Korean J Physiol Pharmacol.
2010 Apr;14(2):83-89. 10.4196/kjpp.2010.14.2.83.
The Inhibitory Effects of Hydrogen Sulfide on Pacemaker Activity of Interstitial Cells of Cajal from Mouse Small Intestine
- Affiliations
-
- 1Department of Physiology, College of Medicine, Chosun University, Gwangju 501-759, Korea. jyjun@chosun.ac.kr
- 2Department of Internal Medicine, College of Medicine, Chosun University, Gwangju 501-759, Korea.
- KMID: 1457673
- DOI: http://doi.org/10.4196/kjpp.2010.14.2.83
Abstract
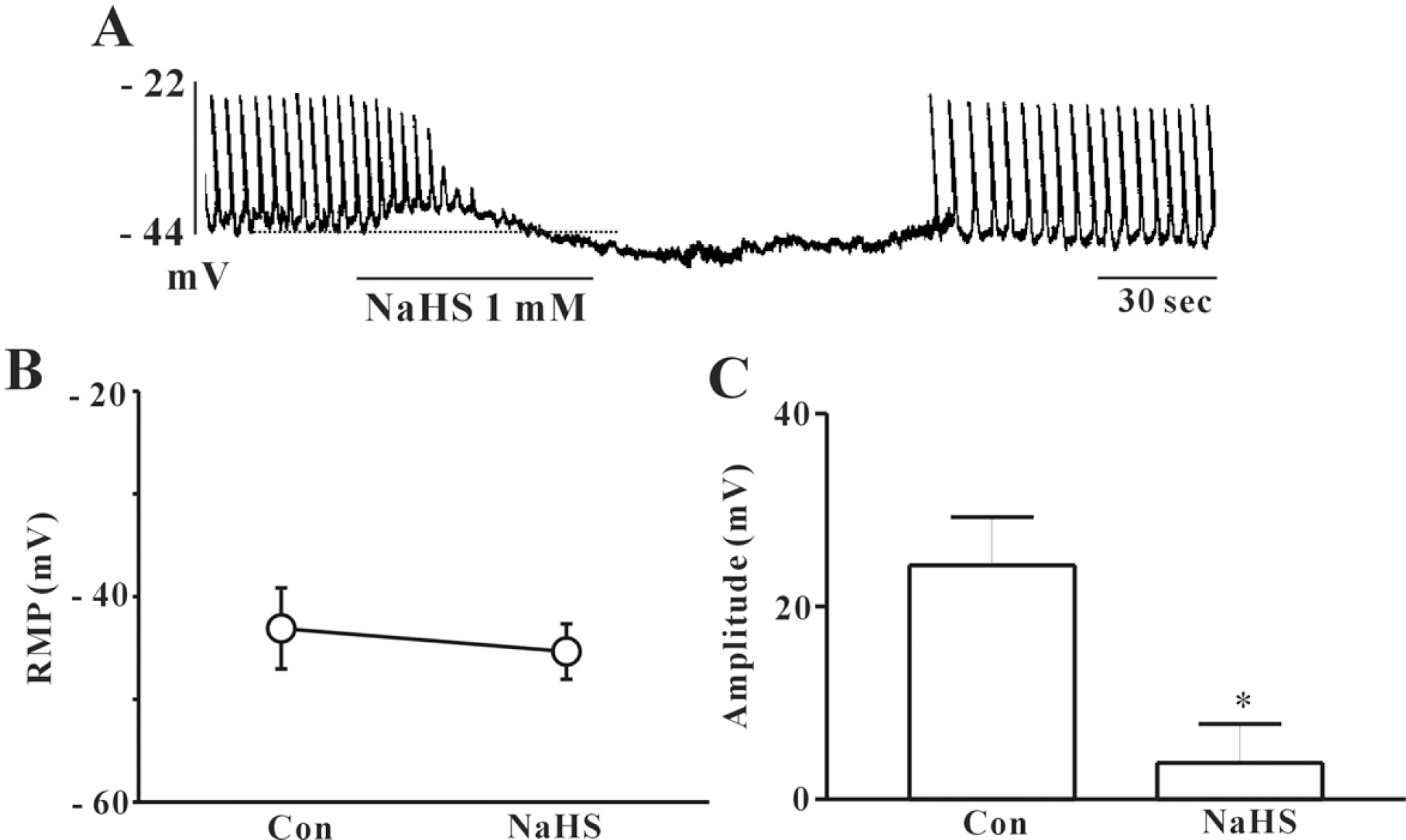
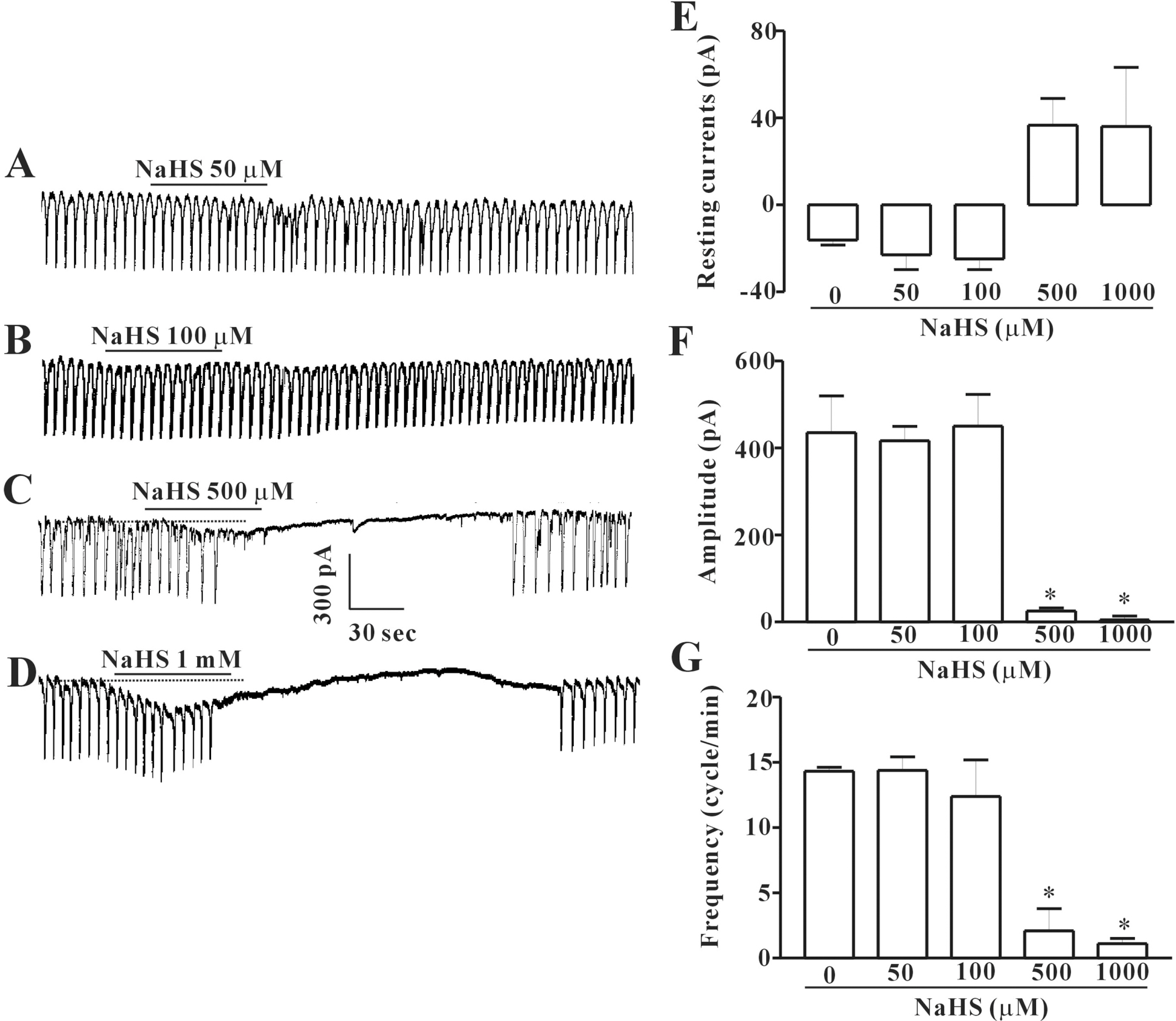
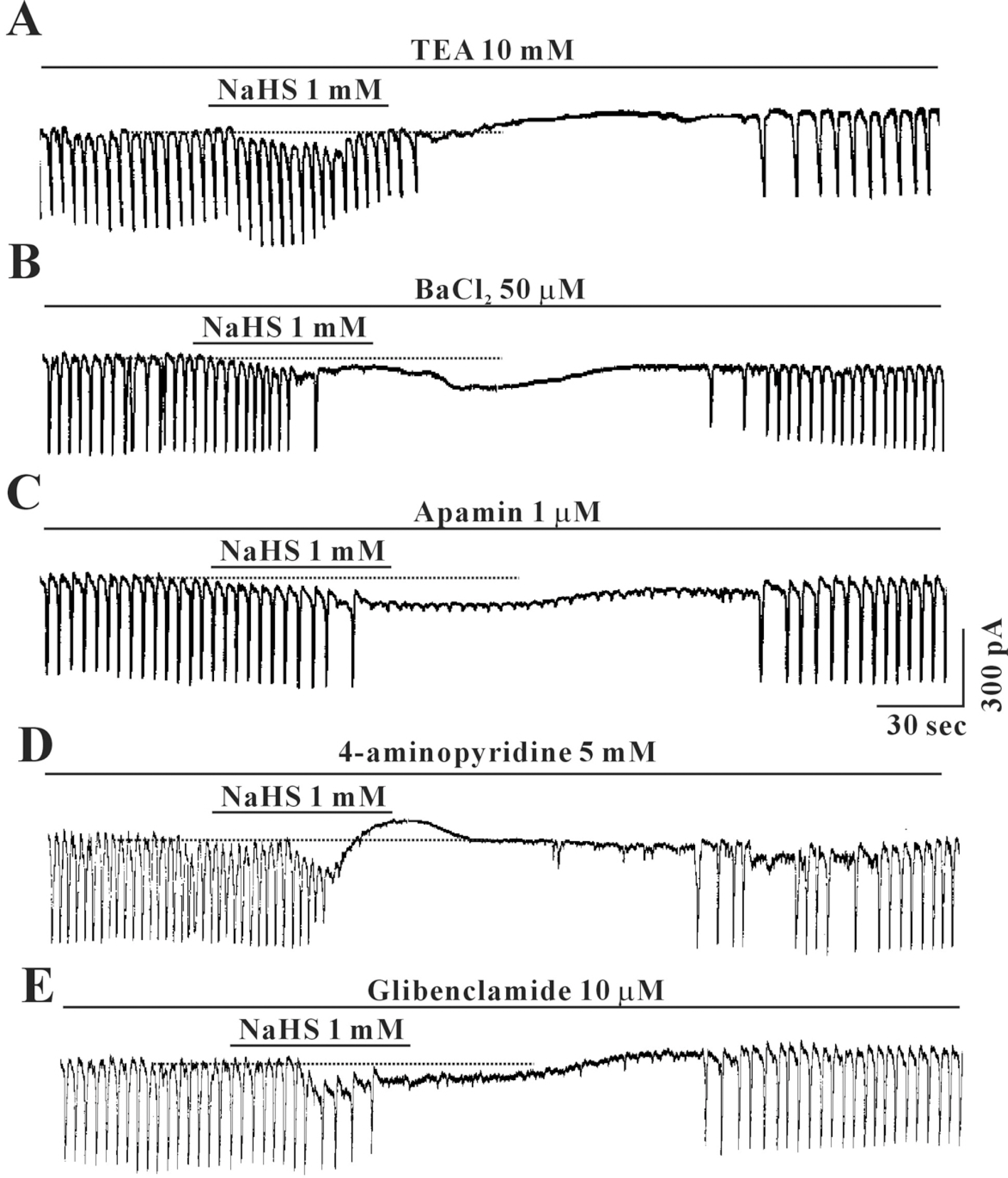
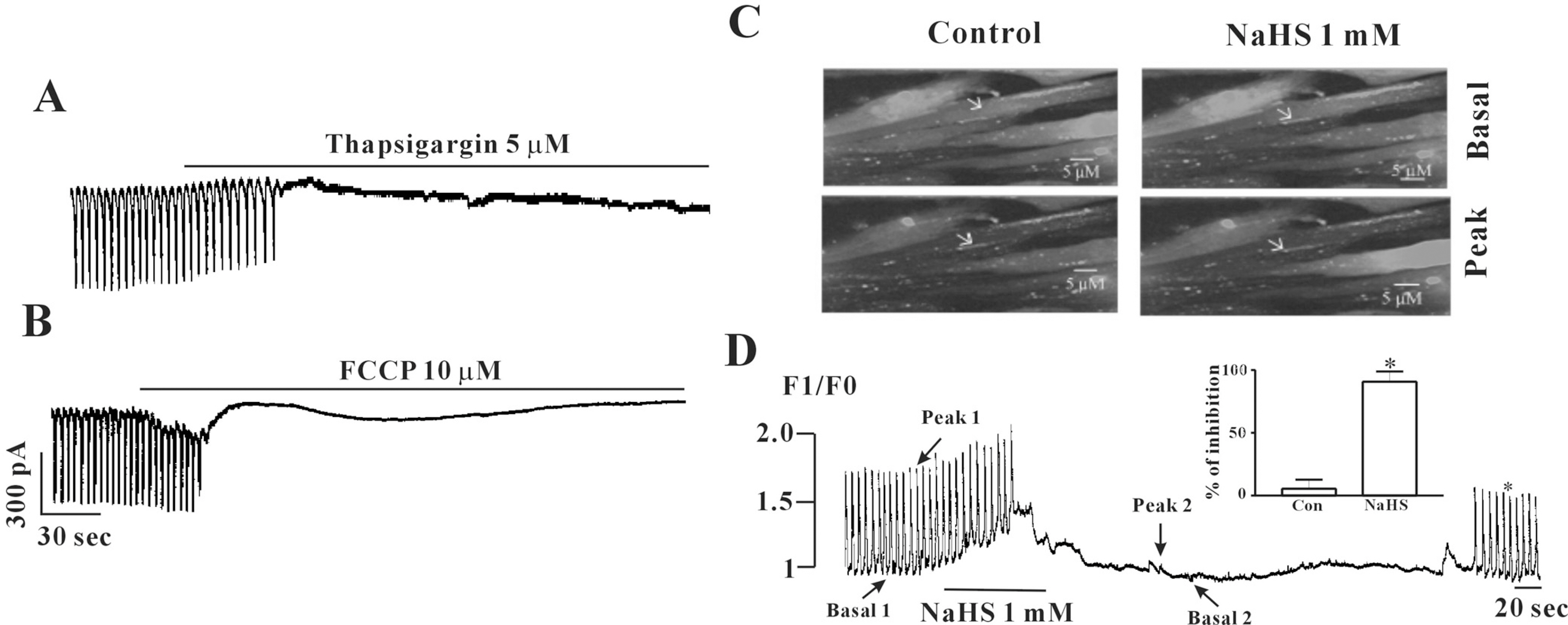
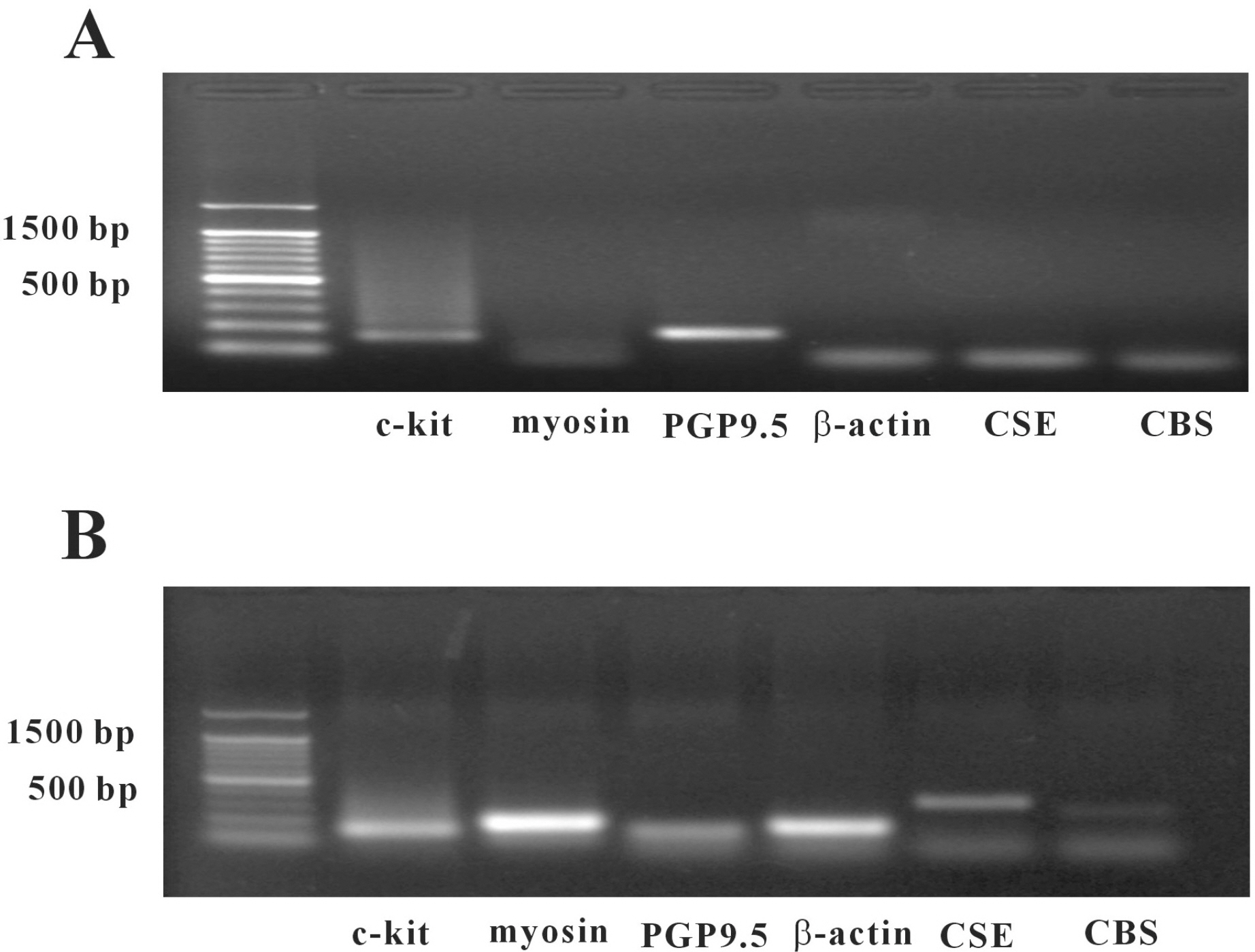
- In this study, we studied whether hydrogen sulfide (H2S) has an effect on the pacemaker activity of interstitial cells of Cajal (ICC), in the small intestine of mice. The actions of H2S on pacemaker activity were investigated using whole-cell patch-clamp technique, intracellular Ca2+ analysis at 30degrees C and RT-PCR in cultured mouse intestinal ICC. Exogenously applied sodium hydrogen sulfide (NaHS), a donor of hydrogen sulfide, caused a slight tonic inward current on pacemaker activity in ICC at low concentrations (50 and 100 micrometer), but at high concentration (500 micrometer and 1 mM) it seemed to cause light tonic inward currents and then inhibited pacemaker amplitude and pacemaker frequency, and also an increase in the resting currents in the outward direction. Glibenclamide or other potassium channel blockers (TEA, BaCl2, apamin or 4-aminopydirine) did not have an effect on NaHS-induced action in ICC. The exogenous application of carbonilcyanide p-triflouromethoxyphenylhydrazone (FCCP) and thapsigargin also inhibited the pacemaker activity of ICC as NaHS. Also, we found NaHS inhibited the spontaneous intracellular Ca2+ ([Ca2+]i) oscillations in cultured ICC. In doing an RT-PCR experiment, we found that ICC enriched population lacked mRNA for both CSE and CBS, but was prominently detected in unsorted muscle. In conclusion, H2S inhibited the pacemaker activity of ICC by modulating intracellular Ca2+. These results can serve as evidence of the physiological action of H2S as acting on the ICC in gastrointestinal (GI) motility.
Keyword
MeSH Terms
-
Animals
Apamin
Barium Compounds
Chlorides
Gastrointestinal Motility
Glyburide
Humans
Hydrogen
Hydrogen Sulfide
Interstitial Cells of Cajal
Intestine, Small
Light
Mice
Muscles
Patch-Clamp Techniques
Potassium Channel Blockers
RNA, Messenger
Sodium
Sulfides
Thapsigargin
Tissue Donors
Apamin
Barium Compounds
Chlorides
Glyburide
Hydrogen
Hydrogen Sulfide
Potassium Channel Blockers
RNA, Messenger
Sodium
Sulfides
Thapsigargin
Figure
Cited by 1 articles
-
Interplay of Hydrogen Sulfide and Nitric Oxide on the Pacemaker Activity of Interstitial Cells of Cajal from Mouse Small Intestine
Pyung Jin Yoon, Shanker Prasad Parajuli, Dong Chuan Zuo, Pawan Kumar Shahi, Hyung Jung Oh, Hae Rang Shin, Mi Jung Lee, Cheol Ho Yeum, Seok Choi, Jae Yeoul Jun
Chonnam Med J. 2011;47(2):72-79. doi: 10.4068/cmj.2011.47.2.72.
Reference
-
References
1. Goodwin LR, Francom D, Dieken FP, Taylor JD, Warenycia NW, Reiffenstein RJ, Dowling G. Determination of sulfide in brain tissue by gas dialysis/ion chromatography: post-mortem studies and two case reports. J Anal Toxicol. 1989; 13:105–109.
Article2. Warenycia MW, Goodwin LR, Benishin CG, Reiffenstein RJ, Francom DM, Taylor JD, Dicken FP. Acute hydrogen sulfide poisoning: demonstration of selective uptake of sulfide by the brainstem by measurement of brain sulfide level. Biochem Pharmacol. 1989; 38:973–981.3. Savage JC, Gould DH. Determination of sulfides in brain tissue and rumen fluid by ion-interaction reversed-phased high-performance liquid chromatography. J Chromatogr. 1990; 526:540–545.4. Patacchini R, Santicioli P, Giuliani S, Maggi CA. Hydrogen sulfide (H2S) stimulates capsaicin-sensitive primary afferent neurons in the rat urinary bladder. Br J Pharmacol. 2004; 142:31–34.5. Hosoki R, Matsiki N, Kimura H. The possible role of hydrogen sulfide as an endogenous smooth muscle relaxant in synergy with nitric oxide. Biochem Biophysic Res Commun. 1997; 237:527–541.
Article6. Gallego D, Clave P, Donovan J, Rahmati R, Grundy D, Jimenez M, Beyak MJ. The gaseous mediator, hydrogen sulphide, inhibits in vitro motor patterns in the human, rat and mouse colon and jejunum. Neurogastroenterol Motil. 2008; 20:1306–1316.7. Ward SM, Burns AJ, Torihashi S, Harney SC, Sanders KM. Impaired development of interstitial cells and intestinal electrical rhythmicity in steel mutants. Am J Physiol. 1995; 269:C1577–1588.
Article8. Zhao W, Zhang J, Lu Y, Wang R. The vasorelaxant effect of H2S as a novel endogenous gaseous KATP channel opener. EMBO J. 2001; 20:6008–6016.9. Abe K, Kimura H. The possible role of hydrogen sulfide as an endogenous neuromodulator. J Neurosci. 1996; 16:1066–1071.
Article10. Reiffenstein RJ, Hulbert WC, Roth SH. Toxicology of hydrogen sulfide. Ann Rev Pharmacol Toxicol. 1992; 32:109–134.
Article11. Rodrigo GC, Standen NB. ATP-sensitive potassium channels. Curr Pharm Des. 2005; 11:1915–1940.
Article12. Choi S, Yeum CH, Chang IY, You HJ, Park JS, Jeong HS, So I, Kim KW, Jun JY. Activating of ATP-dependent K+ channels comprised of Kir6.2 and SUR 2B by PGE2 through EP2 receptor in cultured interstitial cells of Cajal from murine small intestine. Cell Physiol Biochem. 2006; 18:187–198.13. Kubo S, Doe I, Kurokawa Y, Nishikawa H, Kawabata A. Direct inhibition of endothelial nitric oxide synthase by hydrogen sulfide: contribution of dual modulation of vascular tension. Toxicol. 2007; 232:138–146.14. Koh SD, Sanders KM. Stretch-dependent potassium channels in murine colonic smooth muscle cells. J Physiol. 2001; 533:155–163.
Article15. Park KJ, Baker SA, Cho SY, Sanders KM, Koh SD. Sulfur-containing amino acids block stretch-dependent K+ channels and nitrergic responses in the murine colon. Br J Pharmacol. 2005; 144:1126–1137.16. Suzuki H, Takano H, Yamamoto Y, Komuro T, Saito M, Kato K, Mikoshiba K. Properties of gastric smooth muscles obtained from mice which lack inositol trisphosphate receptor. J Physiol. 2000; 525:105–111.
Article17. Ward SM, Ordog T, Koh SD, Baker SA, Jun JY, Amberg G, Monaghan K, Sanders KM. Pacemaking in interstitial cells of Cajal depends upon calcium handling by endoplasmic reticulum and mitochondria. J Physiol. 2000; 525:355–361.
Article18. Jun JY, Choi S, Yeum CH, Chang IY, You HJ, Park CK, Kim MY, Kong ID, Kim MJ, Lee KP, So I, Kim KW. Substance P induces inward current and regulates pacemaker currents through tachykinin NK1 receptor in cultured interstitial cells of Cajal of murine small intestine. Eur J Pharmacol. 2004; 495:35–42.
Article19. Bukovska G, Kery V, Kraus JP. Expression of human cystathionine beta-synthase in Escherichia coli: purification and characterization. Protein Exp Purif. 1994; 5:442–448.20. Erickson PF, Maxwell IH, Su LJ, Baumann M, Glode LM. Sequence of cDNA for rat cystathionine gamma-lyase and comparison of deduced amino acid sequence with related Escherichia coli enzymes. Biochem J. 1990; 269:335–340.21. Barber T, Triguero A, Martinez LI, Torres L, Garcia C, Miralles VJ, Vina JR. Elevated expression of liver gamma-cystathionase is required for the maintenance of lactation in rats. J Nutr. 1999; 129:928–933.22. Fiorucci S, Distrutti E, Cirino G, Wallace JL. The emerging roles of hydrogen sulfide in the gastrointestinal tract and liver. Gastroenterol. 2006; 131:259–271.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Interplay of Hydrogen Sulfide and Nitric Oxide on the Pacemaker Activity of Interstitial Cells of Cajal from Mouse Small Intestine
- Capsaicin Inhibits the Spontaneous Pacemaker Activity in Interstitial Cells of Cajal From the Small Intestine of Mouse
- Inhibition of Pacemaker Activity of Interstitial Cells of Cajal by Hydrogen Peroxide via Activating ATP-sensitive K(+) Channels
- Effects of ATP on Pacemaker Activity of Interstitial Cells of Cajal from the Mouse Small Intestine
- The Pharmacological Regulation of Interstitial Cells of Cajal in the Small Intestine