Korean J Radiol.
2007 Feb;8(1):9-14. 10.3348/kjr.2007.8.1.9.
Assessment of Lymph Node Metastases by Contrast-Enhanced MR Imaging in a Head and Neck Cancer Model
- Affiliations
-
- 1Department of Veterinary Radiology, Chonbuk National University College of Veterinary Medicine, Jeonju City, Korea. moonwk@radcom.snu.ac.kr
- 2Department of Radiology, Seoul National University College of Medicine and The Institute of Radiation Medicine, Seoul National University Medical Research Center, Seoul, Korea.
- 3Institute of Life Science and Biotechnology, Yonsei University, Korea.
- KMID: 753860
- DOI: http://doi.org/10.3348/kjr.2007.8.1.9
Abstract
OBJECTIVE
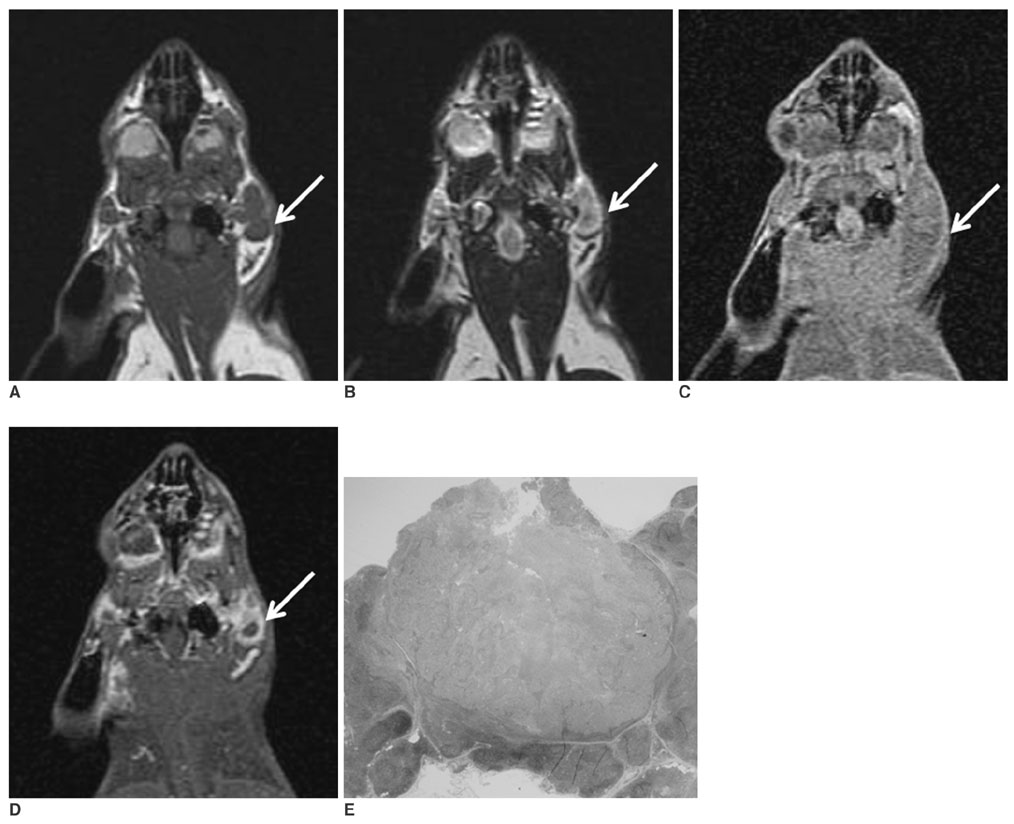
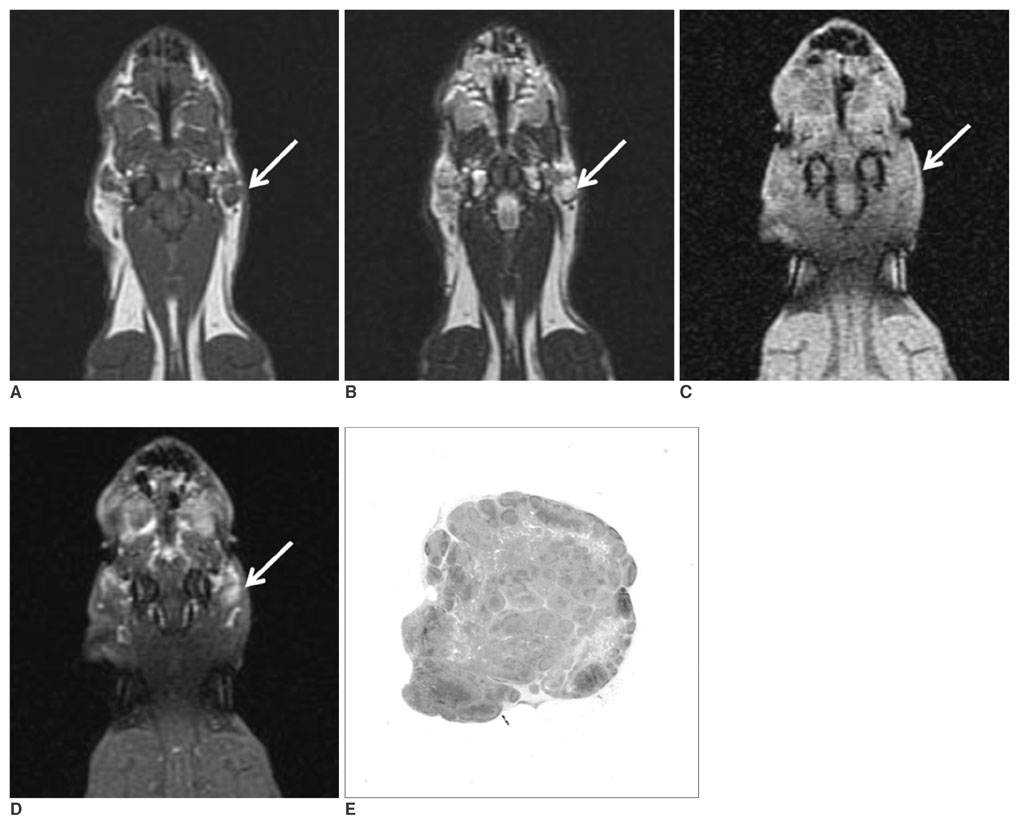
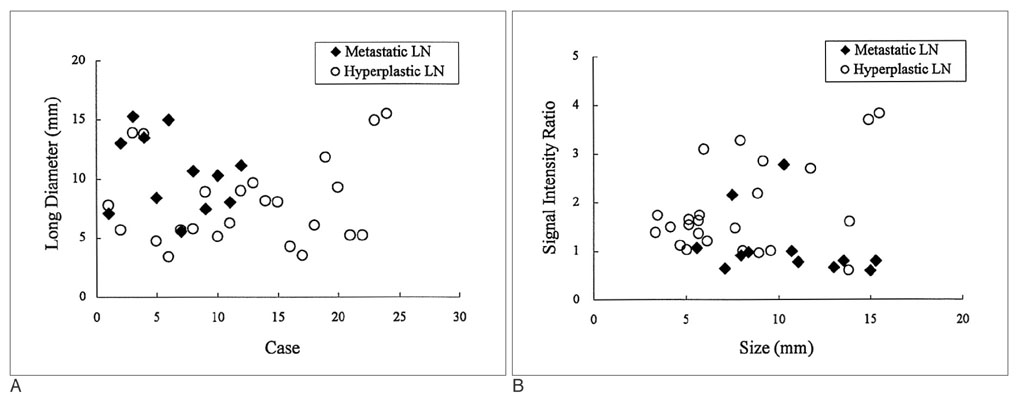
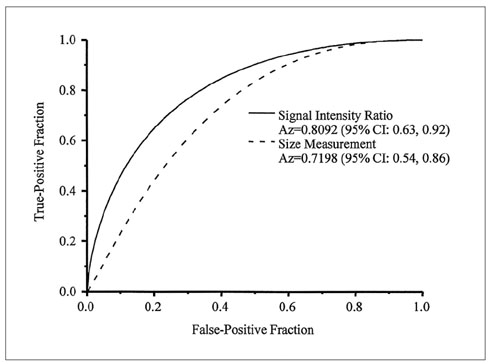
We wanted to investigate the accuracy of contrast-enhanced MR imaging for the detection of lymph node metastases in a head and neck cancer rabbit model. MATERIALS AND METHODS: The metastatic lymph node model we used was created by inoculating VX2 tumors into the auricles of six New Zealand White rabbits. T1-weighted MR images were obtained before and after injecting gadopentetate dimeglumine at three weeks after tumor cell inoculation. The sizes, signal intensity ratios (i.e., the postcontrast signal intensities of the affected nodes relative to the adjacent muscle) and the enhancement patterns of 36 regional lymph nodes (parotid and caudal mandibular nodes) were evaluated on MR images and then compared with the histopathologic findings. RESULTS: No statistical difference was found between the sizes of 12 metastatic (10.5+/-3.2 mm) and 24 hyperplastic (8.0+/-3.6 mm) lymph nodes (p > 0.05). On the contrast-enhanced T1-weighted MR images, nine metastatic and four hyperplastic lymph nodes had peripheral high and central low signal intensity, whereas three metastatic and 20 hyperplastic lymph nodes had homogeneous high signal intensity. Using a signal intensity ratio less than one as a diagnostic criterion for a metastatic lymph node, the sensitivity, specificity and positive and negative predictive values of the enhanced MR images were 75% (9/12), 83% (20/24), 69% (9/13) and 87% (20/23), respectively, with areas under receiver-operating-characteristic curve values of 0.81. CONCLUSION: This experimental study confirms that metastatic and hyperplastic lymph nodes can be differentiated using MR images on the basis of the contrast uptake patterns, but that they cannot be differentiated using any particular size criteria.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Prognostic Value of Radiologic Extranodal Extension in Human Papillomavirus-Related Oropharyngeal Squamous Cell Carcinoma
Boeun Lee, Young Jun Choi, Seon-Ok Kim, Yoon Se Lee, Jung Yong Hong, Jung Hwan Baek, Jeong Hyun Lee
Korean J Radiol. 2019;20(8):1266-1274. doi: 10.3348/kjr.2018.0742.
Reference
-
1. Golder WA. Lymph node diagnosis in oncologic imaging: a dilemma still waiting to be solved. Onkologie. 2004. 27:194–199.2. O'Brien CJ, McNeil EB, McMahon JD, Pathak I, Lauer CS, Jackson MA. Significance of clinical stage, extent of surgery, and pathologic findings in metastatic cutaneous squamous carcinoma of the parotid gland. Head Neck. 2002. 24:417–422.3. Kau RJ, Alexiou C, Stimmer H, Arnold W. Diagnostic procedures for detection of lymph node metastases in cancer of the larynx. J Otorhinolaryngol Relat Spec. 2000. 62:199–203.4. Herborn CU, Vogt FM, Lauenstein TC, Goyen M, Dirsch O, Corot C, et al. Assessment of normal, inflammatory, and tumor-bearing lymph nodes with contrast-enhanced interstitial magnetic resonance lymphography: preliminary results in rabbits. J Magn Reson Imaging. 2003. 18:328–335.5. Kim SH, Kim SC, Choi BI, Han MC. Uterine cervical carcinoma: evaluation of pelvic lymph node metastasis with MR imaging. Radiology. 1994. 190:807–811.6. Moghimi SM, Bonnemain B. Subcutaneous and intravenous delivery of diagnostic agents to the lymphatic system: applications in lymphoscintigraphy and indirect lymphography. Adv Drug Deliv Rev. 1999. 37:295–312.7. Clement O, Luciani A. Imaging the lymphatic system: possibilities and clinical applications. Eur Radiol. 2004. 14:1498–1507.8. Misselwitz B, Platzek J, Weinmann HJ. Early MR lymphography with gadofluorine M in rabbits. Radiology. 2004. 231:682–688.9. Ruehm SG, Schroeder T, Debatin JF. Interstitial MR lymphography with gadoterate meglumine: initial experience in humans. Radiology. 2001. 220:816–821.10. Staatz G, Nolte-Ernsting CC, Adam GB, Grosskortenhaus S, Misselwitz B, Bucker A, et al. Interstitial T1-weighted MR lymphography: lipophilic perfluorinated gadolinium chelates in pigs. Radiology. 2001. 220:129–134.11. Dunne AA, Mandic R, Ramaswamy A, Plehn S, Schulz S, Lippert BM, et al. Lymphogenic metastatic spread of auricular VX2 carcinoma in New Zealand white rabbits. Anticancer Res. 2002. 22:3273–3279.12. Dunne AA, Plehn S, Schulz S, Levermann A, Ramaswamy A, Lippert BM, et al. Lymph node topography of the head and neck in New Zealand White rabbits. Lab Anim. 2003. 37:37–43.13. van Es RJ, Franssen O, Dullens HF, Bernsen MR, Bosman F, Hennink WE, et al. The VX2 carcinoma in the rabbit auricle as an experimental model for intra-arterial embolization of head and neck squamous cell carcinoma with dextran microspheres. Lab Anim. 1999. 33:175–184.14. Metz CE. Some practical issues of experimental design and data analysis in radiological ROC studies. Invest Radiol. 1989. 24:234–245.15. ROCKIT by Kurt Rossmann Laboratories. Accessed June 10, 2005. Department of Radiology, University of Chicago;Available at www.radiology.uchicago.edu/krl/KRL_ROC software _index.htm.16. Som PM. Detection of metastasis in cervical lymph nodes: CT and MR criteria and differential diagnosis. AJR Am J Roentgenol. 1992. 158:961–969.17. van den Brekel MW, Stel HV, Castelijns JA, Nauta JJ, van der Waal I, Valk J, et al. Cervical lymph node metastasis: assessment of radiologic criteria. Radiology. 1990. 177:379–384.18. Fischbein NJ, Noworolski SM, Henry RG, Kaplan MJ, Dillon WP, Nelson SJ. Assessment of metastatic cervical adenopathy using dynamic contrast-enhanced MR imaging. AJNR Am J Neuroradiol. 2003. 24:301–311.19. Anzai Y, Piccoli CW, Outwater EK, Stanford W, Bluemke DA, Nurenberg P, et al. Evaluation of neck and body metastases to nodes with ferumoxtran 10-enhanced MR imaging: phase III safety and efficacy study. Radiology. 2003. 228:777–788.20. Schoder H, Yeung HW, Gonen M, Kraus D, Larson SM. Head and neck cancer: clinical usefulness and accuracy of PET/CT image fusion. Radiology. 2004. 231:65–72.21. Choi SH, Moon WK, Hong JH, Son KR, Cho N, Kwon BJ, et al. Lymph node metastasis: ultrasmall superparamagnetic iron oxide-enhanced MR Imaging versus PET/CT in a rabbit model. Radiology. 2007. 242:137–143.22. Choi SH, Han MH, Moon WK, Son KR, Won JK, Kim JH, et al. Cervical lymph node metastases: MR imaging of gadoffluorine M and monocrystalline iron oxide nanoparticle 47 in a rabbit model of head and neck cancer. Radiology. 2006. 241:753–762.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pelvic Lymph Node Evaluation in Uterine Cervical Carcinoma Using Contrast Enhanced MR Imaging
- Contrast-Enhanced MR Imaging of Lymph Nodes in Cancer Patients
- Ultrasonography for Staging Axillary Lymph Node in Breast Cancer Patients
- A Clinical Review of Lymph Node Metastases for Papillary Thyroid Cancer
- Regional Lymph Node Metastasis in Papillary Thyroid Cancer