Tuberc Respir Dis.
2006 Nov;61(5):479-483. 10.4046/trd.2006.61.5.479.
A Case of Acute Fibrinous and Organizing Pneumonia
- Affiliations
-
- 1Department of Internal Medicine, Inje University., Sooul, Korea. pulho@korea.com
- 2Department of Pathology, Inje University., Sooul, Korea.
- KMID: 1970254
- DOI: http://doi.org/10.4046/trd.2006.61.5.479
Abstract
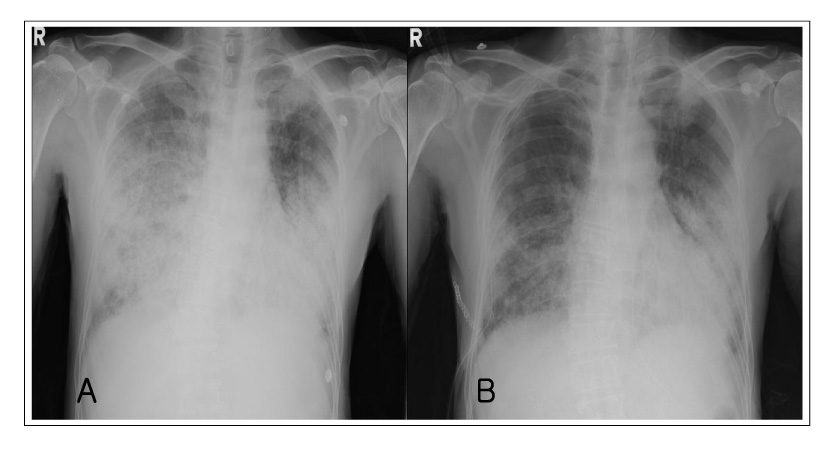
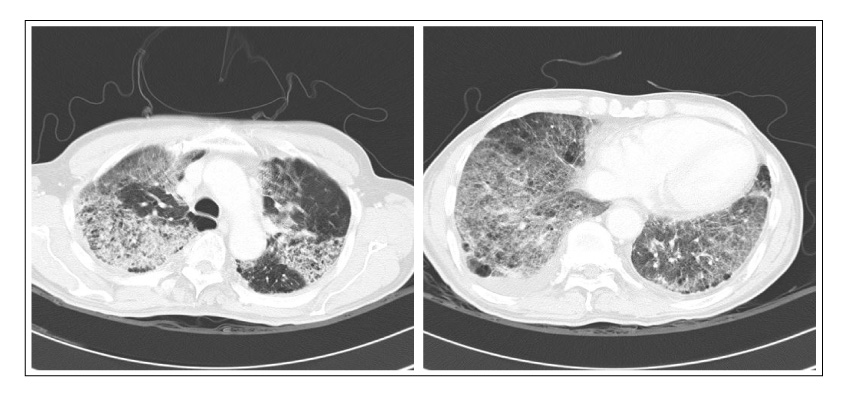
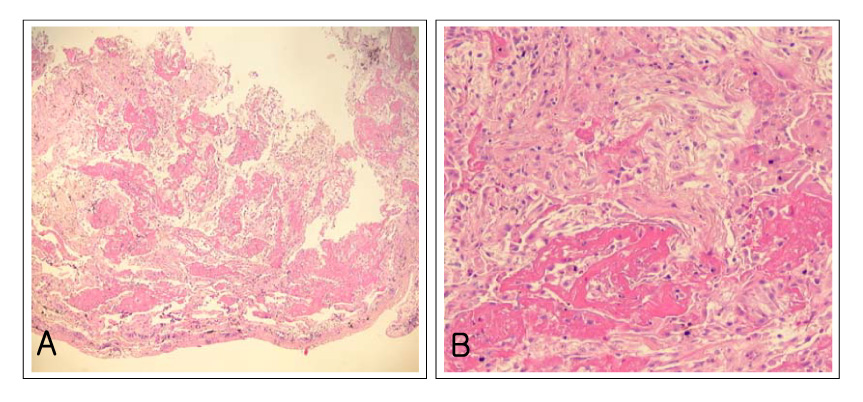
- Acute fibrinous and organizing pneumonia (AFOP) is a histological pattern consisting of prominent intra-alveolar fibrin and organizing pneumonia, with out hyaline membranes or prominent eosinophilia. The clinical manifestations of AFOP resemble those of acute lung injury such as acute interstitial pneumonia (AIP). However, the classic histological patterns of AFOP differ from diffuse alveolar damage (DAD), bronchiolitis obliterans with organizing pneumonia (BOOP) or acute eosinophilic pneumonia (AEP). The characteristic intra-alveolar fibrin ball and lack of classic hyaline membrane are the predominant histological features of AFOP. Although some reports suggest that its clinical course is less catastrophic than DAD, the clinical entity that distinguishes AFOP from DAD has not been established. We present a case of pathologically demonstrated AFOP in a 79-year-old man. The radiological findings of our case were similar to those of DAD, presented with diffuse bilateral lung infiltrations. However, despite the rapid development of respiratory failure, the patient had a better response and outcome to steroid therapy than what would be expected for DAD.
Keyword
MeSH Terms
Figure
Reference
-
1. Beasly MB, Franks TJ, Galvin JR, Gochuico B, Travis WD. Acute fibrous and organizing pneumonia. Arch Pathol Lab Med. 2002. 126:1064–1070.2. American Thoracic Society and European Respiratody Society. American Thoracic Society/European Respiratory Society International Multidisciplinary Consensus Classification of the Idiopathic Interstitial Pneumonias. Am J Respir Crit Care Med. 2002. 165:277–304.3. Vourlekis JS, Brown KK, Schwart MI. Acute interstitial pneumonitis: current understanding regarding diagnosis, pathogenesis, and natural history. Semin Respir Crit Care Med. 2001. 22:399–408.4. Yazdy AM, Tomashefski JF Jr, Yagan R, Kleinerman J. Regional alveolar damage (RAD): a localized counterpart of diffuse alveolar damage. Am J Clin Pathol. 1989. 92:10–15.5. Lamy M, Fallat RJ, Koeniger E, Dietrich HP, Ratliff JL, Eberhart RC, et al. Pathologic features and mechanisms of hypoxemia in adult respiratory distress syndrome. Am Rev Respir Dis. 1976. 114:267–284.6. Tomashefski JF Jr. Pulmonary pathology of the adult respiratory distress syndrome. Clin Chest Med. 1990. 11:593–619.7. Tazelaar HD, Linz LJ, Colby TV, Myers JL, Limper AH. Acute eosinophilic pneumonia: histopathologic findings in nine patients. Am J Respir Crit Care Med. 1997. 155:296–302.8. Muller NL, Guerry-Force ML, Staples CA, Wright JL, Wiggs B, Coppin C, et al. Differential diagnosis of bronchiolitis obliterans with organizing pneumonia and usual interstitial pneumonia: clinical, functional, and radiologic findings. Radiology. 1987. 162:151–156.9. Savici D, Katzenstein AL. Diffuse alveolar damage and recurrent respiratory failure: report of six cases. Hum Pathol. 2001. 32:1398–1402.10. Vourlekis JS, Brown KK, Schwarz MI. Acute interstitial pneumonitis: current understanding regarding diagnosis, pathogenesis, and natural history. Semin Respir Crit Care Med. 2001. 22:399–408.11. Muller NL, Colby TV. Idiopathic interstitial pneumonias: high-resolution CT and histologic findings. Radiographics. 1997. 17:1016–1022.12. Katzenstein AL, Myers JL, Mazur MT. Acute interstitial pneumonia: a clinico-pathologic, ultrastructural, and cell kinetic study. Am J Surg Pathol. 1986. 10:256–267.13. Bouros D, Nicholson AC, Polychronopoulos V, du Bois RM. Acute interstitial pneumonia. Eur Respir J. 2000. 15:412–418.14. Kobayshi H, Itoh T, Sasaki Y, Konishi J. Diagnostic imaging of idiopathic adult respiratory distress syndrome (ARDS)/ diffuse alveolar damage (DAD): histopathological correlation with radiological imaging. Clin Imaging. 1996. 20:1–7.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two cases of acute fibrinous and organizing pneumonia
- Acute Fibrinous and Organizing Pneumonia Following Hematopoietic Stem Cell Transplantation
- A Case of Spontaneous Remission Organizing Pneumonia after Resection of Thymoma
- A Case of Secondary Organizing Pneumonia Associated with Endobronchial Actinomycosis
- Severe Acute Fibrinous and Organizing Pneumonia with Acute Respiratory Distress Syndrome