J Periodontal Implant Sci.
2011 Jun;41(3):135-142. 10.5051/jpis.2011.41.3.135.
Effect of erbium-doped: yttrium, aluminium and garnet laser irradiation on the surface microstructure and roughness of sand-blasted, large grit, acid-etched implants
- Affiliations
-
- 1Department of Periodontology, Kyung Hee University School of Dentistry, Seoul, Korea. chungjh@khu.ac.kr
- 2Department of Periodontology and Institute of Oral Biology, Kyung Hee University School of Dentistry, Seoul, Korea.
- KMID: 1783604
- DOI: http://doi.org/10.5051/jpis.2011.41.3.135
Abstract
- PURPOSE
The present study was performed to evaluate the effect of erbium-doped: yttrium, aluminium and garnet (Er:YAG) laser irradiation on sand-blasted, large grit, acid-etched (SLA) implant surface microstructure according to varying energy levels and application times of the laser.
METHODS
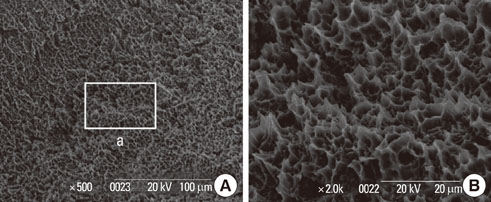
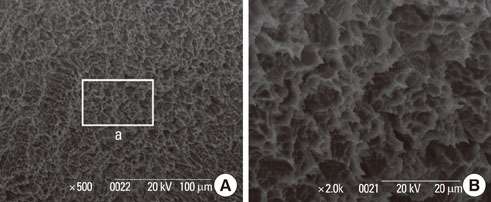
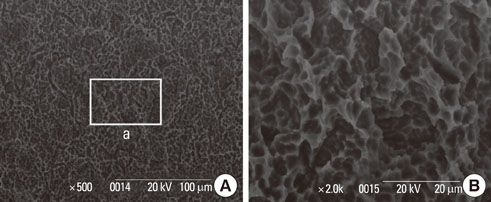
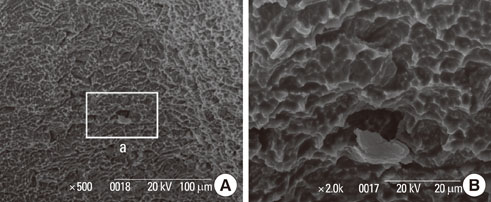
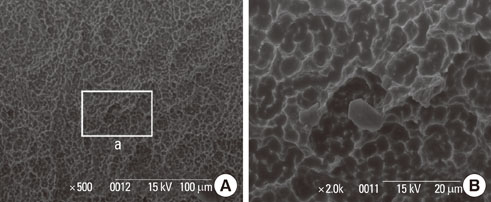
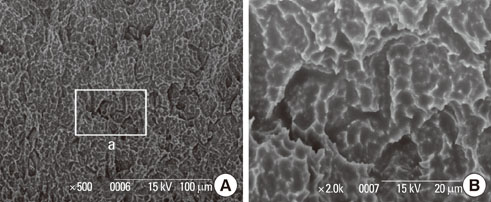
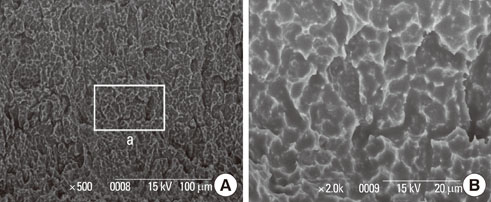
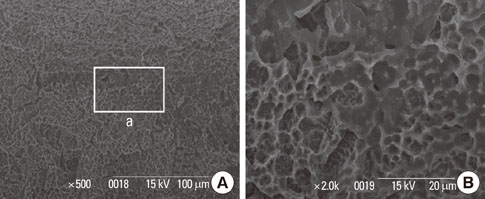
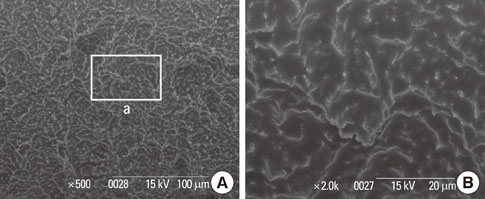
The implant surface was irradiated by the Er:YAG laser under combined conditions of 100, 140, or 180 mJ/pulse and an application time of 1 minute, 1.5 minutes, or 2 minutes. Scanning electron microscopy (SEM) was used to examine the surface roughness of the specimens.
RESULTS
All experimental conditions of Er:YAG laser irradiation, except the power setting of 100 mJ/pulse for 1 minute and 1.5 minutes, led to an alteration in the implant surface. SEM evaluation showed a decrease in the surface roughness of the implants. However, the difference was not statistically significant. Alterations of implant surfaces included meltdown and flattening. More extensive alterations were present with increasing laser energy and application time.
CONCLUSIONS
To ensure no damage to their surfaces, it is recommended that SLA implants be irradiated with an Er:YAG laser below 100 mJ/pulse and 1.5 minutes for detoxifying the implant surfaces.
Keyword
MeSH Terms
Figure
Reference
-
1. el Askary AS, Meffert RM, Griffin T. Why do dental implants fail? Part I. Implant Dent. 1999. 8:173–185.
Article2. Lindhe J, Meyle J. Group D of European Workshop on Periodontology. Peri-implant diseases: Consensus Report of the Sixth European Workshop on Periodontology. J Clin Periodontol. 2008. 35:8 Suppl. 282–285.
Article3. Heitz-Mayfield LJ. Peri-implant diseases: diagnosis and risk indicators. J Clin Periodontol. 2008. 35:8 Suppl. 292–304.
Article4. Mombelli A, Buser D, Lang NP. Colonization of osseointegrated titanium implants in edentulous patients. Early results. Oral Microbiol Immunol. 1988. 3:113–120.
Article5. Albrektsson T, Isidor F. Lang NP, Karring T, editors. Consensus report of session IV. Proceeding of the 1st European Workshop on Periodontology. 1994. London: Quintessence Books;365–369.6. Esposito M, Thomsen P, Ericson LE, Lekholm U. Histopathologic observations on early oral implant failures. Int J Oral Maxillofac Implants. 1999. 14:798–810.7. Mombelli A. Microbiology and antimicrobial therapy of peri-implantitis. Periodontol 2000. 2002. 28:177–189.
Article8. Meffert RM, Langer B, Fritz ME. Dental implants: a review. J Periodontol. 1992. 63:859–870.
Article9. Zablotsky MH, Diedrich DL, Meffert RM. Detoxification of endotoxin-contaminated titanium and hydroxyapatite-coated surfaces utilizing various chemotherapeutic and mechanical modalities. Implant Dent. 1992. 1:154–158.
Article10. Krozer A, Hall J, Ericsson I. Chemical treatment of machined titanium surfaces. An in vitro study. Clin Oral Implants Res. 1999. 10:204–211.
Article11. Kreisler M, Götz H, Duschner H. Effect of Nd:YAG, Ho:YAG, Er:YAG, CO2, and GaAIAs laser irradiation on surface properties of endosseous dental implants. Int J Oral Maxillofac Implants. 2002. 17:202–211.12. Augthun M, Tinschert J, Huber A. In vitro studies on the effect of cleaning methods on different implant surfaces. J Periodontol. 1998. 69:857–864.
Article13. Van de Velde E, Thielens P, Schautteet H, Vanclooster R. Subcutaneous emphysema of the oral floor during cleaning of a bridge fixed on an IMZ implant. Case report. Rev Belge Med Dent (1984). 1991. 46:64–71.14. Thomson-Neal DM, Evans GH, Meffert RM. Effects of various prophylactic treatments on titanium, sapphire, and hydroxyapatite-coated implants: An SEM study. Int J Periodontics Restorative Dent. 1989. 9:300–311.15. Fox SC, Moriarty JD, Kusy RP. The effects of scaling a titanium implant surface with metal and plastic instruments: an in vitro study. J Periodontol. 1990. 61:485–490.
Article16. Mouhyi J, Sennerby L, Pireaux JJ, Dourov N, Nammour S, Van Reck J. An XPS and SEM evaluation of six chemical and physical techniques for cleaning of contaminated titanium implants. Clin Oral Implants Res. 1998. 9:185–194.
Article17. Kato T, Kusakari H, Hoshino E. Bactericidal efficacy of carbon dioxide laser against bacteria-contaminated titanium implant and subsequent cellular adhesion to irradiated area. Lasers Surg Med. 1998. 23:299–309.
Article18. Kreisler M, Al Haj H, Götz H, Duschner H, d'Hoedt B. Effect of simulated CO2 and GaAlAs laser surface decontamination on temperature changes in Ti-plasma sprayed dental implants. Lasers Surg Med. 2002. 30:233–239.
Article19. Romanos GE, Everts H, Nentwig GH. Effects of diode and Nd:YAG laser irradiation on titanium discs: a scanning electron microscope examination. J Periodontol. 2000. 71:810–815.
Article20. Dörtbudak O, Haas R, Bernhart T, Mailath-Pokorny G. Lethal photosensitization for decontamination of implant surfaces in the treatment of peri-implantitis. Clin Oral Implants Res. 2001. 12:104–108.
Article21. Kreisler M, Al Haj H, D'Hoedt B. Temperature changes induced by 809-nm GaAlAs laser at the implant-bone interface during simulated surface decontamination. Clin Oral Implants Res. 2003. 14:91–96.
Article22. Block CM, Mayo JA, Evans GH. Effects of the Nd:YAG dental laser on plasma-sprayed and hydroxyapatite-coated titanium dental implants: surface alteration and attempted sterilization. Int J Oral Maxillofac Implants. 1992. 7:441–449.23. Kreisler M, Kohnen W, Marinello C, Götz H, Duschner H, Jansen B, et al. Bactericidal effect of the Er:YAG laser on dental implant surfaces: an in vitro study. J Periodontol. 2002. 73:1292–1298.
Article24. Friedmann A, Antic L, Bernimoulin JP, Purucker P. In vitro attachment of osteoblasts on contaminated rough titanium surfaces treated by Er:YAG laser. J Biomed Mater Res A. 2006. 79:53–60.
Article25. Eberhard J, Ehlers H, Falk W, Açil Y, Albers HK, Jepsen S. Efficacy of subgingival calculus removal with Er:YAG laser compared to mechanical debridement: an in situ study. J Clin Periodontol. 2003. 30:511–518.
Article26. Schwarz F, Sculean A, Berakdar M, Szathmari L, Georg T, Becker J. In vivo and in vitro effects of an Er:YAG laser, a GaAlAs diode laser, and scaling and root planing on periodontally diseased root surfaces: a comparative histologic study. Lasers Surg Med. 2003. 32:359–366.
Article27. Schwarz F, Sculean A, Berakdar M, Georg T, Reich E, Becker J. Clinical evaluation of an Er:YAG laser combined with scaling and root planing for non-surgical periodontal treatment. A controlled, prospective clinical study. J Clin Periodontol. 2003. 30:26–34.
Article28. Schwarz F, Sculean A, Berakdar M, Georg T, Reich E, Becker J. Periodontal treatment with an Er:YAG laser or scaling and root planing. A 2-year follow-up split-mouth study. J Periodontol. 2003. 74:590–596.
Article29. Schwarz F, Sculean A, Georg T, Reich E. Periodontal treatment with an Er: YAG laser compared to scaling and root planing. A controlled clinical study. J Periodontol. 2001. 72:361–367.
Article30. Schwarz F, Rothamel D, Sculean A, Georg T, Scherbaum W, Becker J. Effects of an Er:YAG laser and the Vector ultrasonic system on the biocompatibility of titanium implants in cultures of human osteoblast-like cells. Clin Oral Implants Res. 2003. 14:784–792.
Article31. Fransson C, Lekholm U, Jemt T, Berglundh T. Prevalence of subjects with progressive bone loss at implants. Clin Oral Implants Res. 2005. 16:440–446.
Article32. Roos-Jansåker AM, Renvert H, Lindahl C, Renvert S. Nine-to fourteen-year follow-up of implant treatment. Part III: factors associated with peri-implant lesions. J Clin Periodontol. 2006. 33:296–301.
Article33. Rimondini L, Farè S, Brambilla E, Felloni A, Consonni C, Brossa F, et al. The effect of surface roughness on early in vivo plaque colonization on titanium. J Periodontol. 1997. 68:556–562.
Article34. Eriksson AR, Albrektsson T. Temperature threshold levels for heat-induced bone tissue injury: a vital-microscopic study in the rabbit. J Prosthet Dent. 1983. 50:101–107.
Article35. Kreisler M, Al Haj H, d'Hoedt B. Temperature changes at the implant-bone interface during simulated surface decontamination with an Er:YAG laser. Int J Prosthodont. 2002. 15:582–587.36. Schwarz F, Sculean A, Romanos G, Herten M, Horn N, Scherbaum W, et al. Influence of different treatment approaches on the removal of early plaque biofilms and the viability of SAOS2 osteoblasts grown on titanium implants. Clin Oral Investig. 2005. 9:111–117.
Article37. Sammons RL, Lumbikanonda N, Gross M, Cantzler P. Comparison of osteoblast spreading on microstructured dental implant surfaces and cell behaviour in an explant model of osseointegration. A scanning electron microscopic study. Clin Oral Implants Res. 2005. 16:657–666.
Article38. Wennerberg A, Albrektsson T. Suggested guidelines for the topographic evaluation of implant surfaces. Int J Oral Maxillofac Implants. 2000. 15:331–344.39. Albrektsson T, Wennerberg A. Oral implant surfaces: Part 1: review focusing on topographic and chemical properties of different surfaces and in vivo responses to them. Int J Prosthodont. 2004. 17:536–543.40. Wennerberg A, Albrektsson T. Effects of titanium surface topography on bone integration: a systematic review. Clin Oral Implants Res. 2009. 20:Suppl 4. 172–184.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The effect of erbium-doped: yttrium, aluminium and garnet laser irradiation on the surface microstructure and roughness of double acid-etched implants
- Scanning Electron Microscopic Study of the Effects of Citric Acid on the Change of Implant Surface According to Application Time
- The effect of Er:YAG laser irradiation on the surface microstructure and roughness of hydroxyapatite-coated implant
- Comparison of the effect of hand instruments, an ultrasonic scaler, and an erbium-doped yttrium aluminium garnet laser on root surface roughness of teeth with periodontitis: a profilometer study
- The Effects of a Er:YAG Laser on Machined, Sand-Blasted and Acid-Etched, and Resorbable Blast Media Titanium Surfaces Using Confocal Microscopy and Scanning Electron Microscopy