J Stroke.
2024 May;26(2):269-279. 10.5853/jos.2023.04259.
Endovascular Therapy in the Extended Time Window for Large Vessel Occlusion in Patients With Pre-Stroke Disability
- Affiliations
-
- 1Division of Stroke Care Unit, National Cerebral and Cardiovascular Center, Suita, Japan
- 2Stroke Center, Kindai University Hospital, Osakasayama, Japan
- 3Division of Stroke Prevention and Treatment, Institute of Medicine, University of Tsukuba, Tsukuba, Japan
- 4Department of Radiology, Radiation Oncology, Boston Medical Center, Boston, MA, USA
- 5Department of Neurosurgery, Hyogo Medical University, Nishinomiya, Japan
- 6Department of Neurology, University of Chicago, Chicago, IL, USA
- 7Department of Neurology, University of Pittsburgh Medical Center, Pittsburgh, PA, USA
- 8Department of Neurosurgery, Kobe City Medical General Hospital, Kobe, Japan
- 9Department of Neurology, Helsinki University Hospital, University of Helsinki, Helsinki, Finland
- 10Department of Neurology, Klinikum Ludwigshafen, Heidelberg University Hospital, Ludwigshafen, Germany
- 11Department of Neurology, Heidelberg University Hospital, Heidelberg, Germany
- 12Department of Neurology, Leuven University Hospital, Leuven, Belgium
- 13Department of Neurology, Faculty of Medicine and University Hospital Carl Gustav Carus, Technische Universität Dresden, Dresden, Germany
- 14Dresden Neurovascular Center, Faculty of Medicine and University Hospital Carl Gustav Carus, Technische Universität Dresden, Dresden, Germany
- 15Department of Neurology, Grady Memorial Hospital, Atlanta, GA, USA
- 16Department of Radiology, Boston Medical Center, Boston University Chobanian & Avedisian School of Medicine, Boston, MA, USA
- 17Department of Neurology, Hospital Vall d’Hebron, Barcelona, Spain
- 18Department of Neurology, Hospital de Egas Moniz, Centro Hospitalar Lisboa Ocidental, Lisbon, Portugal
- 19Department of Neurology, Hôpital Civil Marie Curie, Charleroi, Belgium
- 20Department of Neurology, Centre Hospitalier Universitaire de Lille, University of Lille, Lille, France
- 21Department of Neuroradiology, Hospital de Egas Moniz, Centro Hospitalar Lisboa Ocidental, Lisbon, Portugal
- 22Department of Neurology, University of Iowa, Iowa City, IA, USA
- 23Department of Neurology, UTHealth Houston, Houston, TX, USA
- 24Department of Clinical Neurosciences, University of Cambridge, Cambridge, UK
- 25Institute of Diagnostic and Interventional Neuroradiology, University Hospital Bern, University of Bern, Bern, Switzerland
- 26Department of Radiology, Helsinki University Hospital, University of Helsinki, Helsinki, Finland
- 27Department of Neurology, University of Toledo, Toledo, OH, USA
- 28Division of Interventional Neuroradiology, University of Massachusetts Memorial Medical Center, Worcester, MA, USA
- 29Department of Radiology, Centre Hospitalier de l’Universite de Montreal, Montreal, Canada
- 30Department of Neurology, State University of New York, Upstate Medical University, Syracuse, NY, USA
- 31Department of Radiology, Heidelberg University Hospital, Heidelberg, Germany
- 32Department of Diagnostic and Interventional Neuroradiology, Faculty of Medicine and University Hospital Carl Gustav Carus, Technische Universität Dresden, Dresden, Germany
- 33Department of Neurology, Lausanne University Hospital, Lausanne, Switzerland
- 34Department of Neuroradiology, Heidelberg University Hospital, Heidelberg, Germany
- 35Neuroscience and Stroke Program, Bon Secours Mercy Health St. Vincent Hospital, Toledo, OH, USA
- 36Department of Neurology, University Hospital Basel, Switzerland
- 37Department of Neurology, University Hospital Bern, Switzerland
- 38Department of Neurology, Boston Medical Center, Boston University Chobanian & Avedisian School of Medicine, Boston, MA, USA
- KMID: 2556047
- DOI: http://doi.org/10.5853/jos.2023.04259
Abstract
- Background and Purpose
We compared the outcomes of endovascular therapy (EVT) in an extended time window in patients with large-vessel occlusion (LVO) between patients with and without pre-stroke disability.
Methods
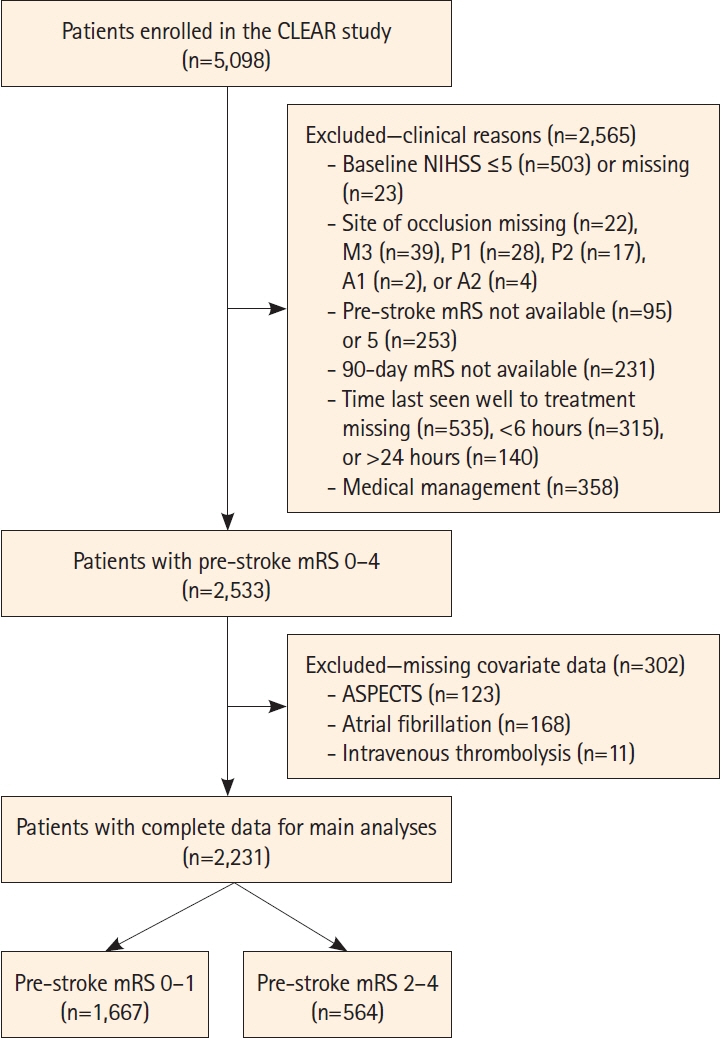
In this prespecified analysis of the multinational CT for Late Endovascular Reperfusion study (66 participating sites, 10 countries between 2014 and 2022), we analyzed data from patients with acute ischemic stroke with a pre-stroke modified Rankin Scale (mRS) score of 0–4 and LVO who underwent EVT 6–24 hours from the time last seen well. The primary outcome was the composite of functional independence (FI; mRS score 0–2) or return to the pre-stroke mRS score (return of Rankin, RoR) at 90 days. Outcomes were compared between patients with pre-stroke disability (pre-stroke mRS score 2–4) and those without (mRS score 0–1).
Results
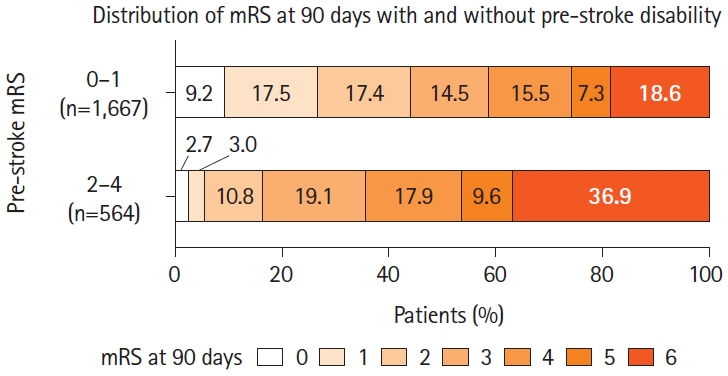
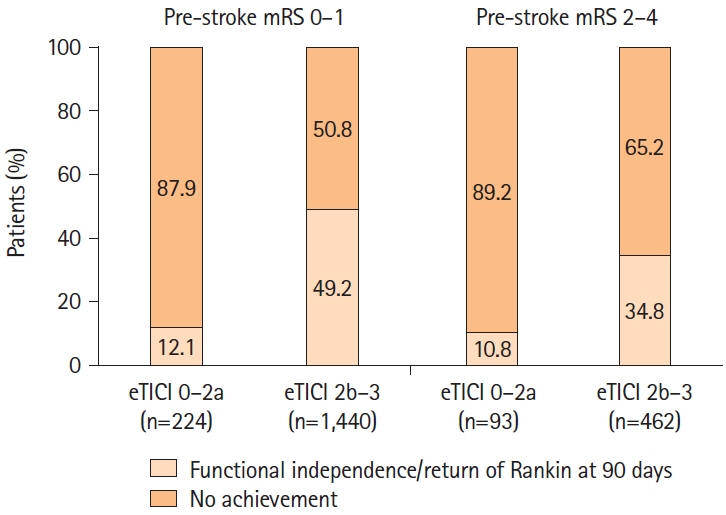
A total of 2,231 patients (median age, 72 years; median National Institutes of Health Stroke Scale score, 16) were included in the present analysis. Of these, 564 (25%) had pre-stroke disability. The primary outcome (FI or RoR) was observed in 30.7% of patients with pre-stroke disability (FI, 16.5%; RoR, 30.7%) compared to 44.1% of patients without (FI, 44.1%; RoR, 13.0%) (P<0.001). In multivariable logistic regression analysis with inverse probability of treatment weighting, pre-stroke disability was not associated with significantly lower odds of achieving FI or RoR (adjusted odds ratio 0.73, 95% confidence interval 0.43–1.25). Symptomatic intracranial hemorrhage occurred in 6.3% of both groups (P=0.995).
Conclusion
A considerable proportion of patients with late-presenting LVO and pre-stroke disability regained pre-stroke mRS scores after EVT. EVT may be appropriate for patients with pre-stroke disability presenting in the extended time window.
Figure
Reference
-
References
1. Yamagami H, Hayakawa M, Inoue M, Iihara K, Ogasawara K, Toyoda K, et al. Guidelines for mechanical thrombectomy in Japan, the fourth edition, March 2020: a guideline from the Japan Stroke Society, the Japan Neurosurgical Society, and the Japanese Society for Neuroendovascular Therapy. Neurol Med Chir (Tokyo). 2021; 61:163–192.
Article2. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019; 50:e344–e418.
Article3. Ganesh A, Luengo-Fernandez R, Pendlebury ST, Rothwell PM. Long-term consequences of worsened poststroke status in patients with premorbid disability. Stroke. 2018; 49:2430–2436.
Article4. Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after largevessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016; 387:1723–1731.
Article5. Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 2018; 378:11–21.6. Yoshimura S, Sakai N, Yamagami H, Uchida K, Beppu M, Toyoda K, et al. Endovascular therapy for acute stroke with a large ischemic region. N Engl J Med. 2022; 386:1303–1313.
Article7. Sarraj A, Hassan AE, Abraham MG, Ortega-Gutierrez S, Kasner SE, Hussain MS, et al. Trial of endovascular thrombectomy for large ischemic strokes. N Engl J Med. 2023; 388:1259–1271.
Article8. Huo X, Ma G, Tong X, Zhang X, Pan Y, Nguyen TN, et al. Trial of endovascular therapy for acute ischemic stroke with large infarct. N Engl J Med. 2023; 388:1272–1283.
Article9. Nguyen TN, Raymond J, Nogueira RG, Fischer U, Siegler JE. The problem of restrictive thrombectomy trial eligibility criteria. Stroke. 2022; 53:2988–2990.10. Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, OrtegaGutierrez S, et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. 2018; 378:708–718.11. Young MJ, Regenhardt RW, Leslie-Mazwi TM, Stein MA. Disabling stroke in persons already with a disability: ethical dimensions and directives. Neurology. 2020; 94:306–310.
Article12. Ganesh A, Fraser JF, Gordon Perue GL, Amin-Hanjani S, Leslie-Mazwi TM, Greenberg SM, et al. Endovascular treatment and thrombolysis for acute ischemic stroke in patients with premorbid disability or dementia: a scientific statement from the American Heart Association/American Stroke Association. Stroke. 2022; 53:e204–e217.
Article13. Goldhoorn RB, Verhagen M, Dippel DWJ, van der Lugt A, Lingsma HF, Roos YBWEM, et al. Safety and outcome of endovascular treatment in prestroke-dependent patients. Stroke. 2018; 49:2406–2414.
Article14. Slawski DE, Salahuddin H, Shawver J, Kenmuir CL, Tietjen GE, Korsnack A, et al. Mechanical thrombectomy in elderly stroke patients with mild-to-moderate baseline disability. Interv Neurol. 2018; 7:246–255.
Article15. Salwi S, Cutting S, Salgado AD, Espaillat K, Fusco MR, Froehler MT, et al. Mechanical thrombectomy in patients with ischemic stroke with prestroke disability. Stroke. 2020; 51:1539–1545.16. Larsson A, Karlsson C, Rentzos A, Schumacher M, Abrahamson M, Allardt A, et al. Do patients with large vessel occlusion ischemic stroke harboring prestroke disability benefit from thrombectomy? J Neurol. 2020; 267:2667–2674.17. de Havenon A, Castonguay A, Nogueira R, Nguyen TN, English J, Satti SR, et al. Prestroke disability and outcome after thrombectomy for emergent anterior circulation large vessel occlusion stroke. Neurology. 2021; 97:e1914–e1919.18. Seker F, Pfaff J, Schönenberger S, Herweh C, Nagel S, Ringleb PA, et al. Clinical outcome after thrombectomy in patients with stroke with premorbid modified Rankin scale scores of 3 and 4: a cohort study with 136 patients. AJNR Am J Neuroradiol. 2019; 40:283–286.19. Tanaka K, Yamagami H, Yoshimoto T, Uchida K, Morimoto T, Toyoda K, et al. Endovascular therapy for acute ischemic stroke in patients with prestroke disability. J Am Heart Assoc. 2021; 10:e020783.20. Siegler JE, Qureshi MM, Nogueira RG, Tanaka K, Nagel S, Michel P, et al. Endovascular vs medical management for late anterior large vessel occlusion with prestroke disability: analysis of CLEAR and RESCUE-Japan. Neurology. 2023; 100:e751–e763.21. Yoshimura S, Sakai N, Uchida K, Yamagami H, Ezura M, Okada Y, et al. Endovascular therapy in ischemic stroke with acute large-vessel occlusion: recovery by endovascular salvage for cerebral ultra-acute embolism Japan registry 2. J Am Heart Assoc. 2018; 7:e008796.22. Nguyen TN, Abdalkader M, Nagel S, Qureshi MM, Ribo M, Caparros F, et al. Noncontrast computed tomography vs computed tomography perfusion or magnetic resonance imaging selection in late presentation of stroke with large-vessel occlusion. JAMA Neurol. 2022; 79:22–31.
Article23. Seker F, Qureshi MM, Möhlenbruch MA, Nogueira RG, Abdalkader M, Ribo M, et al. Reperfusion without functional independence in late presentation of stroke with large vessel occlusion. Stroke. 2022; 53:3594–3604.
Article24. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007; 370:1453–1457.
Article25. Demeestere J, Qureshi MM, Vandewalle L, Wouters A, Strbian D, Nogueira RG, et al. Outcomes of bridging intravenous thrombolysis versus endovascular therapy alone in late-window acute ischemic stroke. Stroke. 2024 May 15 [Epub]. Available form: https://doi.org/10.1161/STROKEAHA.124.04649.26. Nguyen TN, Nogueira RG, Qureshi MM, Nagel S, Raymond J, Abdalkader M, et al. Noncontrast CT selected thrombectomy vs medical management for late-window anterior large vessel occlusion. Neurology. 2024; 102:e209324.
Article27. Mujanovic A, Strbian D, Demeestere J, Marto JP, Puetz V, Nogueira RG, et al. Safety and clinical outcomes of endovascular therapy versus medical management in late presentation of large ischemic stroke. Eur Stroke J. 2024 May 17 [Epub]. Available from https://doi.org/10.1177/23969873241249406.
Article28. Wilson JT, Hareendran A, Grant M, Baird T, Schulz UG, Muir KW, et al. Improving the assessment of outcomes in stroke: use of a structured interview to assign grades on the modified Rankin scale. Stroke. 2002; 33:2243–2246.29. Hacke W, Kaste M, Bluhmki E, Brozman M, Dávalos A, Guidetti D, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008; 359:1317–1329.
Article30. Chaisinanunkul N, Adeoye O, Lewis RJ, Grotta JC, Broderick J, Jovin TG, et al. Adopting a patient-centered approach to primary outcome analysis of acute stroke trials using a utility-weighted modified Rankin scale. Stroke. 2015; 46:2238–2243.31. McDonough RV, Ospel JM, Majoie CBLM, Saver JL, White P, Dippel DWJ, et al. Clinical outcome of patients with mild prestroke morbidity following endovascular treatment: a HERMES substudy. J Neurointerv Surg. 2023; 15:214–220.
Article32. Darsaut TE, Collins J, Raymond J. Patients may be right: clinical research should be designed in their best medical interest. Neurochirurgie. 2023; 69:101391.
Article33. Han TS, Fry CH, Gulli G, Affley B, Robin J, Irvin-Sellers M, et al. Prestroke disability predicts adverse poststroke outcome: a registry-based prospective cohort study of acute stroke. Stroke. 2020; 51:594–600.
Article34. Chen H, Khunte M, Colasurdo M, Jindal G, Malhotra A, Gandhi D, et al. Associations of osteoarthritis with thrombectomy utilization and outcomes for large vessel acute ischemic stroke. Stroke. 2023; 54:518–526.
Article35. Prakapenia A, Gruener C, Winzer S, Barlinn J, Gerber J, Pallesen LP, et al. Misjudgment of pre-stroke functional status contradicts beneficial outcomes after endovascular therapy for large vessel occlusion. J Neurol. 2019; 266:2060–2065.36. Fearon P, McArthur KS, Garrity K, Graham LJ, McGroarty G, Vincent S, et al. Prestroke modified Rankin stroke scale has moderate interobserver reliability and validity in an acute stroke setting. Stroke. 2012; 43:3184–3188.
Article37. Quinn TJ, Langhorne P, Stott DJ. Barthel index for stroke trials: development, properties, and application. Stroke. 2011; 42:1146–1151.38. Williams LS, Weinberger M, Harris LE, Clark DO, Biller J. Development of a stroke-specific quality of life scale. Stroke. 1999; 30:1362–1369.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- An Update of Recent Guideline for the Endovascular Recanalization Therapy in Acute Ischemic Stroke
- Emergency Microsurgical Embolectomy for the Treatment of Acute Intracranial Artery Occlusion: Report of Two Cases
- Review of Stroke Thrombolytics
- Reperfusion therapy in acute ischemic stroke
- Intravenous Thrombolysis and Endovascular Thrombectomy in Acute Ischemic Stroke with Minor Symptom