J Korean Assoc Oral Maxillofac Surg.
2010 Aug;36(4):243-249. 10.5125/jkaoms.2010.36.4.243.
Osteoblast differentiation of human bone marrow stromal cells (hBMSC) according to age for bone tissue engineering
- Affiliations
-
- 1Department of Molecular Genetics, School of Dentistry and Dental Research Institute, BK21 Program, Seoul, Korea.
- 2Department of Oral and Maxillofacial Surgery, School of Dentistry, Seoul National University, Seoul, Korea. jinychoi@plaza.snu.ac.kr
- KMID: 1457774
- DOI: http://doi.org/10.5125/jkaoms.2010.36.4.243
Abstract
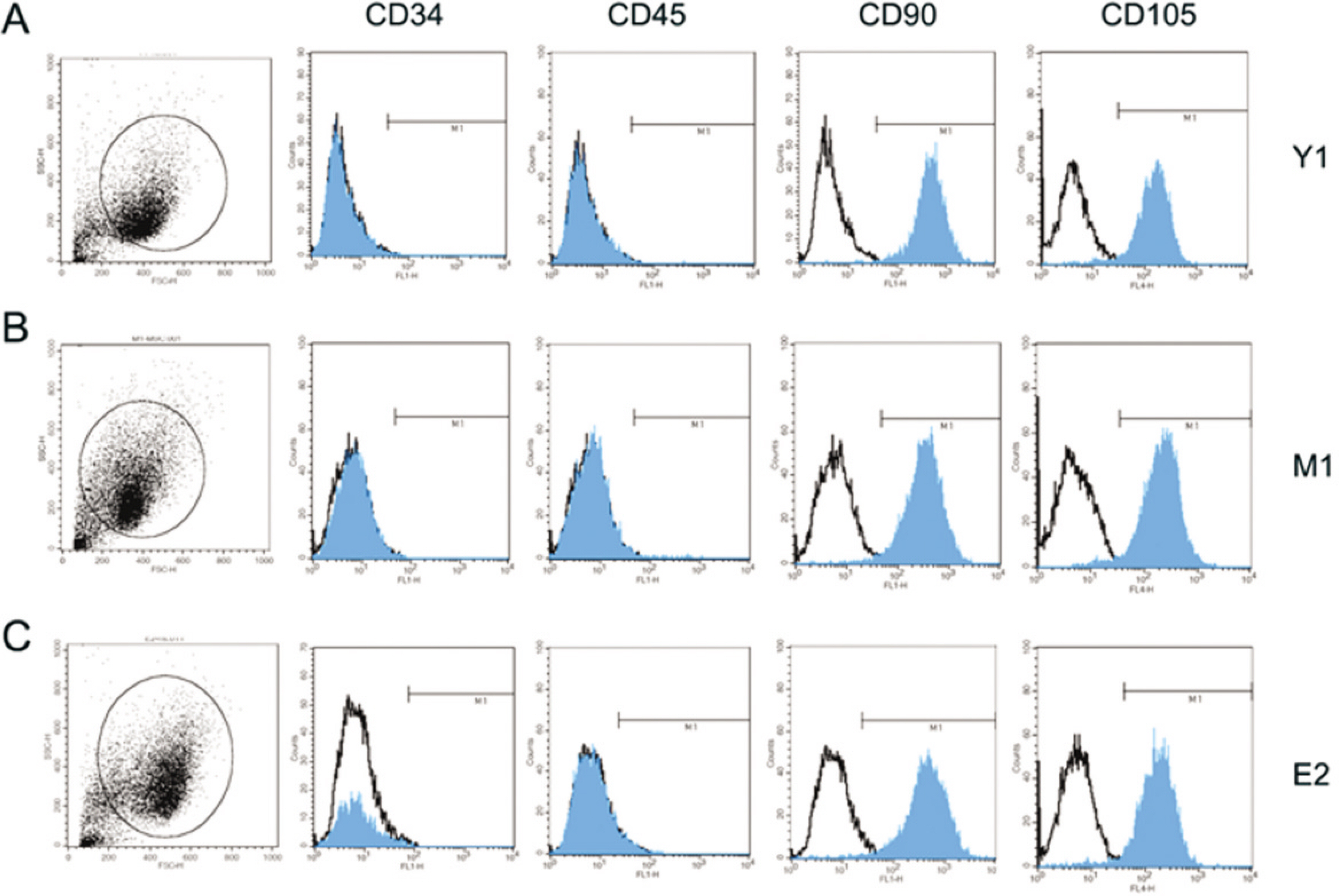
- Tissue engineered bone (TEB) can replace an autogenous bone graft requiring an secondary operation site as well as avoid complications like inflammation or infection from xenogenic or synthetic bone graft. Adult mesenchymal stem cells (MSC) for TEB are considered to have various ranges of differentiation capacity or multipotency by the donor site and age. This study examined the effect of age on proliferation capacity, differentiation capacity and bone morphogenetic protein-2 (BMP-2) responsiveness of human bone marrow stromal cells (hBMSC) according to the age. In addition, to evaluate the effect on enhancement for osteoblast differentiation, the hBMSC were treated with Trichostatin A (TSA) and 5-Azacitidine (5-AZC) which was HDAC inhibitors and methyltransferase inhibitors respectively affecting chromatin remodeling temporarily and reversibly. The young and old group of hBMSC obtained from the iliac crest from total 9 healthy patients, showed similar proliferation capacity. Cell surface markers such as CD34, CD45, CD90 and CD105 showed uniform expression regardless of age. However, the young group showed more prominent transdifferentiation capacity with adipogenic differentiation. The osteoblast differentiation capacity or BMP responsiveness was low and similar between young and old group. TSA and 5-AZC showed potential for enhancing the BMP effect on osteoblast differentiation by increasing the expression level of osteogenic master gene, such as DLX5, ALP. More study will be needed to determine the positive effect of the reversible function of HDAC inhibitors or methyltransferase inhibitors on enhancing the low osteoblast differentiation capacity of hBMSC.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Conget PA, Minguell JJ. Phenotypical and functional properties of human bone marrow mesenchymal progenitor cells. J Cell Physiol. 1999; 181:67–73.
Article2. Zhou S, Greenberger JS, Epperly MW, Goff JP, Adler C, Leboff MS, et al. Age-related intrinsic changes in human bone-marrowderived mesenchymal stem cells and their differentiation to osteoblasts. Aging Cell. 2008; 7:335–43.
Article3. Ma D, Ma Z, Zhang X, Wang W, Yang Z, Zhang M, et al. Effect of age and extrinsic microenvironment on the proliferation and osteogenic differentiation of rat dental pulp stem cells in vitro. J Endod. 2009; 35:1546–53.
Article4. Benetti R, Garcia-Cao M, Blasco MA. Telomere length regulates the epigenetic status of mammalian telomeres and subtelomeres. Nat Genet. 2007; 39:243–50.
Article5. Gonzalo S, Jaco I, Fraga MF, Chen T, Li E, Esteller M, et al. DNA methyltransferases control telomere length and telomere recombination in mammalian cells. Nat Cell Biol. 2006; 8:416–24.
Article6. Schroeder TM, Westendorf JJ. Histone deacetylase inhibitors promote osteoblast maturation. J Bone Miner Res. 2005; 20:2254–63.
Article7. de Boer J, Licht R, Bongers M, van der Klundert T, Arends R, van Blitterswijk C. Inhibition of histone acetylation as a tool in bone tissue engineering. Tissue Eng. 2006; 12:2927–37.8. Jeon EJ, Lee KY, Choi NS, Lee MH, Kim HN, Jin YH, et al. Bone morphogenetic protein-2 stimulates Runx2 acetylation. J Biol Chem. 2006; 281:16502–11.
Article9. Atkinson SP, Keith WN. Epigenetic control of cellular senescence in disease: opportunities for therapeutic intervention. Expert Rev Mol Med. 2007; 9:1–26.
Article10. Hu E, Tontonoz P, Spiegelman BM. Transdifferentiation of my-oblasts by the adipogenic transcription factors PPAR gamma and C/EBP alpha. Proc Natl Acad Sci U S A. 1995; 92:9856–60.
Article11. Ogawa A, Ohba K, Uchida Y, Wada K, Yoshioka T, Muraki T. New adipogenic cell lines derived from C3H10T1/2. In Vitro Cell Dev Biol Anim. 1999; 35:307–10.
Article12. Pittenger MF, Mackay AM, Beck SC, Jaiswal RK, Douglas R, Mosca JD, et al. Multilineage potential of adult human mesenchymal stem cells. Science. 1999; 284:143–7.
Article13. Fang H, Yang X, Chen A, Luo Y. Effect of rhBMP-2 and osteogenic revulsants on proliferation and differentiation of bone marrow stromal cells in rats. J Huazhong Univ Sci Technolog Med Sci. 2007; 27:561–3.
Article14. Osyczka AM, Diefenderfer DL, Bhargave G, Leboy PS. Different effects of BMP-2 on marrow stromal cells from human and rat bone. Cells Tissues Organs. 2004; 176:109–19.
Article15. Justesen J, Stenderup K, Eriksen EF, Kassem M. Maintenance of osteoblastic and adipocytic differentiation potential with age and osteoporosis in human marrow stromal cell cultures. Calcif Tissue Int. 2002; 71:36–44.
Article16. Kretlow JD, Jin YQ, Liu W, Zhang WJ, Hong TH, Zhou G, et al. Donor age and cell passage affects differentiation potential of murine bone marrowderived stem cells. BMC Cell Biol. 2008; 9:60.
Article17. Mizuno D, Agata H, Furue H, Kimura A, Narita Y, Watanabe N, et al. Limited but heterogeneous osteogenic response of human bone marrow mesenchymal stem cells to bone morphogenetic protein-2 and serum. Growth Factors. 2010; 28:34–43.
Article18. Diefenderfer DL, Osyczka AM, Reilly GC, Leboy PS. BMP responsiveness in human mesenchymal stem cells. Connect Tissue Res. 2003; 44(Suppl 1):305–11.
Article19. Fleet JC, Cashman K, Cox K, Rosen V. The effects of aging on the bone inductive activity of recombinant human bone morphogenetic protein-2. Endocrinology. 1996; 137:4605–10.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of Glucocorticoid on Apoptosis of Human Bone Marrow Osteogenic Stromal Cells
- Effect of Dexamethasone and 1,25(OH)2D3 on Proliferation and Osteogenic Differentiation of Cultured Human Bone Marrow Stromal Cells
- Mesenchymal Stem Cells for Tissue Engineering and Regenerative Medicine
- Interaction of TGF-beta1 and rhBMP-2 on Human Bone Marrow Stromal Cells Cultured in Collagen Gel Matrix
- Effect of Fibroblast Growth Factor-2 and Retinoic Acid on Lineage Commitment of Bone Marrow Mesenchymal Stem Cells