Infect Chemother.
2012 Apr;44(2):71-74. 10.3947/ic.2012.44.2.71.
A Case of Severe Community-acquired Acinetobacter baumannii Pneumonia with Bacteremia
- Affiliations
-
- 1Department of Internal Medicine, College of Medicine, Ulsan University, Seoul Asan Medical Center, Seoul, Korea.
- 2Department of Pulmonary and Critical Care Medicine, College of Medicine, Ulsan University, Seoul Asan Medical Center, Seoul, Korea.
- 3Department of Infectious Diseases, College of Medicine, Ulsan University, Seoul Asan Medical Center, Seoul, Korea. sangho@amc.seoul.kr
- KMID: 2054439
- DOI: http://doi.org/10.3947/ic.2012.44.2.71
Abstract
- Acinetobacter baumannii is a significant pathogen in nosocomial infections, especially in intensive care units. However, community-acquired A. baumannii (CAAB) pneumonia is an uncommon disease. Most of the CAAB pneumonia in the literature is characterized by an abrupt onset and rapid progression to respiratory failure and hemodynamic instability. In our case, a 51-year-old man without underlying diseases developed severe pneumonia. Respiratory distress rapidly worsened and mechanical ventilation was applied. Extra-corporeal membrane oxygenation was applied due to refractory septic shock. Fully sensitive A. baumannii pneumonia was confirmed by the sputum culture and blood culture. The patient was effectively treated by the meropenem. However, the patient died of uncontrolled ventilator-associated pneumonia, developed on the 10th hospital day, and refractory septic shock. We report the case of severe CAAB pneumonia with bacteremia in a patient without underlying diseases in Korea.
MeSH Terms
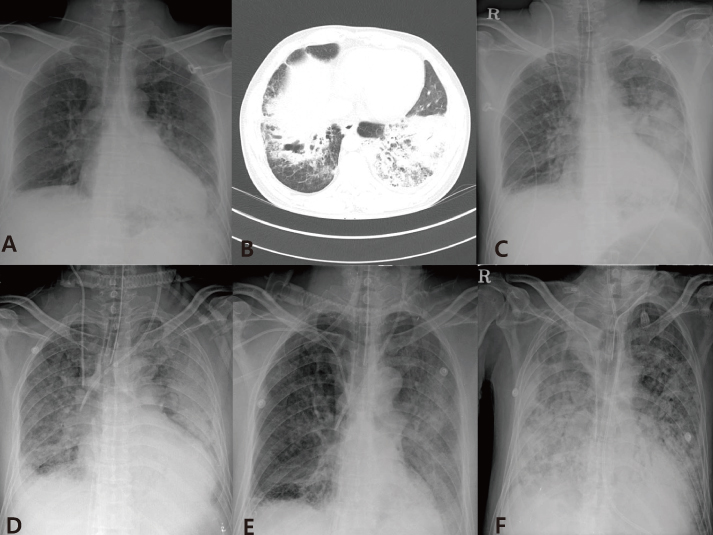
Figure
Cited by 2 articles
-
A Case of Community-Acquired Acinetobacter Meningitis
Seo Hee Ryu, Chang Min Yu, Seong O Suh, Jun Hwan Kim, Yu Jin Ko, Jae Hyun Park, Jae Hyun Cho
Infect Chemother. 2012;44(6):473-476. doi: 10.3947/ic.2012.44.6.473.A Case of Community-Acquired Pneumonia Caused by Multidrug-Resistant Acinetobacter baumannii in Korea
Young Woong Son, In Young Jung, Mi Young Ahn, Yong Duk Jeon, Hea Won Ann, Jin Young Ahn, Nam Su Ku, Sang Hoon Han, Jun Young Choi, Young Goo Song, June Myung Kim
Infect Chemother. 2017;49(4):297-300. doi: 10.3947/ic.2017.49.4.297.
Reference
-
1. Enoch DA, Summers C, Brown NM, Moore L, Gillham MI, Burnstein RM, Thaxter R, Enoch LM, Matta B, Sule O. Investigation and management of an outbreak of multidrug-carbapenem-resistant Acinetobacter baumannii in Cambridge, UK. J Hosp Infect. 2008. 70:109–118.
Article2. Lima AL, Oliveira PR, Paula AP. Acinetobacter infection. N Engl J Med. 2008. 358:2846. author reply 2846-7.
Article3. Ong CW, Lye DC, Khoo KL, Chua GS, Yeoh SF, Leo YS, Tambyah PA, Chua AC. Severe community-acquired Acinetobacter baumannii pneumonia: an emerging highly lethal infectious disease in the Asia-Pacific. Respirology. 2009. 14:1200–1205.
Article4. Falagas ME, Karveli EA, Kelesidis I, Kelesidis T. Community-acquired Acinetobacter infections. Eur J Clin Microbiol Infect Dis. 2007. 26:857–868.5. Han SH, Na DJ, Yoo YW, Kim DG, Moon YR, Moon KM, Lee YD, Cho YS, Han MS, Yoon HJ. A case of probable community acquired Acinetobacter baumannii pneumonia. Tuberc Respir Dis. 2007. 63:273–277.
Article6. Kang CI, Song JH, Oh WS, Ko KS, Chung DR, Peck KR. Asian Network for Surveillance of Resistant Pathogens (ANSORP) Study Group. Clinical outcomes and risk factors of community-acquired pneumonia caused by gram-negative bacilli. Eur J Clin Microbiol Infect Dis. 2008. 27:657–661.
Article7. Na JY, Min BW, Chung SH, Kim MY, Lee YJ, Park JT, Kim HS. A probable community-acquired pneumonia due to Acinetobacter baumannii infection presenting the positive pneumothorax test at autopsy. Korean J Leg Med. 2010. 34:125–128.8. Lolans K, Rice TW, Munoz-Price LS, Quinn JP. Multicity outbreak of carbapenem-resistant Acinetobacter baumannii isolates producing the carbapenemase OXA-40. Antimicrob Agents Chemother. 2006. 50:2941–2945.
Article9. Forster DH, Daschner FD. Acinetobacter species as nosocomial pathogens. Eur J Clin Microbiol Infect Dis. 1998. 17:73–77.
Article10. Chen MZ, Hsueh PR, Lee LN, Yu CJ, Yang PC, Luh KT. Severe community-acquired pneumonia due to Acinetobacter baumannii. Chest. 2001. 120:1072–1077.
Article11. Yang CH, Chen KJ, Wang CK. Community-acquired Acinetobacter pneumonia: a case report. J Infect. 1997. 35:316–318.12. Kanemoto K, Ogawa R, Kurishima K, Ishikawa H, Ohtsuka M, Sekizawa K. Severe community-acquired Acinetobacter pneumonia. Nihon Kokyuki Gakkai Zasshi. 2003. 41:817–821.13. Koshimizu N, Sato M, Gemma H, Uemura K, Chida K. An autopsy case of fulminant community-acquired pneumonia due to Acinetobacter baumannii. Kansenshogaku Zasshi. 2009. 83:392–397.
Article14. Leung WS, Chu CM, Tsang KY, Lo FH, Lo KF, Ho PL. Fulminant community-acquired Acinetobacter baumannii pneumonia as a distinct clinical syndrome. Chest. 2006. 129:102–109.
Article15. Anstey NM, Currie BJ, Hassell M, Palmer D, Dwyer B, Seifert H. Community-acquired bacteremic Acinetobacter pneumonia in tropical Australia is caused by diverse strains of Acinetobacter baumannii, with carriage in the throat in atrisk groups. J Clin Microbiol. 2002. 40:685–686.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of fulminant community-acquired Acinetobacter baumannii pneumonia in Korea
- A Case of Infective Endocarditis Caused by Community-Acquired Acinetobacter baumannii
- A Case of Community-Acquired Pneumonia Caused by Multidrug-Resistant Acinetobacter baumannii in Korea
- A Case of Probable Community Acquired Acinetobacter baumannii Pneumonia
- A Probable Community-Acquired Pneumonia due to Acinetobacter baumannii Infection Presenting the Positive Pneumothorax Test at Autopsy