Tuberc Respir Dis.
2007 Mar;62(3):227-231. 10.4046/trd.2007.62.3.227.
A Case of Secondary Organizing Pneumonia Associated with Endobronchial Actinomycosis
- Affiliations
-
- 1Department of Internal Medicine, Eulji General Hospital, Eulji University School of Medicine, Seoul, Korea. ksh1134@eulji.or.kr
- 2Department of Radiology, Eulji General Hospital, Eulji University School of Medicine, Seoul, Korea.
- KMID: 1518469
- DOI: http://doi.org/10.4046/trd.2007.62.3.227
Abstract
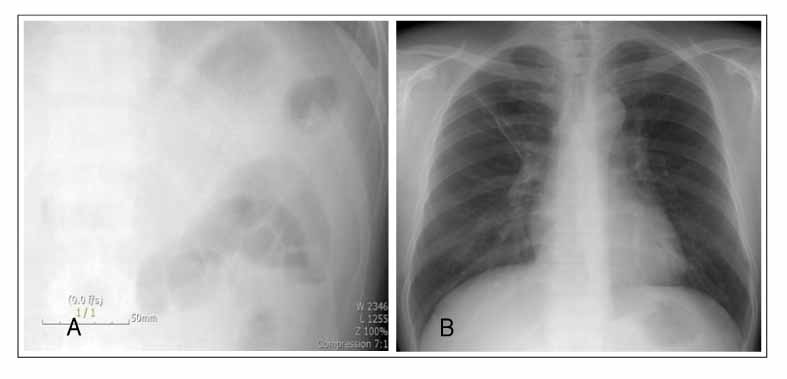
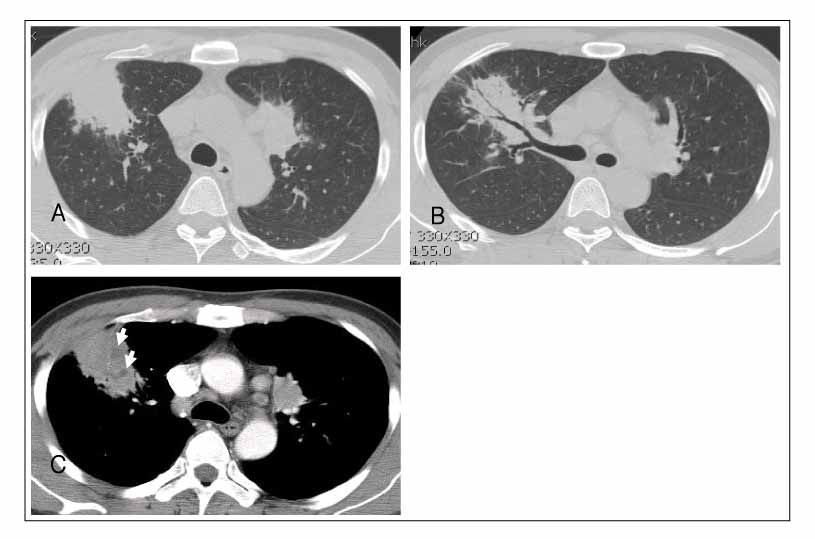
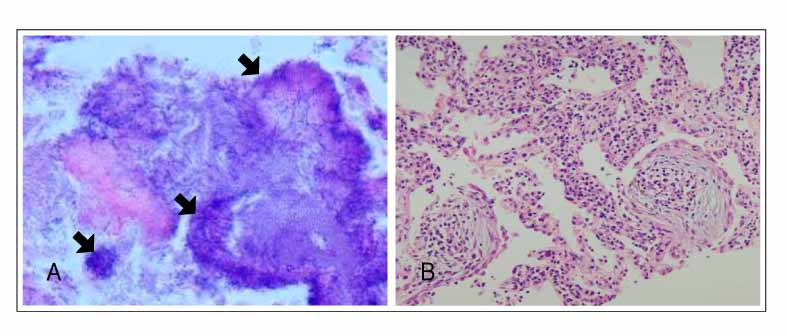
- Several types of infection can cause organizing pneumonia when the inflammatory process remains active with the further organization of the intra-alveolar fibrinous exudates, despite the control of the infectious organism by antibiotics. We report a case of 37-year-old male with secondary organizing pneumonia associated with an endobronchial actinomycosis. The patient presented with a subacute cough, sputum and fever. Bronchial biopsy revealed sulfur granule to be consistent with the actinomycosis, and percutaneous needle biopsy revealed typical pattern of organizing pneumonia. The patient was treated with the appropriate antibiotics and corticosteroid. There was rapid improvement in the symptoms and radiological findings, and after six months of treatment, the corticosteroid dose was tapered off without a recurrence of the organizing pneumonia.
MeSH Terms
Figure
Reference
-
1. Colby TV. Pathologic aspects of bronchiolitis obliterans organizing pneumonia. Chest. 1992. 102:38S–43S.2. Sulavik SB. The concept of "organizing pneumonia". Chest. 1989. 96:967–969.3. Cordier JF. Organising pneumonia. Thorax. 2000. 55:318–328.4. Lohr RH, Boland BJ, Douglas WW, Dockrell DH, Colby TV, Swensen SJ, et al. Organizing pneumonia: features and prognosis of cryptogenic, secondary, and focal variants. Arch Intern Med. 1997. 157:1323–1329.5. Epler GR, Colby TV, McLoud TC, Carrington CB, Gaensler EA. Bronchiolitis obliterans organizing pneumonia. N Engl J Med. 1985. 312:152–158.6. American Thoracic Society and European Respiratory Society. Americaan Thoracic Society/European Respiratory Society International Multidisciplinary Consensus Classification of the Idiopathic Interstitial Pneumonias. Am J Respir Crit Care Med. 2002. 165:277–304.7. Schlesinger C, Koss MN. The organizing pneumonias: an update and review. Curr Opin Pulm Med. 2005. 11:422–430.8. Miwa S, Morita S, Suda T, Suzuki K, Hayakawa H, Chida K, et al. The incidence and clinical characteristics of bronchiolitis obliterans organizing pneumonia syndrome after radiation therapy for breast cancer. Sarcoidosis Vasc Diffuse Lung Dis. 2004. 21:212–218.9. Han SK, Yim JJ, Lee JH, Yoo CG, Chung HS, Shim YS, et al. Bronchiolitis obliterans organizing pneumonia in Korea. Respirology. 1998. 3:187–191.10. Chang J, Han J, Kim DW, Lee I, Lee KY, Jung S, et al. Bronchiolitis obliterans organizing pneumonia: clinicopathologic review of a series of 45 Korean patients including rapidly progressive form. J Korean Med Sci. 2002. 17:179–186.11. Camp M, Mehta JB, Whitson M. Bronchiolitis obliterans and Nocardia asteroides infection of the lung. Chest. 1987. 92:1107–1108.12. Cordier JF. Cryptogenic organising pneumonia. Eur Respir J. 2006. 28:422–446.13. Mabeza GF, Macfarlane J. Pulmonary actinomycosis. Eur Respir J. 2003. 21:545–551.14. Slade PR, Slesser BV, Southgate J. Thoracic actinomycosis. Thorax. 1973. 28:73–85.15. Choi JC, Koh W, Kwon YS, Rhy YJ, Yu C, Jeon K, et al. Diagnosis and treatment of endobronchial actinomycosis. Tuberc Respir Dis. 2005. 58:576–581.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Endobronchial Actinomycosis with a Broncholith cured by Cryotherapy through a Flexible Bronchoscope
- A Case of Spontaneous Remission Organizing Pneumonia after Resection of Thymoma
- A Case of Endobronchial Actinomycosis
- Endobronchial actinomycosis simulating endobronchial tuberculosis: a case report
- A Case of Primary Endobronchial Actinomycosis Presenting as a Complicated Parapneumonic Effusion