Dement Neurocogn Disord.
2014 Mar;13(1):24-26. 10.12779/dnd.2014.13.1.24.
Marchiafava Bignami Disease Potentially Complicating Normal Pressure Hydrocephalus
- Affiliations
-
- 1Department of Neurology, Sanbon Medical Center, College of Medicine, Wonkwang University, Gunpo, Korea. hyundyang@gmail.com
- 2Department of Neurosurgery, Sanbon Medical Center, College of Medicine, Wonkwang University, Gunpo, Korea.
- KMID: 1973687
- DOI: http://doi.org/10.12779/dnd.2014.13.1.24
Abstract
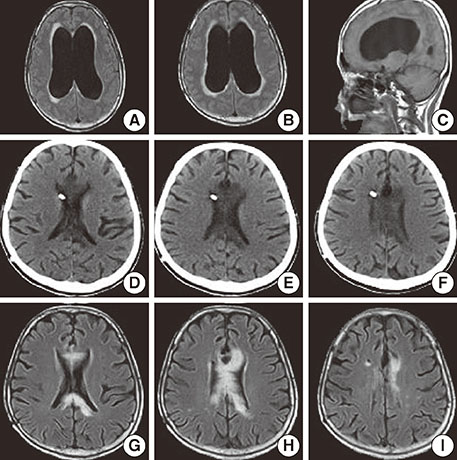
- Marchiafava-Bignami disease (MBD) is a rare disorder of demyelination or necrosis of the corpus callosum. Mainly, MBD is associated with alcohol and malnutrition. We report a 60-year-old woman with no history of alcohol consumption or malnutrition who had MBD as a possible complication of normal pressure hydrocephalus (NPH). The patient presented with a 2-month history of progressive gait unsteadiness, urinary incontinence, and forgetfulness, for which the patient underwent ventriculoperitoneal shunt surgery with remarkable improvement. Magnetic resonance imaging (MRI) demonstrated hyperintensity in the body and splenium of corpus callosum when she was brought to the hospital again with rapid deterioration of her mental ststus. It might be postulated that cerebrospinal fluid (CSF) tumor necrosis factor-alpha (TNF-alpha) might have contributed to the development of MBD although not measured in this patient, given that TNF-alpha, as a proinflammatory cytokine mediating demyelinating process have been found in be increased in the CSF of NPH.
MeSH Terms
-
Alcohol Drinking
Cerebrospinal Fluid
Corpus Callosum
Demyelinating Diseases
Female
Gait
Humans
Hydrocephalus, Normal Pressure*
Magnetic Resonance Imaging
Malnutrition
Marchiafava-Bignami Disease*
Middle Aged
Necrosis
Negotiating
Tumor Necrosis Factor-alpha
Urinary Incontinence
Ventriculoperitoneal Shunt
Tumor Necrosis Factor-alpha
Figure
Reference
-
1. Factora R, Luciano M. Normal pressure hydrocephalus: diagnosis and new approaches to treatment. Clin Geriatr Med. 2006; 22:645–657.
Article2. Hebb AO, Cusimano MD. Idiopathic normal pressure hydrocephalus: a systematic review of diagnosis and outcome. Neurosurgery. 2001; 49:1166–1184. discussion 1184-66.
Article3. Castaigne P, Buge A, Cambier J, Escourolle R, Rancurel G. [Marchiafava-Bignami disease: anatomoclinical study of 2 cases]. Rev Neurol (Paris). 1971; 125:179–196.4. Heinrich A, Runge U, Khaw AV. Clinicoradiologic subtypes of Marchiafava-Bignami disease. J Neurol. 2004; 251:1050–1059.
Article5. Suzuki Y, Oishi M, Ogawa K, Kamei S. A patient with Marchiafava-Bignami disease as a complication of diabetes mellitus treated effectively with cortico steroid. J Clin Neurosci. 2012; 19:761–762.
Article6. Tarkowski E, Tullberg M, Fredman P, Wikkelsö C. Normal pressure hydrocephalus triggers intrathecal production of TNF-alpha. Neurobiol Aging. 2003; 24:707–714.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Marchiafava-Bignami Disease in Crohn's Disease
- Cortical Involvement of Marchiafava-Bignami Disease: A Case Report
- A Case of Reversible Marchiafava-Bignami Disease Showing Severe Thalamic Hypometabolism in PET
- Callosal and Cortical Involvement in Acute Marchiafava-Bignami Disease
- Two cases of Marchiafava-Bignami disease in alcoholics