Clin Endosc.
2024 Jul;57(4):476-485. 10.5946/ce.2023.198.
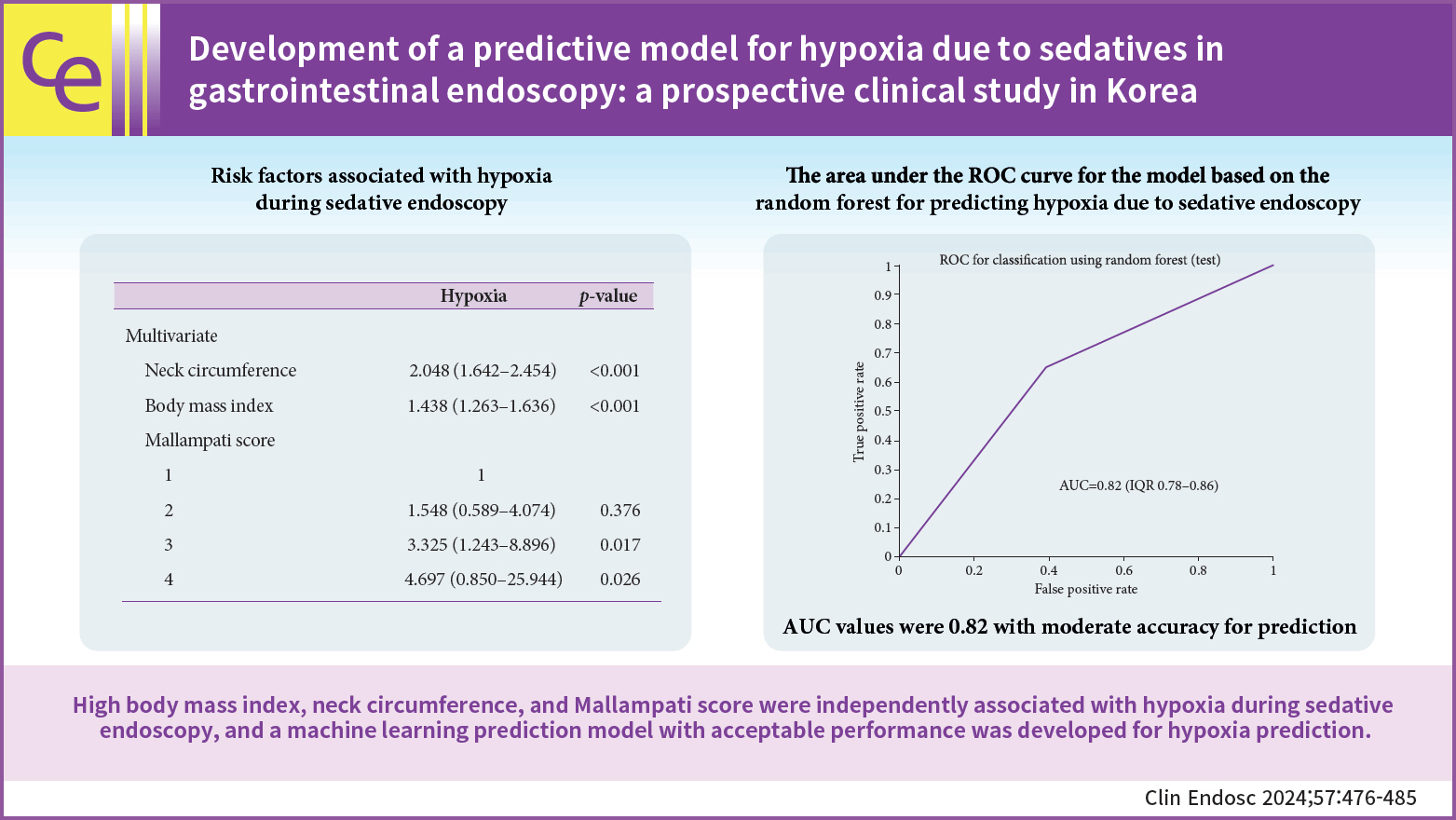
Development of a predictive model for hypoxia due to sedatives in gastrointestinal endoscopy: a prospective clinical study in Korea
- Affiliations
-
- 1Department of Internal Medicine, Korea University Ansan Hospital, Ansan, Korea
- 2Biomedical Research Center, Korea University Ansan Hospital, Ansan, Korea
- KMID: 2558104
- DOI: http://doi.org/10.5946/ce.2023.198
Abstract
- Background/Aims
Sedation has become a standard practice for patients undergoing gastrointestinal (GI) endoscopy. However, considering the serious cardiopulmonary adverse events associated with sedatives, it is important to identify patients at high risk. Machine learning can generate reasonable prediction for a wide range of medical conditions. This study aimed to evaluate the risk factors associated with sedation during GI endoscopy and develop a predictive model for hypoxia during endoscopy under sedation.
Methods
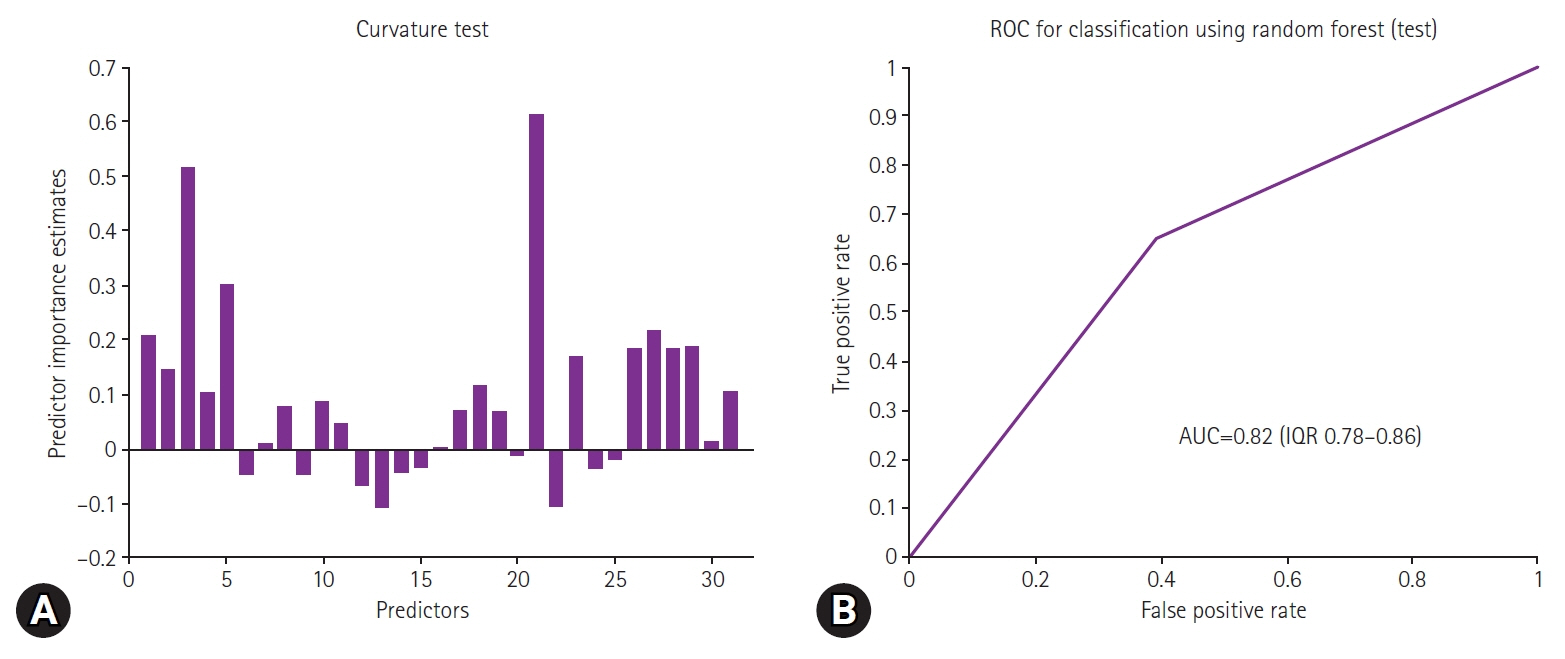
This prospective observational study enrolled 446 patients who underwent sedative endoscopy at the Korea University Ansan Hospital. Clinical data were used as predictor variables to construct predictive models using the random forest method that is a machine learning algorithm.
Results
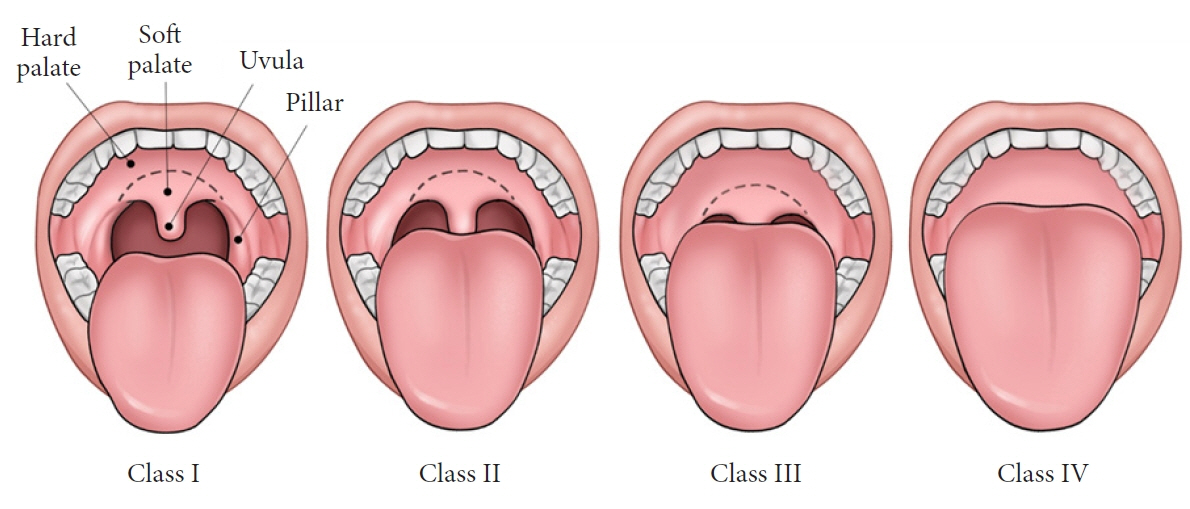
Seventy-two of the 446 patients (16.1%) experienced life-threatening hypoxia requiring immediate medical intervention. Patients who developed hypoxia had higher body weight, body mass index (BMI), neck circumference, and Mallampati scores. Propofol alone and higher initial and total dose of propofol were significantly associated with hypoxia during sedative endoscopy. Among these variables, high BMI, neck circumference, and Mallampati score were independent risk factors for hypoxia. The area under the receiver operating characteristic curve for the random forest-based predictive model for hypoxia during sedative endoscopy was 0.82 (95% confidence interval, 0.79–0.86) and displayed a moderate discriminatory power.
Conclusions
High BMI, neck circumference, and Mallampati score were independently associated with hypoxia during sedative endoscopy. We constructed a model with acceptable performance for predicting hypoxia during sedative endoscopy.
Keyword
Figure
Reference
-
1. Cohen LB, Delegge MH, Aisenberg J, et al. AGA Institute review of endoscopic sedation. Gastroenterology. 2007; 133:675–701.
Article2. McQuaid KR, Laine L. A systematic review and meta-analysis of randomized, controlled trials of moderate sedation for routine endoscopic procedures. Gastrointest Endosc. 2008; 67:910–923.
Article3. Lee JM, Park Y, Park JM. New sedatives and analgesic drugs for gastrointestinal endoscopic procedures. Clin Endosc. 2022; 55:581–587.
Article4. Moon SH. Sedation regimens for gastrointestinal endoscopy. Clin Endosc. 2014; 47:135–140.
Article5. Agostoni M, Fanti L, Gemma M, et al. Adverse events during monitored anesthesia care for GI endoscopy: an 8-year experience. Gastrointest Endosc. 2011; 74:266–275.
Article6. Triantafillidis JK, Merikas E, Nikolakis D, et al. Sedation in gastrointestinal endoscopy: current issues. World J Gastroenterol. 2013; 19:463–481.
Article7. Mallampati SR, Gatt SP, Gugino LD, et al. A clinical sign to predict difficult tracheal intubation: a prospective study. Can Anaesth Soc J. 1985; 32:429–434.
Article8. Park HJ, Kim BW, Lee JK, et al. 2021 Korean Society of Gastrointestinal Endoscopy clinical practice guidelines for endoscopic sedation. Clin Endosc. 2022; 55:167–182.
Article9. Rudner R, Jalowiecki P, Kawecki P, et al. Conscious analgesia/sedation with remifentanil and propofol versus total intravenous anesthesia with fentanyl, midazolam, and propofol for outpatient colonoscopy. Gastrointest Endosc. 2003; 57:657–663.
Article10. Strobl C, Boulesteix AL, Kneib T, et al. Conditional variable importance for random forests. BMC Bioinformatics. 2008; 9:307.
Article11. Nam JH, Jang DK, Lee JK, et al. Propofol alone versus propofol in combination with midazolam for sedative endoscopy in patients with paradoxical reactions to midazolam. Clin Endosc. 2022; 55:234–239.
Article12. Iber FL, Sutberry M, Gupta R, et al. Evaluation of complications during and after conscious sedation for endoscopy using pulse oximetry. Gastrointest Endosc. 1993; 39:620–625.
Article13. Woods SD, Chung SC, Leung JW, et al. Hypoxia and tachycardia during endoscopic retrograde cholangiopancreatography: detection by pulse oximetry. Gastrointest Endosc. 1989; 35:523–525.
Article14. Pozin IE, Zabida A, Nadler M, et al. Respiratory complications during recovery from gastrointestinal endoscopies performed by gastroenterologists under moderate sedation. Clin Endosc. 2023; 56:188–193.
Article15. Vargo JJ. Procedural sedation and obesity: waters left uncharted. Gastrointest Endosc. 2009; 70:980–984.
Article16. Wani S, Azar R, Hovis CE, et al. Obesity as a risk factor for sedation-related complications during propofol-mediated sedation for advanced endoscopic procedures. Gastrointest Endosc. 2011; 74:1238–1247.
Article17. Jehan S, Zizi F, Pandi-Perumal SR, et al. Obstructive sleep apnea and obesity: implications for public health. Sleep Med Disord. 2017; 1:93–99.18. Dumonceau JM, Riphaus A, Schreiber F, et al. Non-anesthesiologist administration of propofol for gastrointestinal endoscopy: European Society of Gastrointestinal Endoscopy, European Society of Gastroenterology and Endoscopy Nurses and Associates Guideline. Updated June 2015. Endoscopy. 2015; 47:1175–1189.
Article19. Ahbab S, Ataoğlu HE, Tuna M, et al. Neck circumference, metabolic syndrome and obstructive sleep apnea syndrome: evaluation of possible linkage. Med Sci Monit. 2013; 19:111–117.
Article20. Katz I, Stradling J, Slutsky AS, et al. Do patients with obstructive sleep apnea have thick necks? Am Rev Respir Dis. 1990; 141(5 Pt 1):1228–1231.
Article21. Xu CX, Chen X, Jia Y, et al. Stepwise sedation for elderly patients with mild/moderate COPD during upper gastrointestinal endoscopy. World J Gastroenterol. 2013; 19:4791–4798.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Sedation Regimens for Gastrointestinal Endoscopy
- The Elderly Also Deserves to Undergo Therapeutic Endoscopy Safely under Sedation with Propofol by Gastroenterologists
- Clinical Study on Duodenal Polyps Prevalence Submitted to Upper Gaatrointestinal Endoscopy
- New sedatives and analgesic drugs for gastrointestinal endoscopic procedures
- Arterial Oxygen Desaturation during Non-sedated Diagnostic Gastrointestinal Endoscopy