Ann Surg Treat Res.
2021 Jun;100(6):329-337. 10.4174/astr.2021.100.6.329.
Effectiveness and stability of robot-assisted anastomosis in minimally invasive pancreaticoduodenectomy
- Affiliations
-
- 1Division of Hepato-biliary and Pancreas Surgery, Department of Surgery, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2516226
- DOI: http://doi.org/10.4174/astr.2021.100.6.329
Abstract
- Purpose
Reconstruction using robotic assistance in pancreaticoduodenectomy (PD) was expected to be an effective means to overcome the limitations of laparoscopic surgery. To our knowledge, few comparative reports exist on the outcomes of totally laparoscopic PD (TLPD) and robot-assisted laparoscopic PD (RLPD). This retrospective study aimed to analyze the surgical results of TLPD and RLPD in a high-volume pancreatic center.
Methods
We analyzed the surgical results of consecutive patients who underwent a minimally invasive PD for malignant or benign periampullary lesions between January 2016 and May 2020. Forty-three TLPD patients and 49 RLPD patients were enrolled.
Results
There were no significant differences in the demographic characteristics between the 2 groups except for tumor size, which was significantly larger in the RLPD group than in the TLPD group (mean, 3.1 cm vs. 2.5 cm; P = 0.035). The RLPD group had shorter whole operative times (mean, 400.4 minutes vs. 352.2 minutes; P = 0.003) and shorter anastomosis times than the TLPD group (mean, 94.5 minutes vs. 54.9 minutes; P < 0.001). There was no significant difference between the 2 groups in the rate of pancreatic fistulas, morbidity, and mortality. However, a significantly lower wound infection rate was found in the RLPD group relative to the TLPD group (0% vs. 9.3%, P = 0.038).
Conclusion
RLPD showed the advantage of reducing the operation time compared to TLPD as well as technical feasibility and safety.
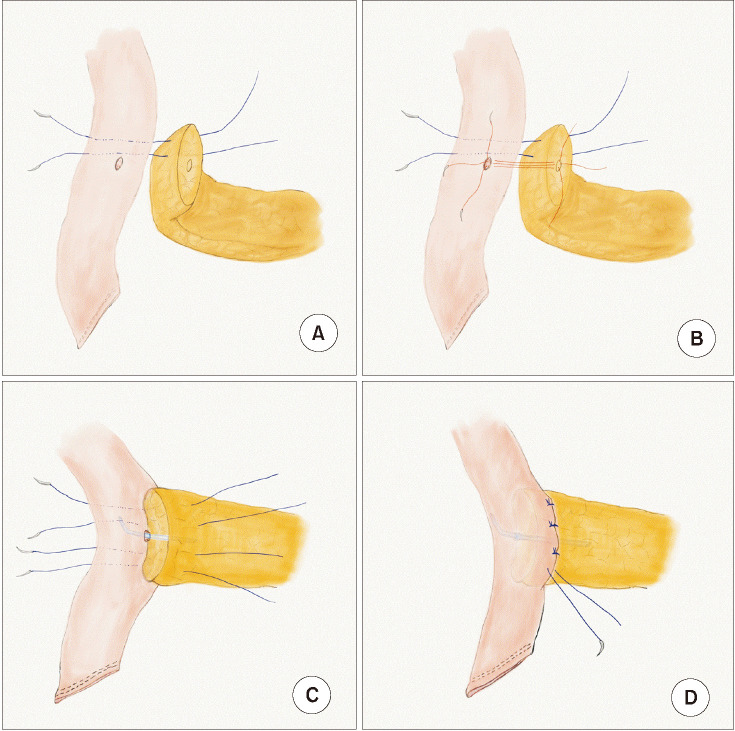
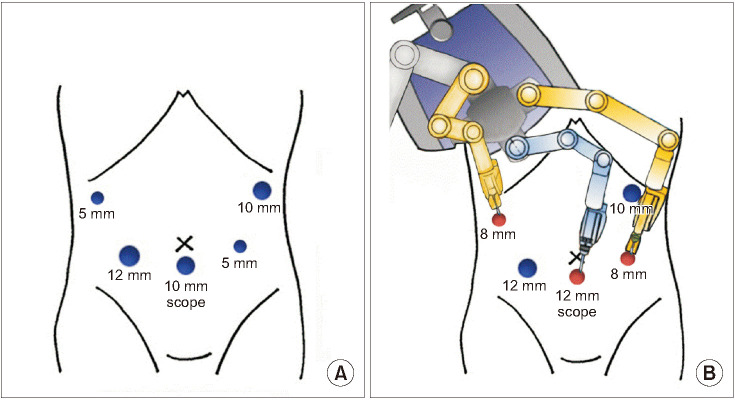
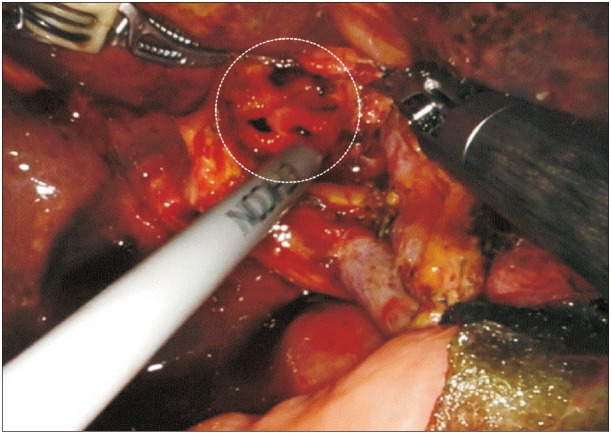
Figure
Reference
-
1. Zhang T, Zhao ZM, Gao YX, Lau WY, Liu R. The learning curve for a surgeon in robot-assisted laparoscopic pancreaticoduodenectomy: a retrospective study in a high-volume pancreatic center. Surg Endosc. 2019; 33:2927–2933. PMID: 30483970.
Article2. Chen K, Pan Y, Liu XL, Jiang GY, Wu D, Maher H, et al. Minimal ly invasive pancreaticoduodenectomy for periampullary disease: a comprehensive review of literature and meta-analysis of outcomes compared with open surgery. BMC Gastroenterol. 2017; 17:120. PMID: 29169337.
Article3. Kostakis ID, Sran H, Uwechue R, Chandak P, Olsburgh J, Mamode N, et al. Comparison between robotic and laparoscopic or open anastomoses: a systematic review and meta-analysis. Robot Surg. 2019; 6:27–40. PMID: 31921934.4. Liu R, Wakabayashi G, Palanivelu C, Tsung A, Yang K, Goh BK, et al. International consensus statement on robotic pancreatic surgery. Hepatobiliary Surg Nutr. 2019; 8:345–360. PMID: 31489304.
Article5. Watkins AA, Kent TS, Gooding WE, Boggi U, Chalikonda S, Kendrick ML, et al. Multicenter outcomes of robotic reconstruction during the early learning curve for minimally-invasive pancreaticoduodenectomy. HPB (Oxford). 2018; 20:155–165. PMID: 28966031.
Article6. Giulianotti PC, Coratti A, Angelini M, Sbrana F, Cecconi S, Balestracci T, et al. Robotics in general surgery: personal experience in a large community hospital. Arch Surg. 2003; 138:777–784. PMID: 12860761.7. Kim HS, Han Y, Kang JS, Kim H, Kim JR, Kwon W, et al. Comparison of surg i c a l out comes b e twe en open and robot-assisted minimally invasive pancreaticoduodenectomy. J Hepatobiliary Pancreat Sci. 2018; 25:142–149. PMID: 29117639.8. Zhao W, Liu C, Li S, Geng D, Feng Y, Sun M. Safety and efficacy for robot-assisted versus open pancreaticoduodenectomy and distal pancreatectomy: a systematic review and meta-analysis. Surg Oncol. 2018; 27:468–478. PMID: 30217304.
Article9. Coratti A, Di Marino M, Coratti F, Baldoni G, Guerra F, Amore Bonapasta S, et al. Initial experience with robotic pancreatic surgery: technical feasibility and oncological implications. Surg Laparosc Endosc Percutan Tech. 2016; 26:31–37. PMID: 26766310.10. Kaspy MS, Hassan GM, Paquin SC, Sahai AV. An assessment of the yield of EUS in patients referred for dilated common bile duct and normal liver function tests. Endosc Ultrasound. 2019; 8:318–320. PMID: 31249161.
Article11. Marino MV, Podda M, Pisanu A, di Saverio S, Fleitas MG. Robotic-assisted pancreaticoduodenectomy: technique description and performance evaluation after 60 cases. Surg Laparosc Endosc Percutan Tech. 2020; 30:156–163. PMID: 31923162.
Article12. Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, et al. The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery. 2017; 161:584–591. PMID: 28040257.13. Tol JA, Gouma DJ, Bassi C, Dervenis C, Montorsi M, Adham M, et al. Definition of a standard lymphadenectomy in surgery for pancreatic ductal adenocarcinoma: a consensus statement by the International Study Group on Pancreatic Surgery (ISGPS). Surgery. 2014; 156:591–600. PMID: 25061003.
Article14. Kawakatsu S, Inoue Y, Mise Y, Ishizawa T, Ito H, Takahashi Y, et al. Comparison of pancreatojejunostomy techniques in patients with a soft pancreas: Kakita anastomosis and Blumgart anastomosis. BMC Surg. 2018; 18:88. PMID: 30355352.
Article15. Karim SA, Abdulla KS, Abdulkarim QH, Rahim FH. The outcomes and complications of pancreaticoduodenectomy (Whipple procedure): cross sectional study. Int J Surg. 2018; 52:383–387. PMID: 29438817.
Article16. Corcione F, Esposito C, Cuccurullo D, Settembre A, Miranda N, Amato F, et al. Advantages and limits of robot-assisted laparoscopic surgery: preliminary experience. Surg Endosc. 2005; 19:117–119. PMID: 15549629.
Article17. Zhang YH, Zhang CW, Hu ZM, Hong DF. Pancreatic cancer: open or minimally invasive surgery? World J Gastroenterol. 2016; 22:7301–7310. PMID: 27621576.
Article18. Zhang Y, Hong D, Zhang C, Hu Z. Total laparoscopic versus robot-assisted laparoscopic pancreaticoduodenectomy. Biosci Trends. 2018; 12:484–490. PMID: 30473556.
Article19. Kim H, Kim JR, Han Y, Kwon W, Kim SW, Jang JY. Early experience of laparoscopic and robotic hybrid pancreaticoduodenectomy. Int J Med Robot. 2017; 13.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Robotic-assisted resection of proximal jejunal ischemic stricture and intracorporeal robot-sewn anastomosis
- Robot-Assisted Colorectal Surgery
- Anterior pancreatic duct split prior to duct-to-mucosa pancreatico-jejunal anastomosis in pancreaticoduodenectomy
- Robotic Radical Nephrectomy with Vena Caval Tumor Thrombectomy: Experience of Novice Robotic Surgeons
- A case of pancreatic hamartoma pathologically confirmed after robot-assisted pancreaticoduodenectomy