Near-Road Exposure and Impact of Air Pollution on Allergic Diseases in Elementary School Children: A Cross-Sectional Study
- Affiliations
-
- 1Department of Integrated Environmental Systems, Pyeongtaek University, Pyeongtaek, Korea.
- 2Research Development and Education Division, National Institute of Chemical Safety, Ministry of Environment, Daejeon, Korea.
- 3Environmental Health Research Division, Environmental Health Research Department, National Institute of Environmental Research, Ministry of Environment, Incheon, Korea.
- 4Department of Environmental Science and Engineering, Kyung Hee University College of Engineering, Suwon, Korea.
- 5Institute for Environmental Research, Yonsei University College of Medicine, Seoul, Korea. envlim@yuhs.ac
- 6The Environment Technology Institute, Coway., Ltd., Seoul, Korea.
- KMID: 2374091
- DOI: http://doi.org/10.3349/ymj.2016.57.3.698
Abstract
- PURPOSE
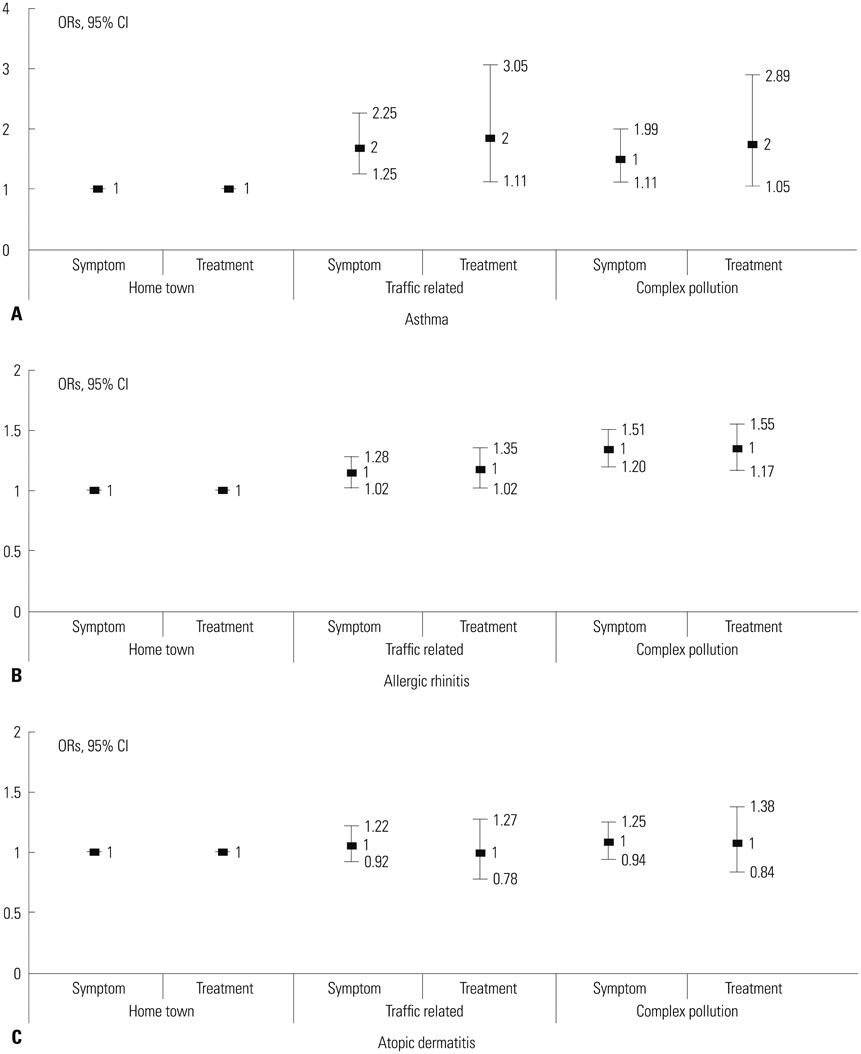
The study aims to classify schools based on traffic pollutants and their complex sources, to assess the environment, to determine the state of allergic diseases among students using the International Study of Asthma and Allergies in children (ISAAC) questionnaire, and to assess their connection to air pollutants.
MATERIALS AND METHODS
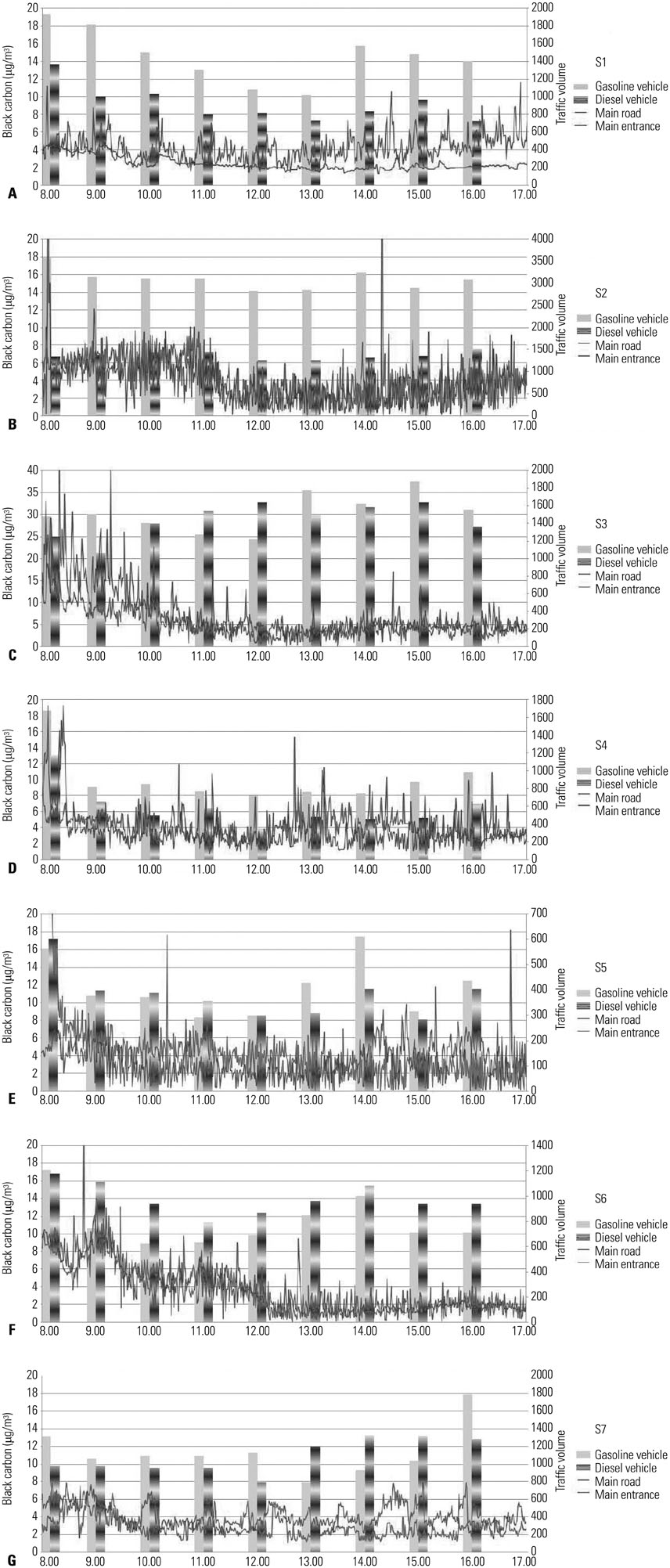
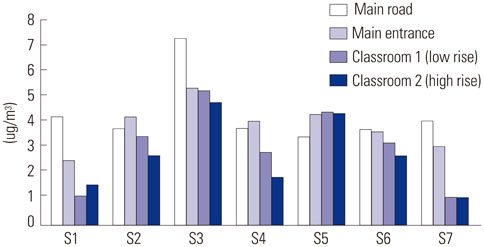
A total of seven schools were divided into three categories according to the characteristics of their surrounding environments: three schools in traffic-related zones, two schools in complex source zones I (urban), and two schools in complex source zones II (industrial complex). ISAAC questionnaires were administered and the 4404 completed questionnaires were analyzed.
RESULTS
The frequency of asthma treatment during the past 12 months showed a significant increase (p<0.05) with exposure to NO2 [1.67, 95% confidence intervals (CIs) 1.03-2.71] in the complex source zones. The frequency of allergic rhinitis treatment during the past 12 months increased significantly with exposure to Black Carbon (1.60, 95% CIs 1.36-1.90) (p<0.001), SO2 (1.09, 95% CIs 1.01-1.17) (p<0.05), NO2 (1.18, 95% CIs 1.07-1.30) (p<0.01) for all subjects.
CONCLUSION
In terms of supporting children's health, care, and prevention related to major spaces for children, such as school zones, spaces used in coming to and leaving school, playgrounds, and classrooms are essential to ensuring not only the safety of children from traffic accidents but also their protection from local traffic pollutants and various hazardous environmental factors.
Keyword
MeSH Terms
-
Adolescent
Air Pollutants/*adverse effects
Air Pollution/*adverse effects
Asthma/chemically induced/*epidemiology/*etiology
Child
Cross-Sectional Studies
*Environmental Exposure
Female
Humans
Male
Republic of Korea/epidemiology
Rhinitis, Allergic, Perennial/chemically induced/*epidemiology
Schools
Surveys and Questionnaires
Vehicle Emissions/analysis/toxicity
Air Pollutants
Vehicle Emissions
Figure
Cited by 3 articles
-
Current State of Research on the Risk of Morbidity and Mortality Associated with Air Pollution in Korea
Sanghyuk Bae, Ho-jang Kwon
Yonsei Med J. 2019;60(3):243-256. doi: 10.3349/ymj.2019.60.3.243.Asia Pacific Association of Allergy Asthma and Clinical Immunology White Paper 2020 on climate change, air pollution, and biodiversity in Asia-Pacific and impact on allergic diseases
Ruby Pawankar, Jiu-Yao Wang, I-Jen Wang, Francis Thien, Yoon-Seok Chang, Amir Hamzah Abdul Latiff, Takao Fujisawa, Luo Zhang, Bernard Yu-Hor Thong, Pantipa Chatchatee, Ting Fan Leung, Wasu Kamchaisatian, Iris Rengganis, Ho Joo Yoon, Sonomjamts Munkhbayarlakh, Marysia T. Recto, Anne Goh Eng Neo, Duy Le Pham, Le Thi Tuyet Lan, Janet Mary Davies, Jae Won Oh
Asia Pac Allergy. 2020;10(1):e11. doi: 10.5415/apallergy.2020.10.e11.Asia Pacific Association of Allergy Asthma and Clinical Immunology White Paper 2020 on climate change, air pollution, and biodiversity in Asia-Pacific and impact on allergic diseases
Ruby Pawankar, Jiu-Yao Wang, I-Jen Wang, Francis Thien, Yoon-Seok Chang, Amir Hamzah Abdul Latiff, Takao Fujisawa, Luo Zhang, Bernard Yu-Hor Thong, Pantipa Chatchatee, Ting Fan Leung, Wasu Kamchaisatian, Iris Rengganis, Ho Joo Yoon, Sonomjamts Munkhbayarlakh, Marysia T. Recto, Anne Goh Eng Neo, Duy Le Pham, Le Thi Tuyet Lan, Janet Mary Davies, Jae Won Oh
Asia Pac Allergy. 2020;10(1):. doi: 10.5415/apallergy.2020.10.e11.
Reference
-
1. Kim HH, Lee CS, Jeon JM, Yu SD, Lee CW, Park JH, et al. Analysis of the association between air pollution and allergic diseases exposure from nearby sources of ambient air pollution within elementary school zones in four Korean cities. Environ Sci Pollut Res Int. 2013; 20:4831–4846.
Article2. Vette A, Burke J, Norris G, Landis M, Batterman S, Breen M, et al. The near-road exposures and effects of urban air pollutants study (NEXUS): study design and methods. Sci Total Environ. 2013; 448:38–47.
Article3. Brauer M, Hoek G, Smit HA, de Jongste JC, Gerritsen J, Postma DS, et al. Air pollution and development of asthma, allergy and infections in a birth cohort. Eur Respir J. 2007; 29:879–888.
Article4. McConnell R, Islam T, Shankardass K, Jerrett M, Lurmann F, Gilliland F, et al. Childhood incident asthma and traffic-related air pollution at home and school. Environ Health Perspect. 2010; 118:1021–1026.
Article5. Brauer M, Hoek G, Van Vliet P, Meliefste K, Fischer PH, Wijga A, et al. Air pollution from traffic and the development of respiratory infections and asthmatic and allergic symptoms in children. Am J Respir Crit Care Med. 2002; 166:1092–1098.
Article6. Carlisle AJ, Sharp NC. Exercise and outdoor ambient air pollution. Br J Sports Med. 2001; 35:214–222.
Article7. Gauderman WJ, Vora H, McConnell R, Berhane K, Gilliland F, Thomas D, et al. Effect of exposure to traffic on lung development from 10 to 18 years of age: a cohort study. Lancet. 2007; 369:571–577.
Article8. Gauderman WJ, Gilliland GF, Vora H, Avol E, Stram D, McConnell R, et al. Association between air pollution and lung function growth in southern California children: results from a second cohort. Am J Respir Crit Care Med. 2002; 166:76–84.
Article9. Kang HY, Park CS, Bang HR, Sazonov V, Kim CJ. Effect of allergic rhinitis on the use and cost of health services by children with asthma. Yonsei Med J. 2008; 49:521–529.
Article10. Keuken M, Sanderson E, van Aalst R, Borken J, Schneider J. Contribution of traffic to levels of ambient air pollution in Europ. In : Krzyzanowski M, Kuna-Dibbert B, Schneider J, editors. Health effects of transport-related air pollution. 2005. Copenhagen, Denmark: WHO Regional Office Europe;p. 53–54.11. Nel A. Atmosphere. Air pollution-related illness: effects of particles. Science. 2005; 308:804–806.12. Canhaa N, Almeidab M, Freitasa M, Almeidaa SM, Wolterbeekc HT. Seasonal variation of total particulate matter and children respiratory diseases at Lisbon primary schools using passive methods. Procedia Environ Sci. 2011; 4:170–183.
Article13. Crilley LR, Ayoko GA, Jayaratne ER, Salimi F, Morawska L. Aerosol mass spectrometric analysis of the chemical composition of non-refractory PM(1) samples from school environments in Brisbane, Australia. Sci Total Environ. 2013; 458-460:81–89.
Article14. Hwang BF, Lee YL. Air pollution and prevalence of bronchitic symptoms among children in Taiwan. Chest. 2010; 138:956–964.
Article15. Kim JH, Kim JK, Son BK, Oh JE, Lim DH, Lee KH, et al. Effects of air pollutants on childhood asthma. Yonsei Med J. 2005; 46:239–244.
Article16. Longhini E, Fanari P, Giacomotti E, Palmulli P, Gabrione M, Gori D, et al. Lung function and methacholine responsiveness among adolescents in an air-polluted area. Respiration. 2004; 71:51–59.
Article17. Zhao Z, Zhang Z, Wang Z, Ferm M, Liang Y, Norbäck D. Asthmatic symptoms among pupils in relation to winter indoor and outdoor air pollution in schools in Taiyuan, China. Environ Health Perspect. 2008; 116:90–97.
Article18. Cheng YH, Shiu BT, Lin MH, Yan JW. Levels of black carbon and their relationship with particle number levels-observation at an urban roadside in Taipei City. Environ Sci Pollut Res Int. 2013; 20:1537–1545.
Article19. Gonzalez-Barcala FJ, Pertega S, Garnelo L, Castro TP, Sampedro M, Lastres JS, et al. Truck traffic related air pollution associated with asthma symptoms in young boys: a cross-sectional study. Public Health. 2013; 127:275–281.
Article20. Invernizzi G, Ruprecht A, Mazza R, De Marco C, Mocčnik G, Sioutas C, et al. Measurement of black carbon concentration as an indicator of air quality benefits of traffic restriction policies within the ecopass zone in Milan, Italy. Atmos Environ. 2011; 45:3522–3527.
Article21. Jacobson MZ. Short-term effects of controlling fossil-fuel soot, biofuel soot and gases, and methane on climate, Arctic ice, and air pollution health. J Geophys Res. 2010; 115:D14209.
Article22. Liu MM, Wang D, Zhao Y, Liu YQ, Huang MM, Liu Y, et al. Effects of outdoor and indoor air pollution on respiratory health of Chinese children from 50 kindergartens. J Epidemiol. 2013; 23:280–287.
Article23. Richmond-Bryant J, Bukiewicz L, Kalin R, Galarraga C, Mirer F. A multi-site analysis of the association between black carbon concentrations and vehicular idling, traffic, background pollution, and meteorology during school dismissals. Sci Total Environ. 2011; 409:2085–2093.
Article24. Buthbumrung N, Mahidol C, Navasumrit P, Promvijit J, Hunsonti P, Autrup H, et al. Oxidative DNA damage and influence of genetic polymorphisms among urban and rural schoolchildren exposed to benzene. Chem Biol Interact. 2008; 172:185–194.
Article25. Raysoni AU, Sarnat JA, Sarnat SE, Garcia JH, Holguin F, Luévano SF, et al. Binational school-based monitoring of traffic-related air pollutants in El Paso, Texas (USA) and Ciudad Juárez, Chihuahua (México). Environ Pollut. 2011; 159:2476–2486.
Article26. Richmond-Bryant J, Saganich C, Bukiewicz L, Kalin R. Associations of PM2.5 and black carbon concentrations with traffic, idling, background pollution, and meteorology during school dismissals. Sci Total Environ. 2009; 407:3357–3364.
Article27. Worldwide variation in prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and atopic eczema: ISAAC. The International Study of Asthma and Allergies in Childhood (ISAAC) Steering Committee. Lancet. 1998; 351:1225–1232.28. Kim HH, Kim CS, Lim YW, Suh MA, Shin DC. Indoor and outdoor air quality and its relation to allergic diseases among children: a case study at a primary school in Korea. Asian J Atmos Environ. 2010; 4:157–165.
Article29. Gruzieva O, Bergström A, Hulchiy O, Kull I, Lind T, Melén E, et al. Exposure to air pollution from traffic and childhood asthma until 12 years of age. Epidemiology. 2013; 24:54–61.
Article30. Boogaard H, Kos GPA, Weijers EP, Janssen NAH, Fischer PH, van der Zee SC, et al. Contrast in air pollution components between major streets and background locations: particulate matter mass, black carbon, elemental composition, nitrogen oxide and ultrafine particle number. Atmos Environ. 2011; 45:650–658.
Article31. Fruin S, Westerdahl D, Sax T, Sioutas C, Fine PM. Measurements and predictors of on-road ultrafine particle concentrations and associated pollutants in Los Angeles. Atmos Environ. 2008; 42:207–219.
Article32. Reche C, Querol X, Alastuey A, Viana M, Pey J, Moreno T, et al. New considerations for PM, Black Carbon and particle number concentration for air quality monitoring across different European cities. Atmos Chem Phys. 2011; 11:6207–6227.
Article33. Mastrangelo G, Clonfero E, Pavanello S, Fedeli U, Fadda E, Turato A, et al. Exposure to diesel exhaust enhances total IgE in non-atopic dockers. Int Arch Occup Environ Health. 2003; 76:63–68.
Article34. Lee YL, Lin YC, Hsiue TR, Hwang BF, Guo YL. Indoor and outdoor environmental exposures, parental atopy, and physician-diagnosed asthma in Taiwanese schoolchildren. Pediatrics. 2003; 112:e389.
Article35. Peters JM, Avol E, Navidi W, London SJ, Gauderman WJ, Lurmann F, et al. A study of twelve Southern California communities with differing levels and types of air pollution. I. Prevalence of respiratory morbidity. Am J Respir Crit Care Med. 1999; 159:760–767.
Article36. Annesi-Maesano I, Moreau D, Caillaud D, Lavaud F, Le Moullec Y, Taytard A, et al. Residential proximity fine particles related to allergic sensitisation and asthma in primary school children. Respir Med. 2007; 101:1721–1729.
Article37. Mejía JF, Choy SL, Mengersen K, Morawska L. Methodology for assessing exposure and impacts of air pollutants in school children: data collection, analysis and health effects - a literature review. Atmos Environ. 2011; 45:813–823.
Article38. Suh M, Kim HH, Choi DP, Kim KW, Sohn MH, Ha KH, et al. Association between body mass index and asthma symptoms among Korean children: a Nation-Wide Study. J Korean Med Sci. 2011; 26:1541–1547.
Article39. Montefort S, Ellul P, Montefort M, Caruana S, Grech V, Agius Muscat H. The effect of cigarette smoking on allergic conditions in Maltese children (ISAAC). Pediatr Allergy Immunol. 2012; 23:472–478.
Article40. Suh M, Kim HH, Sohn MH, Kim KE, Kim C, Shin DC. Prevalence of allergic diseases among Korean school-age children: a Nationwide Cross-Sectional Questionnaire Study. J Korean Med Sci. 2011; 26:332–338.
Article41. Ferreira F, Wolf M, Wallner M. Molecular approach to allergy diagnosis and therapy. Yonsei Med J. 2014; 55:839–852.
Article42. Lee JU, Kim JD, Park CS. Gene-environment interactions in asthma: genetic and epigenetic effects. Yonsei Med J. 2015; 56:877–886.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of air pollution on acute exacerbation of adult asthma in Seoul, Korea
- Near-Road Exposure and Impact of Air Pollution on Allergic Diseases in Elementary School Children: A Cross-Sectional Study
- Effect of Traffic-Related Air Pollution on Allergic Disease: Results of the Children's Health and Environmental Research
- Traffic-Related Air Pollution and Allergic Diseases
- Air pollution and childhood allergic disease