Tuberc Respir Dis.
2014 Nov;77(5):223-226. 10.4046/trd.2014.77.5.223.
Aspergillus Tracheobronchitis in a Mild Immunocompromised Host
- Affiliations
-
- 1Department of Internal Medicine, Chungbuk National University College of Medicine, Cheongju, Korea. drahnjy@chungbuk.ac.kr
- 2Department of Pathology, Chungbuk National University College of Medicine, Cheongju, Korea.
- KMID: 2050716
- DOI: http://doi.org/10.4046/trd.2014.77.5.223
Abstract
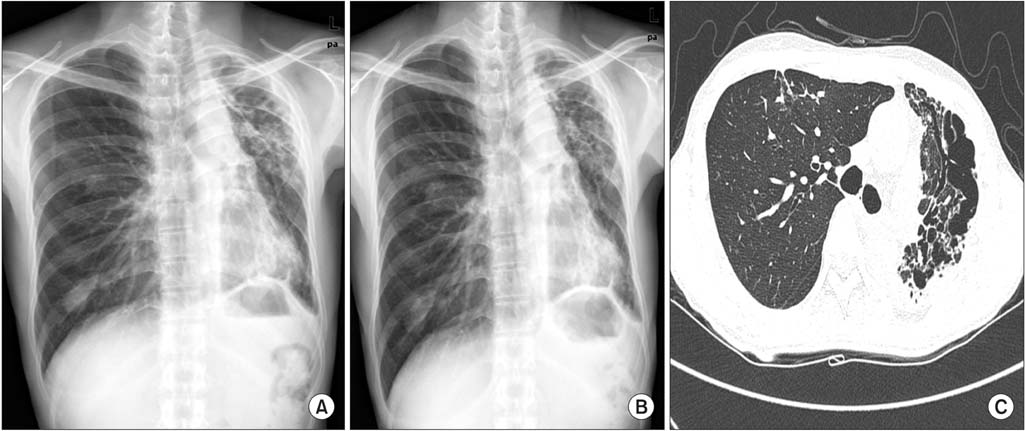
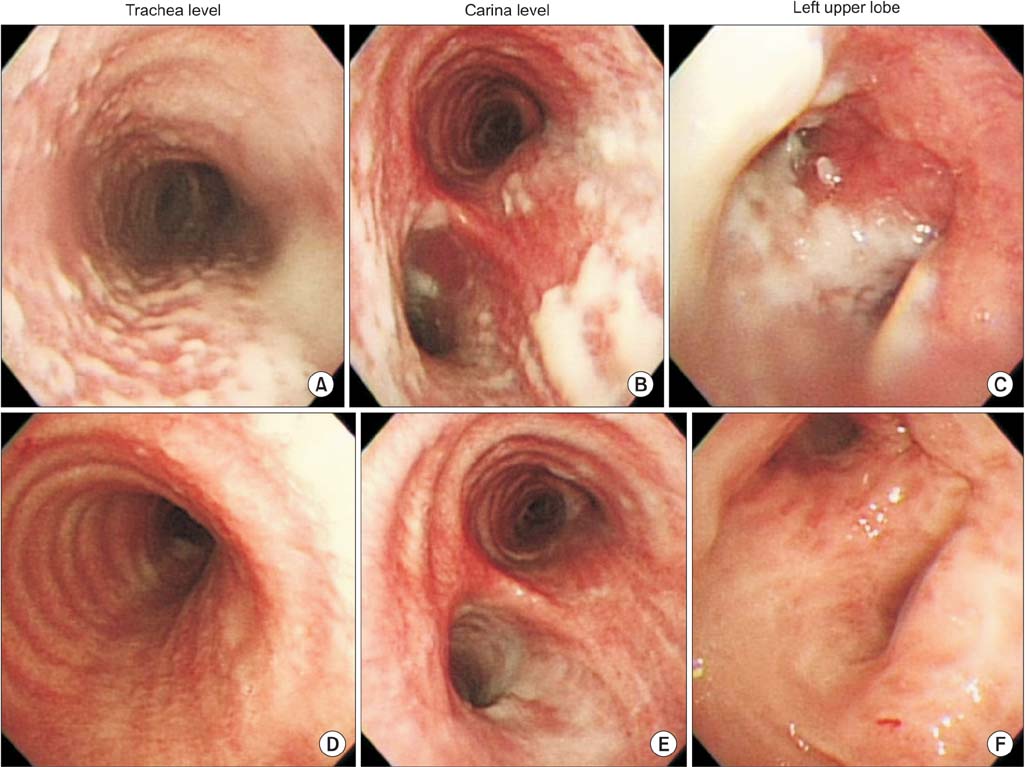
- Aspergillus tracheobronchitis is a form of invasive pulmonary aspergillosis in which the Aspergillus infection is limited predominantly to the tracheobronchial tree. It occurs primarily in severely immunocompromised patients such as lung transplant recipients. Here, we report a case of Aspergillus tracheobronchitis in a 42-year-old man with diabetes mellitus, who presented with intractable cough, lack of expectoration of sputum, and chest discomfort. The patient did not respond to conventional treatment with antibiotics and antitussive agents, and he underwent bronchoscopy that showed multiple, discrete, gelatinous whitish plaques mainly involving the trachea and the left bronchus. On the basis of the bronchoscopic and microbiologic findings, we made the diagnosis of Aspergillus tracheobronchitis and initiated antifungal therapy. He showed gradual improvement in his symptoms and continued taking oral itraconazole for 6 months. Physicians should consider Aspergillus tracheobronchitis as a probable diagnosis in immunocompromised patients presenting with atypical respiratory symptoms and should try to establish a prompt diagnosis.
MeSH Terms
-
Adult
Anti-Bacterial Agents
Antitussive Agents
Aspergillosis, Allergic Bronchopulmonary
Aspergillus*
Bronchi
Bronchoscopy
Cough
Diabetes Mellitus
Diagnosis
Gelatin
Humans
Immunocompromised Host*
Invasive Pulmonary Aspergillosis
Itraconazole
Lung
Sputum
Thorax
Trachea
Transplantation
Anti-Bacterial Agents
Antitussive Agents
Gelatin
Itraconazole
Figure
Reference
-
1. Kemper CA, Hostetler JS, Follansbee SE, Ruane P, Covington D, Leong SS, et al. Ulcerative and plaque-like tracheobronchitis due to infection with Aspergillus in patients with AIDS. Clin Infect Dis. 1993; 17:344–352.2. Wheaton SW. Case primarily of tubercle, in which a fungus (Aspergillus) grew in the bronchi and lung, simulating actinomycosis. Trans Pathol Soc Lond. 1890; 41:34–37.3. Soubani AO, Chandrasekar PH. The clinical spectrum of pulmonary aspergillosis. Chest. 2002; 121:1988–1999.4. Boots RJ, Paterson DL, Allworth AM, Faoagali JL. Successful treatment of post-influenza pseudomembranous necrotising bronchial aspergillosis with liposomal amphotericin, inhaled amphotericin B, gamma interferon and GM-CSF. Thorax. 1999; 54:1047–1049.5. Franco J, Munoz C, Vila B, Marin J. Pseudomembranous invasive tracheobronchial aspergillosis. Thorax. 2004; 59:452.6. Lee SE, Jun EJ, Song JH, Shin JW, Kim JY, Park IW, et al. A case of pseudomembranous necrotizing bronchial aspergillosis in an old age host. Tuberc Respir Dis. 2007; 63:278–282.7. Chang SM, Kuo HT, Lin FJ, Tzen CY, Sheu CY. Pseudomembranous tracheobronchitis caused by Aspergillus in immunocompromised patients. Scand J Infect Dis. 2005; 37:937–942.8. Wu N, Huang Y, Li Q, Bai C, Huang HD, Yao XP. Isolated invasive Aspergillus tracheobronchitis: a clinical study of 19 cases. Clin Microbiol Infect. 2010; 16:689–695.9. Kousha M, Tadi R, Soubani AO. Pulmonary aspergillosis: a clinical review. Eur Respir Rev. 2011; 20:156–174.10. Segal BH, Walsh TJ. Current approaches to diagnosis and treatment of invasive aspergillosis. Am J Respir Crit Care Med. 2006; 173:707–717.11. Tasci S, Glasmacher A, Lentini S, Tschubel K, Ewig S, Molitor E, et al. Pseudomembranous and obstructive Aspergillus tracheobronchitis: optimal diagnostic strategy and outcome. Mycoses. 2006; 49:37–42.12. Kramer MR, Denning DW, Marshall SE, Ross DJ, Berry G, Lewiston NJ, et al. Ulcerative tracheobronchitis after lung transplantation. A new form of invasive aspergillosis. Am Rev Respir Dis. 1991; 144(3 Pt 1):552–556.13. Walsh TJ, Anaissie EJ, Denning DW, Herbrecht R, Kontoyiannis DP, Marr KA, et al. Treatment of aspergillosis: clinical practice guidelines of the Infectious Diseases Society of America. Clin Infect Dis. 2008; 46:327–360.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Death due to Aspergillus Tracheobronchitis: An Autopsy Case
- Airway Obstruction and Respiratory Failure Due to Aspergillus Tracheobronchitis
- Pseudomembranous Aspergillus Tracheobronchitis in an Immunocompetent Patient
- A Case of Pseudomembranous Necrotizing Bronchial Aspergillosis in An Old Age Host
- A Case of Pseudomembranous Aspergillus Tracheobronchitis in a Patient with Diabetes Mellitus