Ann Hepatobiliary Pancreat Surg.
2024 Nov;28(4):508-515. 10.14701/ahbps.24-121.
Perioperative outcomes of robot-assisted pancreatoduodenectomy (PD) and totally laparoscopic PD after overcoming learning curves with comparison of oncologic outcomes between open PD and minimally invasive PD
- Affiliations
-
- 1Department of Surgery and Cancer Research Institute, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- 2Department of Surgery and Robot Surgery Center, Myongju Hospital, Yongin, Korea
- 3Department of Surgery and Division of Hepatobiliary and Pancreatic Surgery, Asan Medical Center, Seoul, Korea
- 4Department of Surgery, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea
- 5Department of Surgery, Incheon St. Mary’s Hospital, Incheon, Korea
- 6Department of Surgery, Chung-Ang University Gwangmyeong Hospital, Gwangmyeong, Korea
- 7Department of Surgery, National Medical Center, Seoul, Korea
- KMID: 2561584
- DOI: http://doi.org/10.14701/ahbps.24-121
Abstract
- Backgrounds/Aims
Minimally invasive pancreatoduodenectomy (MIPD), such as totally laparoscopic pancreatoduodenectomy (TLPD) or robot-assisted pancreatoduodenectomy (RAPD), is increasingly performed worldwide. This study aimed to compare the perioperative outcomes of TLPD and RAPD, and compare the oncologic outcomes between MIPD and open pancreatoduodenectomy (OPD) for malignant disease.
Methods
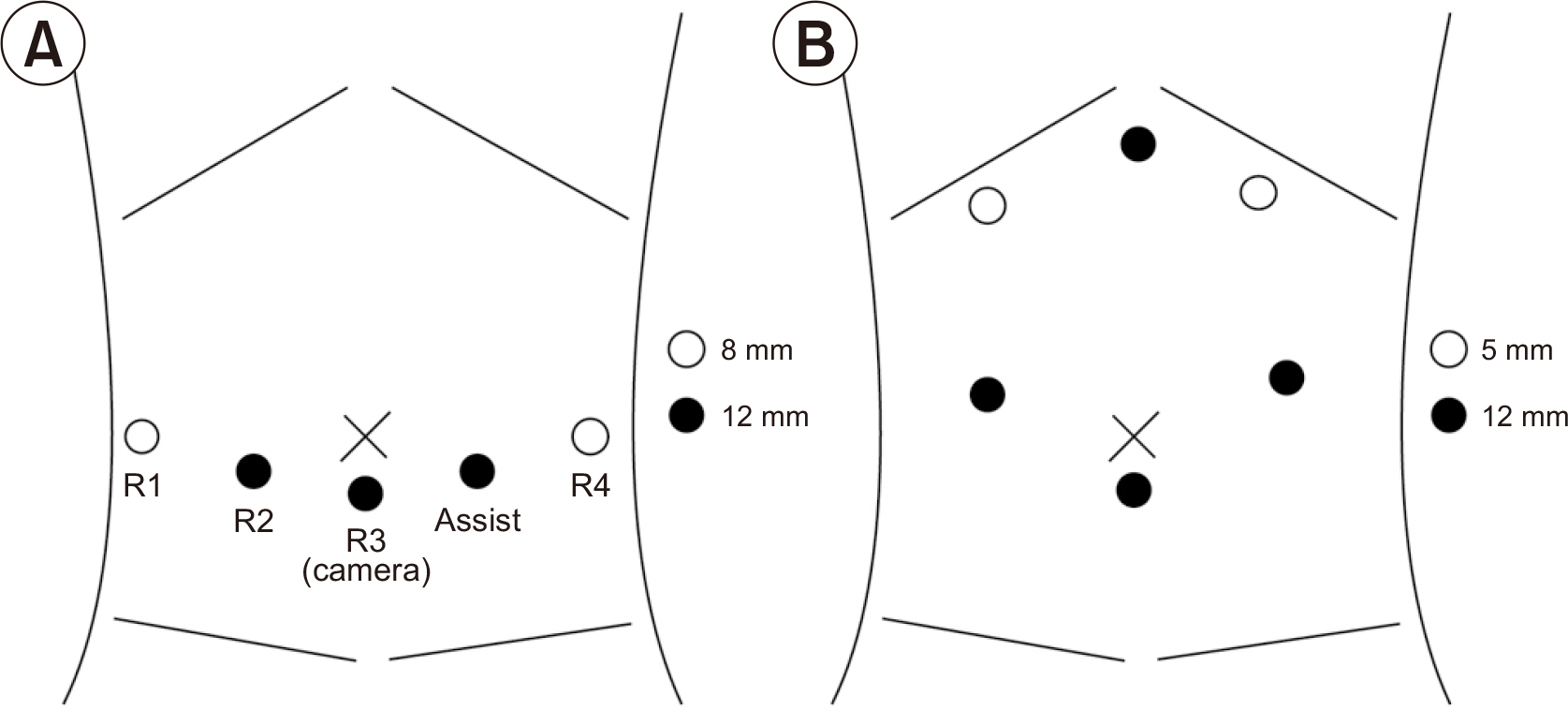
This retrospective study was conducted at two hospitals that followed similar oncological surgical principles, including the extent of resection. RAPD was performed at Seoul National University Hospital, and TLPD at Seoul National University Bundang Hospital. Patient demographics, perioperative outcomes, and oncological outcomes were analyzed. Propensity score matching (PSM) analysis was performed to compare oncologic outcomes between MIPD and OPD.
Results
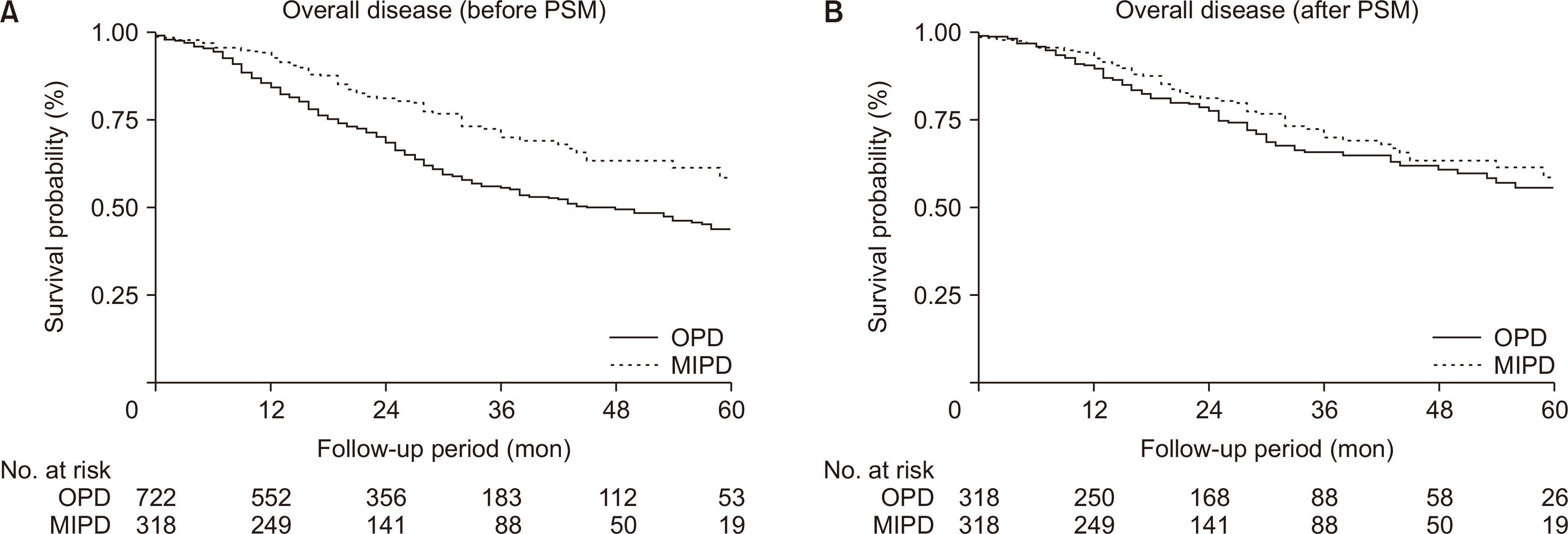
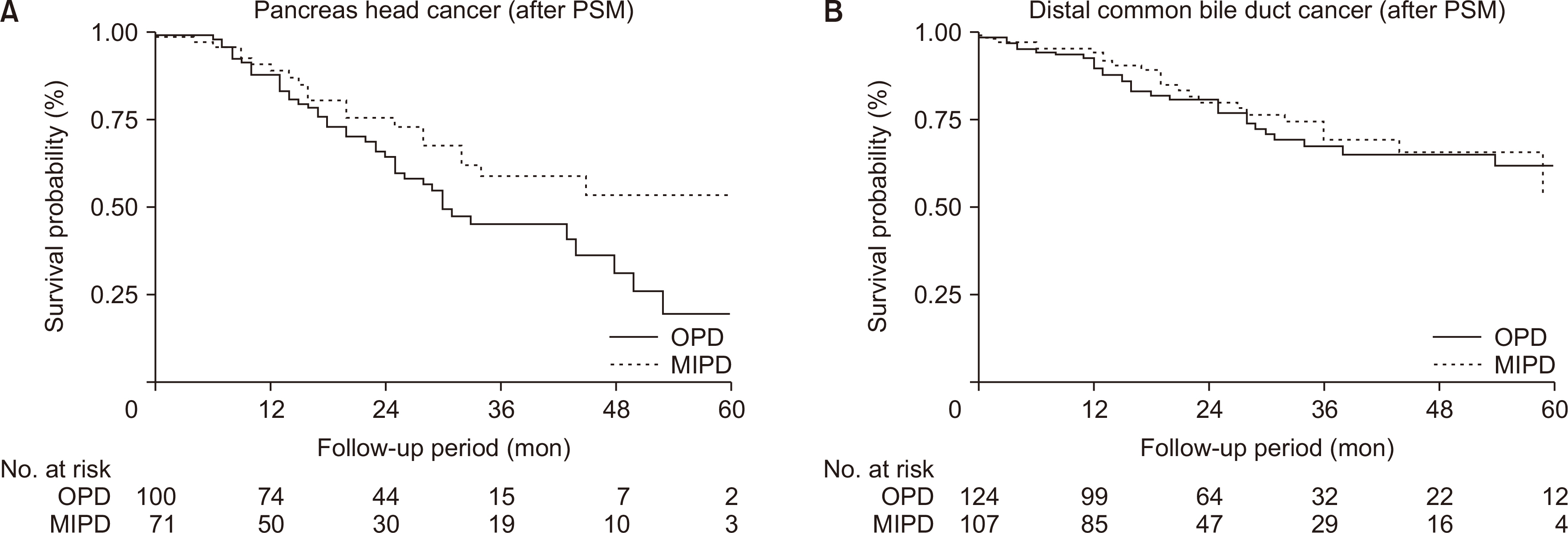
Between 2015 and 2020, 332 RAPD and 178 TLPD were performed. The rates of Clavian–Dindo grade ≥ 3 complications (19.3% vs. 20.2%, p = 0.816), clinically relevant postoperative pancreatic fistula (9.9% vs. 11.8%, p = 0.647), and open conversions (6.6% vs. 10.5%, p = 0.163) were comparable between the two groups. The mean operation time (341 minutes vs. 414 minutes, p < 0.001) and postoperative hospital stay were shorter in the RAPD group (11 days vs. 14 days, p = 0.034). After PSM, the 5-year overall survival rate was comparable between MIPD and OPD for overall malignant disease (58.4% vs. 55.5%, p = 0.180).
Conclusions
Both RAPD and TLPD are safe and feasible, and MIPD has clinical outcomes that are comparable to those of OPD. Although RAPD exhibits some advantages, its perioperative outcomes are similar to those associated with TLPD. A surgical method may be selected based on the convenience of surgical movements, medical costs, and operator experience.
Figure
Reference
-
References
1. Byun Y, Choi YJ, Han Y, Kang JS, Kim H, Kwon W, et al. 2022; Outcomes of 5000 pancreatectomies in Korean single referral center and literature reviews. J Hepatobiliary Pancreat Sci. 29:1327–1335. DOI: 10.1002/jhbp.933. PMID: 33636051.2. Torphy RJ, Friedman C, Halpern A, Chapman BC, Ahrendt SS, McCarter MM, et al. 2019; Comparing short-term and oncologic outcomes of minimally invasive versus open pancreaticoduodenectomy across low and high volume centers. Ann Surg. 270:1147–1155. DOI: 10.1097/SLA.0000000000002810. PMID: 29771723.3. Lee B, Yoon YS, Kang CM, Choi M, Lee JS, Hwang HK, et al. 2021; Fistula risk score-adjusted comparison of postoperative pancreatic fistula following laparoscopic vs open pancreatoduodenectomy. J Hepatobiliary Pancreat Sci. 28:1089–1097. DOI: 10.1002/jhbp.866. PMID: 33174394.4. Song KB, Kim SC, Hwang DW, Lee JH, Lee DJ, Lee JW, et al. 2015; Matched case-control analysis comparing laparoscopic and open pylorus-preserving pancreaticoduodenectomy in patients with periampullary tumors. Ann Surg. 262:146–155. DOI: 10.1097/SLA.0000000000001079. PMID: 25563866.5. van Hilst J, de Rooij T, Bosscha K, Brinkman DJ, van Dieren S, Dijkgraaf MG, et al. 2019; Laparoscopic versus open pancreatoduodenectomy for pancreatic or periampullary tumours (LEOPARD-2): a multicentre, patient-blinded, randomised controlled phase 2/3 trial. Lancet Gastroenterol Hepatol. 4:199–207. DOI: 10.1016/S2468-1253(19)30004-4. PMID: 30685489.6. Giulianotti PC, Coratti A, Angelini M, Sbrana F, Cecconi S, Balestracci T, et al. 2003; Robotics in general surgery: personal experience in a large community hospital. Arch Surg. 138:777–784. DOI: 10.1001/archsurg.138.7.777. PMID: 12860761.7. Napoli N, Kauffmann EF, Menonna F, Perrone VG, Brozzetti S, Boggi U. 2016; Indications, technique, and results of robotic pancreatoduodenectomy. Updates Surg. 68:295–305. DOI: 10.1007/s13304-016-0387-7. PMID: 27614901.8. Kim HS, Han Y, Kang JS, Kim H, Kim JR, Kwon W, et al. 2018; Comparison of surgical outcomes between open and robot-assisted minimally invasive pancreaticoduodenectomy. J Hepatobiliary Pancreat Sci. 25:142–149. DOI: 10.1002/jhbp.522. PMID: 29117639.9. McMillan MT, Zureikat AH, Hogg ME, Kowalsky SJ, Zeh HJ, Sprys MH, et al. 2017; A propensity score-matched analysis of robotic vs open pancreatoduodenectomy on incidence of pancreatic fistula. JAMA Surg. 152:327–335. DOI: 10.1001/jamasurg.2016.4755. PMID: 28030724. PMCID: PMC5470429.10. Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, et al. 2017; The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery. 161:584–591. DOI: 10.1016/j.surg.2016.11.014. PMID: 28040257.11. Kwon W, He J, Higuchi R, Son D, Lee SY, Kim J, et al. 2018; Multinational validation of the American Joint Committee on Cancer 8th edition pancreatic cancer staging system in a pancreas head cancer cohort. J Hepatobiliary Pancreat Sci. 25:418–427. DOI: 10.1002/jhbp.577. PMID: 30118171.12. Jang JY, Kang JS, Han Y, Heo JS, Choi SH, Choi DW, et al. 2017; Long-term outcomes and recurrence patterns of standard versus extended pancreatectomy for pancreatic head cancer: a multicenter prospective randomized controlled study. J Hepatobiliary Pancreat Sci. 24:426–433. DOI: 10.1002/jhbp.465. PMID: 28514000.13. Kim H, Kim JR, Han Y, Kwon W, Kim SW, Jang JY. 2017; Early experience of laparoscopic and robotic hybrid pancreaticoduodenectomy. Int J Med Robot. 13:e1814. DOI: 10.1002/rcs.1814. PMID: 28276146.14. Kim S, Yoon YS, Han HS, Cho JY, Choi Y, Lee B. 2021; Evaluation of a single surgeon's learning curve of laparoscopic pancreaticoduodenectomy: risk-adjusted cumulative summation analysis. Surg Endosc. 35:2870–2878. DOI: 10.1007/s00464-020-07724-z. PMID: 32548654.15. Coppola A, Stauffer JA, Asbun HJ. 2016; Laparoscopic pancreatoduodenectomy: current status and future directions. Updates Surg. 68:217–224. DOI: 10.1007/s13304-016-0402-z. PMID: 27815783.16. Gagner M, Pomp A. 1994; Laparoscopic pylorus-preserving pancreatoduodenectomy. Surg Endosc. 8:408–410. DOI: 10.1007/BF00642443. PMID: 7915434.17. Choi M, Hwang HK, Lee WJ, Kang CM. 2021; Total laparoscopic pancreaticoduodenectomy in patients with periampullary tumors: a learning curve analysis. Surg Endosc. 35:2636–2644. DOI: 10.1007/s00464-020-07684-4. PMID: 32495184.18. de Rooij T, van Hilst J, Topal B, Bosscha K, Brinkman DJ, Gerhards MF, et al. 2019; Outcomes of a multicenter training program in laparoscopic pancreatoduodenectomy (LAELAPS-2). Ann Surg. 269:344–350. DOI: 10.1097/SLA.0000000000002563. PMID: 29099400.19. Watkins AA, Kent TS, Gooding WE, Boggi U, Chalikonda S, Kendrick ML, et al. 2018; Multicenter outcomes of robotic reconstruction during the early learning curve for minimally-invasive pancreaticoduodenectomy. HPB (Oxford). 20:155–165. DOI: 10.1016/j.hpb.2017.08.032. PMID: 28966031.20. Kim H, Choi SH, Jang JY, Choi M, Lee JH, Kang CM. 2022; Multicenter comparison of totally laparoscopic and totally robotic pancreaticoduodenectomy: propensity score and learning curve-matching analyses. J Hepatobiliary Pancreat Sci. 29:311–321. DOI: 10.1002/jhbp.1078. PMID: 34773395.21. Tyutyunnik P, Klompmaker S, Lombardo C, Lapshyn H, Menonna F, Napoli N, et al. 2022; Learning curve of three European centers in laparoscopic, hybrid laparoscopic, and robotic pancreatoduodenectomy. Surg Endosc. 36:1515–1526. DOI: 10.1007/s00464-021-08439-5. PMID: 33825015.22. Leijte E, de Blaauw I, Van Workum F, Rosman C, Botden S. 2020; Robot assisted versus laparoscopic suturing learning curve in a simulated setting. Surg Endosc. 34:3679–3689. DOI: 10.1007/s00464-019-07263-2. PMID: 31754849. PMCID: PMC7326898.23. Aboudou T, Li M, Zhang Z, Wang Z, Li Y, Feng L, et al. 2022; Laparoscopic versus robotic hepatectomy: a systematic review and meta-analysis. J Clin Med. 11:5831. DOI: 10.3390/jcm11195831. PMID: 36233697. PMCID: PMC9571364.24. Khorgami Z, Li WT, Jackson TN, Howard CA, Sclabas GM. 2019; The cost of robotics: an analysis of the added costs of robotic-assisted versus laparoscopic surgery using the National Inpatient Sample. Surg Endosc. 33:2217–2221. DOI: 10.1007/s00464-018-6507-3. PMID: 30327915.25. Gerber MH, Delitto D, Crippen CJ, George TJ Jr, Behrns KE, Trevino JG, et al. 2017; Analysis of the cost effectiveness of laparoscopic pancreatoduodenectomy. J Gastrointest Surg. 21:1404–1410. DOI: 10.1007/s11605-017-3466-2. PMID: 28567575. PMCID: PMC6032973.26. Kowalsky SJ, Zenati MS, Steve J, Esper SA, Lee KK, Hogg ME, et al. 2019; A combination of robotic approach and ERAS pathway optimizes outcomes and cost for pancreatoduodenectomy. Ann Surg. 269:1138–1145. DOI: 10.1097/SLA.0000000000002707. PMID: 31082913.27. Klompmaker S, van Hilst J, Wellner UF, Busch OR, Coratti A, D'Hondt M, et al. 2020; Outcomes after minimally-invasive versus open pancreatoduodenectomy: a pan-european propensity score matched study. Ann Surg. 271:356–363. DOI: 10.1097/SLA.0000000000002850. PMID: 29864089.28. Croome KP, Farnell MB, Que FG, Reid-Lombardo KM, Truty MJ, Nagorney DM, et al. 2014; Total laparoscopic pancreaticoduodenectomy for pancreatic ductal adenocarcinoma: oncologic advantages over open approaches? Ann Surg. 260:633–638. DOI: 10.1097/SLA.0000000000000937. PMID: 25203880.29. Kauffmann EF, Napoli N, Menonna F, Iacopi S, Lombardo C, Bernardini J, et al. 2019; A propensity score-matched analysis of robotic versus open pancreatoduodenectomy for pancreatic cancer based on margin status. Surg Endosc. 33:234–242. DOI: 10.1007/s00464-018-6301-2. PMID: 29943061.30. Kim SH, Lee B, Hwang HK, Lee JS, Han HS, Lee WJ, et al. 2022; Comparison of postoperative complications and long-term oncological outcomes in minimally invasive versus open pancreatoduodenectomy for distal cholangiocarcinoma: a propensity score-matched analysis. J Hepatobiliary Pancreat Sci. 29:329–337. DOI: 10.1002/jhbp.1067. PMID: 34717038.31. Yoo D, Song KB, Lee JW, Hwang K, Hong S, Shin D, et al. 2020; A comparative study of laparoscopic versus open pancreaticoduodenectomy for ampulla of vater carcinoma. J Clin Med. 9:2214. DOI: 10.3390/jcm9072214. PMID: 32668683. PMCID: PMC7408711.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Impact of conversion at time of minimally invasive pancreaticoduodenectomy on perioperative and long-term outcomes: Review of the National Cancer Database
- Low-cost model for pancreatojejunostomy simulation in minimally invasive pancreatoduodenectomy
- External pancreatic ductal stenting in minimally invasive pancreatoduodenectomy: How to do it?
- Effectiveness and stability of robot-assisted anastomosis in minimally invasive pancreaticoduodenectomy
- The duodenal window approach to pancreatoduodenectomy