
Article10. Ferrante E, Ferraroni M, Castrignanò T, Menicatti L, Anagni M, Reimondo G, et al. Non-functioning pituitary adenoma database: a useful resource to improve the clinical management of pituitary tumors. Eur J Endocrinol. 2006; 155:823–829. PMID: 17132751.
Article11. Fluss R, Faraggi D, Reiser B. Estimation of the Youden Index and its associated cutoff point. Biom J. 2005; 47:458–472. PMID: 16161804.
Article13. Garibi J, Pomposo I, Villar G, Gaztambide S. Giant pituitary adenomas: clinical characteristics and surgical results. Br J Neurosurg. 2002; 16:133–139. PMID: 12046731.
Article14. Gnanalingham KK, Bhattacharjee S, Pennington R, Ng J, Mendoza N. The time course of visual field recovery following transphenoidal surgery for pituitary adenomas: predictive factors for a good outcome. J Neurol Neurosurg Psychiatry. 2005; 76:415–419. PMID: 15716538.
Article15. Goel A, Nadkarni T, Muzumdar D, Desai K, Phalke U, Sharma P. Giant pituitary tumors: a study based on surgical treatment of 118 cases. Surg Neurol. 2004; 61:436–445. discussion 445-446. PMID: 15120215.
Article16. Hennessey JV, Jackson IM. Clinical features and differential diagnosis of pituitary tumours with emphasis on acromegaly. Baillieres Clin Endocrinol Metab. 1995; 9:271–314. PMID: 7625986.
Article17. Hollenhorst RW, Younge BR. Ocular manifestations produced by adenomas of the pituitary gland: analysis of 1000 cases. In : Kohler PO, Ross GT, editors. Diagnosis and Treatment of Pituitary Tumors. Amsterdam: Excepta Medica;1973. p. 53–63.18. Ikeda H, Yoshimoto T. Visual disturbances in patients with pituitary adenoma. Acta Neurol Scand. 1995; 92:157–160. PMID: 7484065.
Article19. Jaeger W, Thomann H. [German Ophthalmological Association. Recommendations for evaluation of reduced earning capacity caused by damage to vision. September 1981]. Klin Monbl Augenheilkd. 1982; 180:242–244. PMID: 7078020.20. Jaffe CA. Clinically non-functioning pituitary adenoma. Pituitary. 2006; 9:317–321. PMID: 17082898.
Article21. Kerrison JB, Lynn MJ, Baer CA, Newman SA, Biousse V, Newman NJ. Stages of improvement in visual fields after pituitary tumor resection. Am J Ophthalmol. 2000; 130:813–820. PMID: 11124302.
Article22. Krisht AF. Giant invasive pituitary adenomas: management plan. Contemp Neurosurg. 1999; 21:1–5.23. Lee JP, Park IW, Chung YS. The volume of tumor mass and visual field defect in patients with pituitary macroadenoma. Korean J Ophthalmol. 2011; 25:37–41. PMID: 21350693.
Article24. Levy A. Pituitary disease: presentation, diagnosis, and management. J Neurol Neurosurg Psychiatry. 2004; 75(Suppl 3):iii47–iii52. PMID: 15316045.
Article25. Miller NR. Walsh and Hoyt's Clinical Neuro-Ophthalmology. ed 4. Baltimore: Williams & Wilkins;1988. p. 1433–1484.26. Miller NR, Newman NJ, Biousse V, Kerrison JB. Walsh & Hoyt's Clinical Neuro-Ophthalmology. ed 6. Philadelphia: Lippincott Williams & Wilkins;2005. p. 503–573.27. Monteiro ML, Zambon BK, Cunha LP. Predictive factors for the development of visual loss in patients with pituitary macroadenomas and for visual recovery after optic pathway decompression. Can J Ophthalmol. 2010; 45:404–408. PMID: 20648089.
Article28. Mortini P, Barzaghi R, Losa M, Boari N, Giovanelli M. Surgical treatment of giant pituitary adenomas: strategies and results in a series of 95 consecutive patients. Neurosurgery. 2007; 60:993–1002. discussion 1003-1004. PMID: 17538372.29. Müslüman AM, Cansever T, Yılmaz A, Kanat A, Oba E, ÇavuŞoğlu H, et al. Surgical results of large and giant pituitary adenomas with special consideration of ophthalmologic outcomes. World Neurosurg. 2011; 76:141–148. discussion 63-66. PMID: 21839965.
Article30. Nishimura M, Kurimoto T, Yamagata Y, Ikemoto H, Arita N, Mimura O. Giant pituitary adenoma manifesting as homonymous hemianopia. Jpn J Ophthalmol. 2007; 51:151–153. PMID: 17401630.
Article31. Peter M, De Tribolet N. Visual outcome after transsphenoidal surgery for pituitary adenomas. Br J Neurosurg. 1995; 9:151–157. PMID: 7632360.
Article32. Powell M. Recovery of vision following transsphenoidal surgery for pituitary adenomas. Br J Neurosurg. 1995; 9:367–373. PMID: 7546358.
Article33. Rivoal O, Brézin AP, Feldman-Billard S, Luton JP. Goldmann perimetry in acromegaly: a survey of 307 cases from 1951 through 1996. Ophthalmology. 2000; 107:991–997. PMID: 10811095.34. Roelfsema F, Biermasz NR, Pereira AM. Clinical factors involved in the recurrence of pituitary adenomas after surgical remission: a structured review and meta-analysis. Pituitary. 2012; 15:71–83. PMID: 21918830.
Article35. Sivakumar W, Chamoun R, Nguyen V, Couldwell WT. Incidental pituitary adenomas. Neurosurg Focus. 2011; 31:E18. PMID: 22133173.
Article36. Thomas R, Shenoy K, Seshadri MS, Muliyil J, Rao A, Paul P. Visual field defects in non-functioning pituitary adenomas. Indian J Ophthalmol. 2002; 50:127–130. PMID: 12194569.37. Westheimer G. Visual acuity. In : Kaufman PL, Alm A, Adler FH, editors. Adler's Physiology of the Eye : clinical application. ed 10. St. Louis, MO: CV Mosby;2003. p. 453–469.38. Wilson CB. Surgical management of pituitary tumors. J Clin Endocrinol Metab. 1997; 82:2381–2385. PMID: 9253304.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Silent Corticotropic Adenomas of the Pituitary Gland: Cases Report
- Trigemino-cardiac reflex: occurrence of asystole during trans-sphenoidal adenomectomy: a case report
- Feasibility of Endoscopic Endonasal Approach for Recurrent Pituitary Adenomas after Microscopic Trans-Sphenoidal Approach
- Pituitary Adenoma Accompanying Sphenoidal Meningoencephalocele with Clival Extension
- Pituitary Apoplexy: Surgical Experience with 16 Patients