Yonsei Med J.
2011 May;52(3):435-444. 10.3349/ymj.2011.52.3.435.
Cortisol Awakening Response and Nighttime Salivary Cortisol Levels in Healthy Working Korean Subjects
- Affiliations
-
- 1Department of Neurosurgery, Anam Hospital, Korea University College of Medicine, Seoul, Korea.
- 2CHA Biomedical Center, CHA University, Seoul, Korea. ryunsup@yahoo.co.kr
- 3Department of Statistics, Chonnam National University Medical School, Gwangju, Korea.
- 4Institute of Environmental and Occupational Medicine, Department of Occupational and Environmental Medicine, Pusan Paik Hospital, Inje University College of Medicine, Busan, Korea.
- 5Integrative Medicine Research Center, Anam Hospital, Korea University College of Medicine, Seoul, Korea.
- KMID: 1777015
- DOI: http://doi.org/10.3349/ymj.2011.52.3.435
Abstract
- PURPOSE
Cortisol awakening response (CAR) and nighttime cortisol levels have been used as indices of adrenocortical activity. However, population-based statistical information regarding these indices has not been provided in healthy subjects. This study was carried out to provide basic statistical information regarding these indices.
MATERIALS AND METHODS
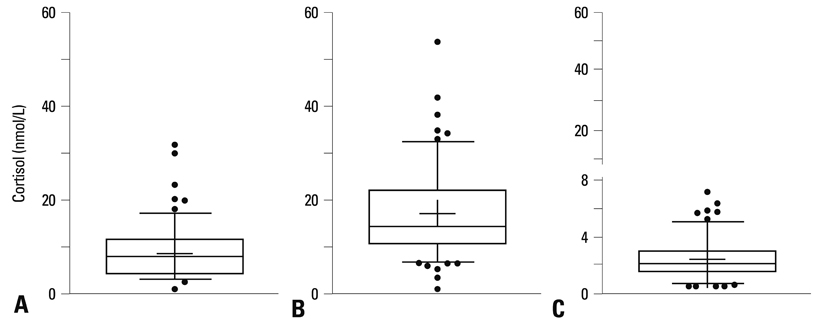
Cortisol levels were measured in saliva samples collected immediately upon awakening (0 min), 30 min after awakening and in the nighttime on two consecutive days in 133 healthy subjects.
RESULTS
We determined the mean [standard deviation (SD)], median (interquartile range) and 5th-95th percentile range for each measure and auxiliary indices for CAR, i.e., the secreted cortisol concentration within 30 min of awakening (CARscc) and absolute and relative increases in cortisol level within 30 min of awakening (CARi and CARi%, respectively). We also determined these values for auxiliary indices derived from nighttime cortisol level, i.e., the ratio of cortisol level 30 min after awakening (CA30 min) to nighttime level (CA30 min/NC), as well as absolute and relative decreases in cortisol levels from CA30 min to nighttime (DCd and DCd%, respectively). We found no significant differences in cortisol level for any time point or in auxiliary indices between collection days, genders and ages.
CONCLUSION
The provided descriptive information and statistics on the CAR and nighttime cortisol level will be helpful to medical specialists and researchers involved in hypothalamus-pituitary-adrenal axis assessment.
MeSH Terms
Figure
Reference
-
1. Clow A, Thorn L, Evans P, Hucklebridge F. The awakening cortisol response: methodological issues and significance. Stress. 2004. 7:29–37.
Article2. Hucklebridge F, Hussain T, Evans P, Clow A. The diurnal patterns of the adrenal steroids cortisol and dehydroepiandrosterone (DHEA) in relation to awakening. Psychoneuroendocrinology. 2005. 30:51–57.
Article3. Vining RF, McGinley RA, Maksvytis JJ, Ho KY. Salivary cortisol: a better measure of adrenal cortical function than serum cortisol. Ann Clin Biochem. 1983. 20:329–335.
Article4. Pruessner JC, Wolf OT, Hellhammer DH, Buske-Kirschbaum A, von Auer K, Jobst S, et al. Free cortisol levels after awakening: a reliable biological marker for the assessment of adrenocortical activity. Life Sci. 1997. 61:2539–2549.
Article5. Edwards S, Evans P, Hucklebridge F, Clow A. Association between time of awakening and diurnal cortisol secretory activity. Psychoneuroendocrinology. 2001. 26:613–622.
Article6. Wüst S, Wolf J, Hellhammer DH, Federenko I, Schommer N, Kirschbaum C. The cortisol awakening response - normal values and confounds. Noise Health. 2000. 2:79–88.7. Wilhelm I, Born J, Kudielka BM, Schlotz W, Wüst S. Is the cortisol awakening rise a response to awakening? Psychoneuroendocrinology. 2007. 32:358–366.
Article8. Federenko I, Wüst S, Hellhammer DH, Dechoux R, Kumsta R, Kirschbaum C. Free cortisol awakening responses are influenced by awakening time. Psychoneuroendocrinology. 2004. 29:174–184.
Article9. Schmidt-Reinwald A, Pruessner JC, Hellhammer DH, Federenko I, Rohleder N, Schürmeyer TH, et al. The cortisol response to awakening in relation to different challenge tests and a 12-hour cortisol rhythm. Life Sci. 1999. 64:1653–1660.
Article10. Buchanan TW, Kern S, Allen JS, Tranel D, Kirschbaum C. Circadian regulation of cortisol after hippocampal damage in humans. Biol Psychiatry. 2004. 56:651–656.
Article11. Wirtz PH, von Känel R, Emini L, Ruedisueli K, Groessbauer S, Maercker A, et al. Evidence for altered hypothalamus-pituitary-adrenal axis functioning in systemic hypertension: blunted cortisol response to awakening and lower negative feedback sensitivity. Psychoneuroendocrinology. 2007. 32:430–436.
Article12. Chida Y, Steptoe A. Cortisol awakening response and psychosocial factors: a systematic review and meta-analysis. Biol Psychol. 2009. 80:265–278.
Article13. McEwen BS, Wingfield JC. The concept of allostasis in biology and biomedicine. Horm Behav. 2003. 43:2–15.
Article14. Palesh O, Zeitzer JM, Conrad A, Giese-Davis J, Mustian KM, Popek V, et al. Vagal regulation, cortisol, and sleep disruption in women with metastatic breast cancer. J Clin Sleep Med. 2008. 4:441–449.
Article15. Lindeberg SI, Eek F, Lindbladh E, Ostergren PO, Hansen AM, Karlson B. Exhaustion measured by the SF-36 vitality scale is associated with a flattened diurnal cortisol profile. Psychoneuroendocrinology. 2008. 33:471–477.
Article16. Nater UM, Maloney E, Boneva RS, Gurbaxani BM, Lin JM, Jones JF, et al. Attenuated morning salivary cortisol concentrations in a population-based study of persons with chronic fatigue syndrome and well controls. J Clin Endocrinol Metab. 2008. 93:703–709.
Article17. Gafni RI, Papanicolaou DA, Nieman LK. Nighttime salivary cortisol measurement as a simple, noninvasive, outpatient screening test for Cushing's syndrome in children and adolescents. J Pediatr. 2000. 137:30–35.
Article18. Kim MS, Lee YJ, Ahn RS. Day-to-day differences in cortisol levels and molar cortisol-to-DHEA ratios among working individuals. Yonsei Med J. 2010. 51:212–218.
Article19. Kudielka BM, Broderick JE, Kirschbaum C. Compliance with saliva sampling protocols: electronic monitoring reveals invalid cortisol daytime profiles in noncompliant subjects. Psychosom Med. 2003. 65:313–319.
Article20. Schlotz W, Hellhammer J, Schulz P, Stone AA. Perceived work overload and chronic worrying predict weekend-weekday differences in the cortisol awakening response. Psychosom Med. 2004. 66:207–214.
Article21. Gröschl M, Wagner R, Rauh M, Dörr HG. Stability of salivary steroids: the influences of storage, food and dental care. Steroids. 2001. 66:737–741.
Article22. Gozansky WS, Lynn JS, Laudenslage ML, Kohrt WM. Salivary cortisol determined by enzyme immunoassay is preferable to serum total cortisol for assessment of dynamic hypothalamic--pituitary--adrenal axis activity. Clin Endocrinol (Oxf). 2005. 63:336–341.
Article23. Ahn RS, Lee YJ, Choi JY, Kwon HB, Chun SI. Salivary cortisol and DHEA levels in the Korean population: age-related differences, diurnal rhythm, and correlations with serum levels. Yonsei Med J. 2007. 48:379–388.
Article24. Buchanan TW, Kern S, Allen JS, Tranel D, Kirschbaum C. Circadian regulation of cortisol after hippocampal damage in humans. Biol Psychiatry. 2004. 56:651–656.
Article25. Wolf OT, Fujiwara E, Luwinski G, Kirschbaum C, Markowitsch HJ. No morning cortisol response in patients with severe global amnesia. Psychoneuroendocrinology. 2005. 30:101–105.
Article26. Brosnan M, Turner-Cobb J, Munro-Naan Z, Jessop D. Absence of a normal cortisol awakening response (CAR) in adolescent males with Asperger syndrome (AS). Psychoneuroendocrinology. 2009. 34:1095–1100.
Article27. Steptoe A, Siegrist J, Kirschbaum C, Marmot M. Effort-reward imbalance, overcommitment, and measures of cortisol and blood pressure over the working day. Psychosom Med. 2004. 66:323–329.
Article28. Pruessner JC, Kirschbaum C, Meinlschmid G, Hellhammer DH. Two formulas for computation of the area under the curve represent measures of total hormone concentration versus time-dependent change. Psychoneuroendocrinology. 2003. 28:916–931.
Article29. Hucklebridge F, Clow A, Evans P. The relationship between salivary secretory immunoglobulin A and cortisol: neuroendocrine response to awakening and the diurnal cycle. Int J Psychophysiol. 1998. 31:69–76.
Article30. Hucklebridge F, Sen S, Evans PD, Clow A. The relationship between circadian patterns of salivary cortisol and endogenous inhibitor of monoamine oxidase A. Life Sci. 1998. 62:2321–2328.
Article31. Hucklebridge FH, Clow A, Abeyguneratne T, Huezo-Diaz P, Evans P. The awakening cortisol response and blood glucose levels. Life Sci. 1999. 64:931–937.
Article32. Pruessner JC, Hellhammer DH, Kirschbaum C. Burnout, perceived stress, and cortisol responses to awakening. Psychosom Med. 1999. 61:197–204.
Article33. Schmidt-Reinwald A, Pruessner JC, Hellhammer DH, Federenko I, Rohleder N, Schürmeyer TH, et al. The cortisol response to awakening in relation to different challenge tests and a 12-hour cortisol rhythm. Life Sci. 1999. 64:1653–1660.
Article34. Edwards S, Clow A, Evans P, Hucklebridge F. Exploration of the awakening cortisol response in relation to diurnal cortisol secretory activity. Life Sci. 2001. 68:2093–2103.
Article35. Brooke-Wavell K, Clow A, Ghazi-Noori S, Evans P, Hucklebridge F. Ultrasound measures of bone and the diurnal free cortisol cycle: a positive association with the awakening cortisol response in healthy premenopausal women. Calcif Tissue Int. 2002. 70:463–468.
Article36. Kirschbaum C, Kudielka BM, Gaab J, Schommer NC, Hellhammer DH. Impact of gender, menstrual cycle phase, and oral contraceptives on the activity of the hypothalamus-pituitary-adrenal axis. Psychosom Med. 1999. 61:154–162.
Article37. Kudielka BM, Kirschbaum C. Awakening cortisol responses are influenced by health status and awakening time but not by menstrual cycle phase. Psychoneuroendocrinology. 2003. 28:35–47.
Article38. Kunz-Ebrecht SR, Kirschbaum C, Marmot M, Steptoe A. Differences in cortisol awakening response on work days and weekends in women and men from the Whitehall II cohort. Psychoneuroendocrinology. 2004. 29:516–528.
Article39. Sjögren E, Leanderson P, Kristenson M. Diurnal saliva cortisol levels and relations to psychosocial factors in a population sample of middle-aged Swedish men and women. Int J Behav Med. 2006. 13:193–200.
Article40. Aardal E, Holm AC. Cortisol in saliva--reference ranges and relation to cortisol in serum. Eur J Clin Chem Clin Biochem. 1995. 33:927–932.41. Hansen AM, Garde AH, Christensen JM, Eller NH, Netterstrøm B. Evaluation of a radioimmunoassay and establishment of a reference interval for salivary cortisol in healthy subjects in Denmark. Scand J Clin Lab Invest. 2003. 63:303–310.
Article42. Patel RS, Shaw SR, Macintyre H, McGarry GW, Wallace AM. Production of gender-specific morning salivary cortisol reference intervals using internationally accepted procedures. Clin Chem Lab Med. 2004. 42:1424–1429.
Article43. Wüst S, Federenko I, Hellhammer DH, Kirschbaum C. Genetic factors, perceived chronic stress, and the free cortisol response to awakening. Psychoneuroendocrinology. 2000. 25:707–720.
Article44. Cohen S, Schwartz JE, Epel E, Kirschbaum C, Sidney S, Seeman T. Socioeconomic status, race, and diurnal cortisol decline in the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Psychosom Med. 2006. 68:41–50.
Article45. DeSantis AS, Adam EK, Doane LD, Mineka S, Zinbarg RE, Craske MG. Racial/ethnic differences in cortisol diurnal rhythms in a community sample of adolescents. J Adolesc Health. 2007. 41:3–13.
Article46. Adam EK, Hawkley LC, Kudielka BM, Cacioppo JT. Day-to-day dynamics of experience--cortisol associations in a population-based sample of older adults. Proc Natl Acad Sci U S A. 2006. 103:17058–17063.
Article47. Grossi G, Perski A, Lundberg U, Soares J. Associations between financial strain and the diurnal salivary cortisol secretion of long-term unemployed individuals. Integr Physiol Behav Sci. 2001. 36:205–219.
Article48. Carroll T, Raff H, Findling JW. Late-night salivary cortisol measurement in the diagnosis of Cushing's syndrome. Nat Clin Pract Endocrinol Metab. 2008. 4:344–350.
Article49. Yaneva M, Mosnier-Pudar H, Dugué MA, Grabar S, Fulla Y, Bertagna X. Midnight salivary cortisol for the initial diagnosis of Cushing's syndrome of various causes. J Clin Endocrinol Metab. 2004. 89:3345–3351.
Article50. Raff H, Raff JL, Findling JW. Late-night salivary cortisol as a screening test for Cushing's syndrome. J Clin Endocrinol Metab. 1998. 83:2681–2686.
Article51. Castro M, Elias PC, Quidute AR, Halah FP, Moreira AC. Out-patient screening for Cushing's syndrome: the sensitivity of the combination of circadian rhythm and overnight dexamethasone suppression salivary cortisol tests. J Clin Endocrinol Metab. 1999. 84:878–882.
Article52. Papanicolaou DA, Mullen N, Kyrou I, Nieman LK. Nighttime salivary cortisol: a useful test for the diagnosis of Cushing's syndrome. J Clin Endocrinol Metab. 2002. 87:4515–4521.
Article53. Solberg HE. The theory of reference values Part 5. Statistical treatment of collected reference values. Determination of reference limits. J Clin Chem Clin Biochem. 1983. 21:749–760.
Article54. Solberg HE. International Federation of Clinical Chemistry (IFCC). Scientific Committee. Clinical Section. Expert Panel on Theory of Reference Values. International Committee for Standardization in Haematology (ICSH), Standing Committee on Reference Values. Approved Recommendation (1986) on the theory of reference values. Part 1. The concept of reference values. J Clin Chem Clin Biochem. 1987. 25:337–342.
Article55. Solberg HE, PetitClerc C. International Federation of Clinical Chemistry (IFCC). Scientific Committee. Clinical Section. Expert Panel on Theory of Reference Values. Approved recommendation (1988) on the theory of reference values. Part 3. Preparation of individuals and collection of specimens for the production of reference values. J Clin Chem Clin Biochem. 1988. 26:593–598.
Article56. Solberg HE, Stamm D. International Federation of Clinical Chemistry, Scientific Division: approved recommendation on the theory of reference values. Part 4. Control of analytical variation in the production, transfer and application of reference values. Eur J Clin Chem Clin Biochem. 1991. 29:531–535.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- An Exploratory Study on Occupational Stress and Anxiety Through Salivary Cortisol and Self-Report Scale in Korean Nurses on Shift and Regular Work
- Day-to-Day Differences in Cortisol Levels and Molar Cortisol-to-DHEA Ratios among Working Individuals
- Exploring Subjective Stress, Sleep and Diurnal Variation of Salivary Cortisol in Korean Female Adults
- Comparison of salivary and serum cortisol levels in mechanically ventilated patients and non-critically ill patients
- Determination of Appropriate Sampling Time for Job Stress Assessment: the Salivary Chromogranin A and Cortisol in Adult Females