J Korean Surg Soc.
2012 Jan;82(1):45-49. 10.4174/jkss.2012.82.1.45.
Inflammatory myofibroblastic tumor in colon
- Affiliations
-
- 1Department of Surgery, The Catholic University of Korea School of Medicine, Seoul, Korea. cmcgslee@catholic.ac.kr
- 2Department of Radiology, The Catholic University of Korea School of Medicine, Seoul, Korea.
- 3Department of Hospital Pathology, The Catholic University of Korea School of Medicine, Seoul, Korea.
- 4Department of Internal Medicine, The Catholic University of Korea School of Medicine, Seoul, Korea.
- KMID: 1437757
- DOI: http://doi.org/10.4174/jkss.2012.82.1.45
Abstract
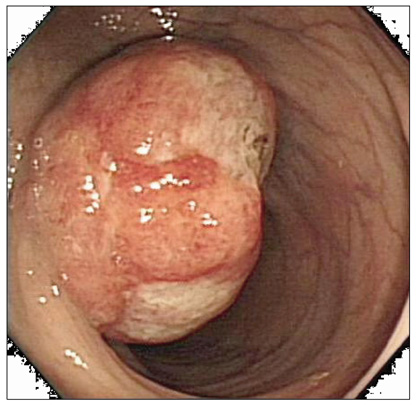
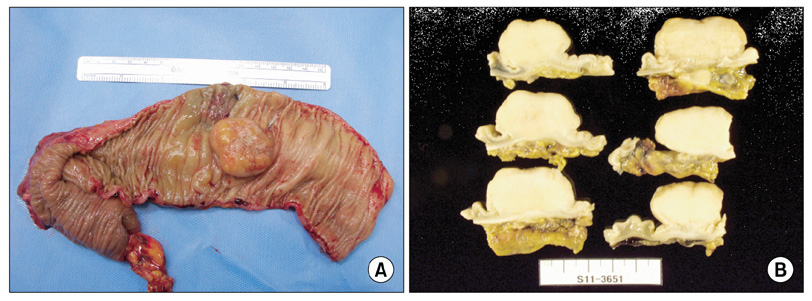
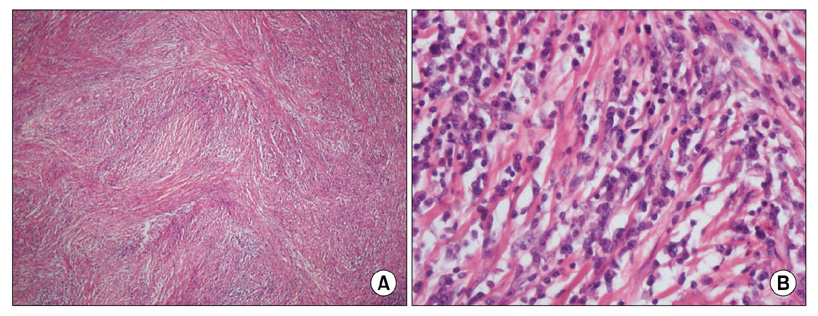
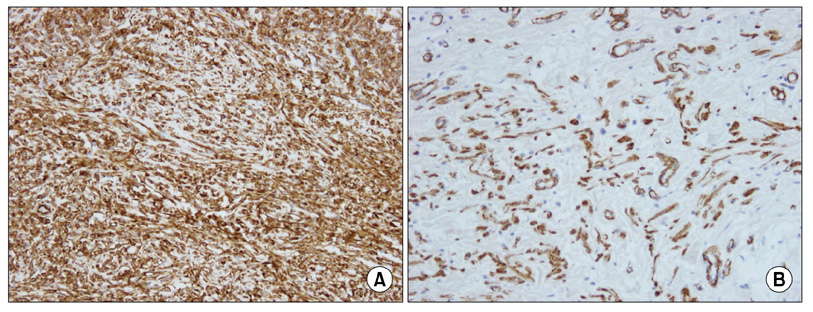
- Inflammatory myofibroblastic tumor (IMT) is an uncommon mesenchymal solid tumor commonly documented in children and young adults. Here, we report a case of IMT in colon confirmed pathologically after laparoscopic anterior resection. A 35-year-old man presented with anal bleeding after defecation for 2 weeks. Colonoscopy demonstrated a mass with shallow ulceration in the central area and irregular margin accompanied by intact mucosa in the descending colon. Computer tomography showed a well-demarcated and homogenous solitary mass in the descending colon. We performed laparoscopic anterior resection. This case was diagnosed as IMT after microscopic examination. The tumor was composed of a proliferation of spindle-shaped cells arranged in the hyaline material with chronic inflammatory cells, composed mainly of plasma cells and lymphocytes. Immunohistochemically, tumor cells were positive for smooth muscle actin, and vimentin, and negative for desmin, CD117 (c-kit), anaplastic lymphoma kinase-1.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Two Cases of Infantile Intra-abdominal Inflammatory Myofibroblastic Tumor
Soo-Hong Kim, Yong Hoon Cho, Hae Young Kim
Pediatr Gastroenterol Hepatol Nutr. 2014;17(2):116-120. doi: 10.5223/pghn.2014.17.2.116.
Reference
-
1. Tanaka A, Hirabayashi K, Sadahiro S, Maeda Y, Suzuki T, Ogoshi K. Inflammatory myofibroblastic tumor of the ascending colon in adults manifested by positive fecal occult blood test. Gastrointest Endosc. 2010. 71:214–216.2. Coffin CM, Hornick JL, Fletcher CD. Inflammatory myofibroblastic tumor: comparison of clinicopathologic, histologic, and immunohistochemical features including ALK expression in atypical and aggressive cases. Am J Surg Pathol. 2007. 31:509–520.3. Saleem MI, Ben-Hamida MA, Barrett AM, Bunn SK, Huntley L, Wood KM, et al. Lower abdominal inflammatory myofibroblastic tumor -an unusual presentation-a case report and brief literature review. Eur J Pediatr. 2007. 166:679–683.4. Salameh M, Sultan I, Barbar M, Al Hussaini M, Jameel A, Ghandour K, et al. Inflammatory myofibroblastic tumor causing unexplained anemia in a toddler: a case report. J Med Case Reports. 2011. 5:69.5. Kovach SJ, Fischer AC, Katzman PJ, Salloum RM, Ettinghausen SE, Madeb R, et al. Inflammatory myofibroblastic tumors. J Surg Oncol. 2006. 94:385–391.6. Karnak I, Senocak ME, Ciftci AO, Cağlar M, Bingöl-Koloğlu M, Tanyel FC, et al. Inflammatory myofibroblastic tumor in children: diagnosis and treatment. J Pediatr Surg. 2001. 36:908–912.7. Coffin CM, Fletcher JA. Fletcher CD, Unni KK, Mertens F, editors. Inflammatory myofibroblastic tumour. World Health Organization classification of tumours Pathology and genetics of tumours of soft tissue and bone. 2002. Lyon: IARC Press;91–93.8. Greenson JK. Gastrointestinal stromal tumors and other mesenchymal lesions of the gut. Mod Pathol. 2003. 16:366–375.9. Chun YS, Wang L, Nascimento AG, Moir CR, Rodeberg DA. Pediatric inflammatory myofibroblastic tumor: anaplastic lymphoma kinase (ALK) expression and prognosis. Pediatr Blood Cancer. 2005. 45:796–801.10. Jiang YH, Cheng B, Ge MH, Cheng Y, Zhang G. Comparison of the clinical and immunohistochemical features, including anaplastic lymphoma kinase (ALK) and p53, in inflammatory myofibroblastic tumours. J Int Med Res. 2009. 37:867–877.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Inflammatory Myofibroblastic Tumor of Nasal Septum after Septoplasty: A Case Report
- Huge Inflammatory Myofibroblastic Tumor Arising from the Abdominal Wall
- Inflammatory Myofibroblastic Tumor of Kidney
- Inflammatory Myofibroblastic Tumor of the Mesentery: A case report
- A Case of Inflammatory Myofibroblastic Tumor of the Maxillary Sinus