J Stroke.
2024 May;26(2):260-268. 10.5853/jos.2023.02621.
Infarcts Due to Large Vessel Occlusions Continue to Grow Despite Near-Complete Reperfusion After Endovascular Treatment
- Affiliations
-
- 1Department of Radiology, University of Calgary, Calgary, AB, Canada
- 2Department of Clinical Neurosciences, University of Calgary, Calgary, AB, Canada
- 3Department of Diagnostic Imaging, Brown University, Providence, RI, USA
- KMID: 2556046
- DOI: http://doi.org/10.5853/jos.2023.02621
Abstract
- Background and Purpose
Infarcts in acute ischemic stroke (AIS) patients may continue to grow even after reperfusion, due to mechanisms such as microvascular obstruction and reperfusion injury. We investigated whether and how much infarcts grow in AIS patients after near-complete (expanded Thrombolysis in Cerebral Infarction [eTICI] 2c/3) reperfusion following endovascular treatment (EVT), and to assess the association of post-reperfusion infarct growth with clinical outcomes.
Methods
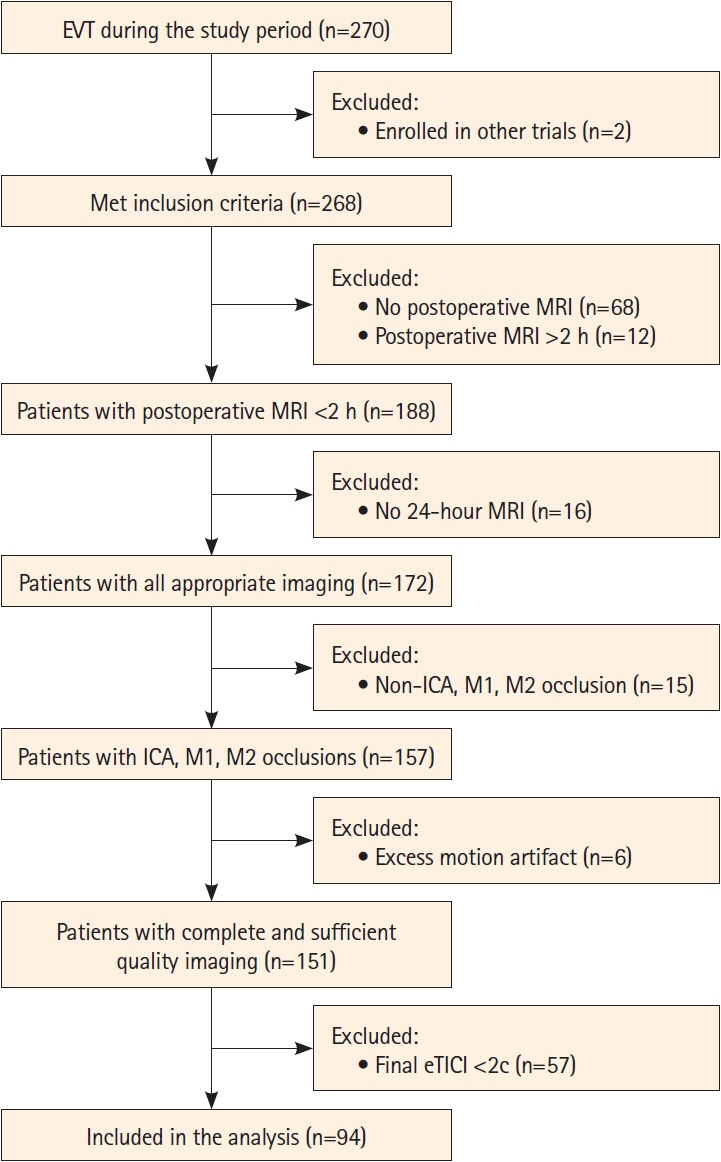
Data are from a single-center retrospective observational cohort study that included AIS patients undergoing EVT with near-complete reperfusion who received diffusion-weighted magnetic resonance imaging (MRI) within 2 hours post-EVT and 24 hours after EVT. Association of infarct growth between 2 and 24 hours post-EVT and 24-hour National Institutes of Health Stroke Scale (NIHSS) as well as 90-day modified Rankin Scale score was assessed using multivariable logistic regression.
Results
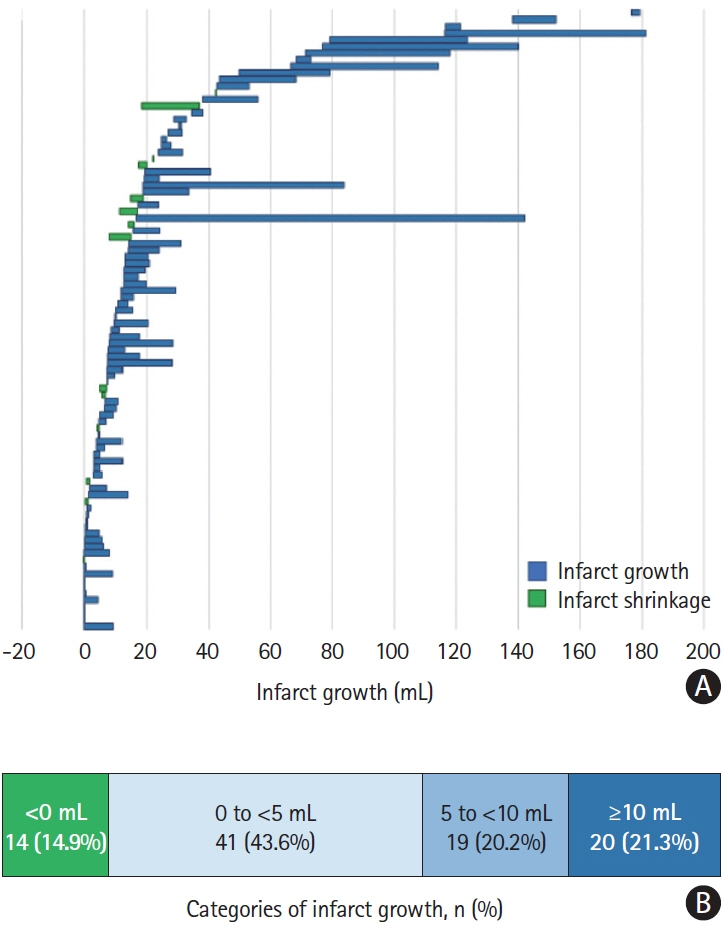
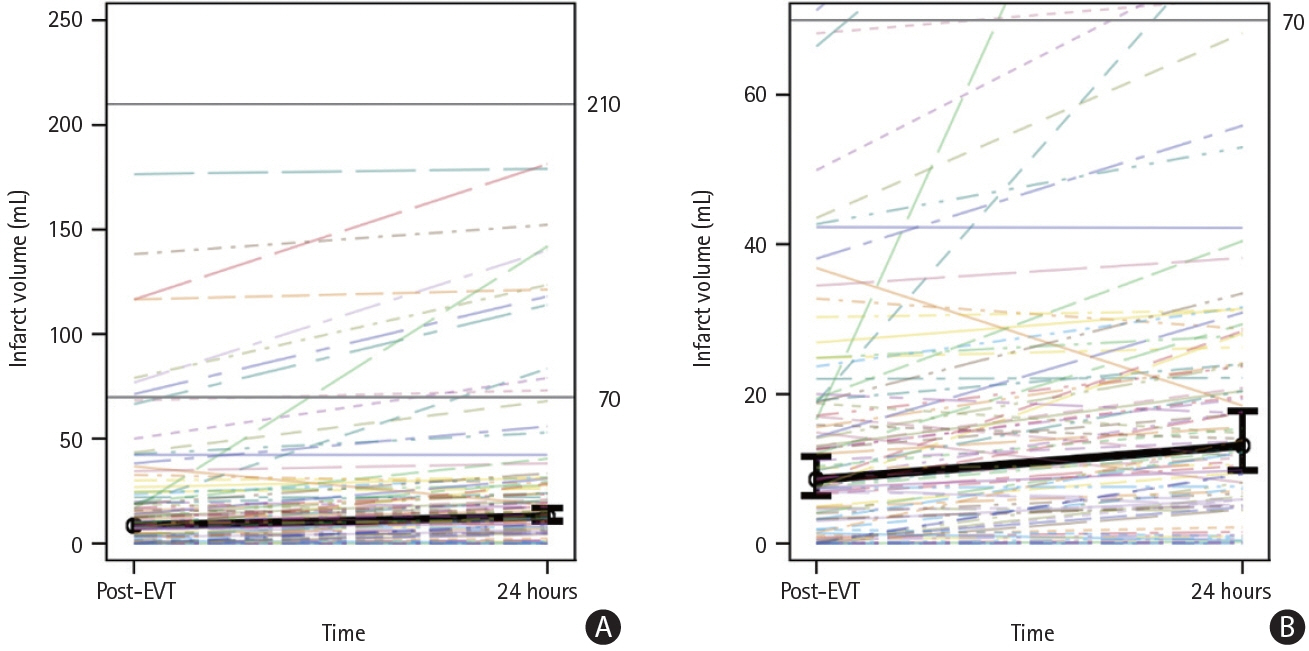
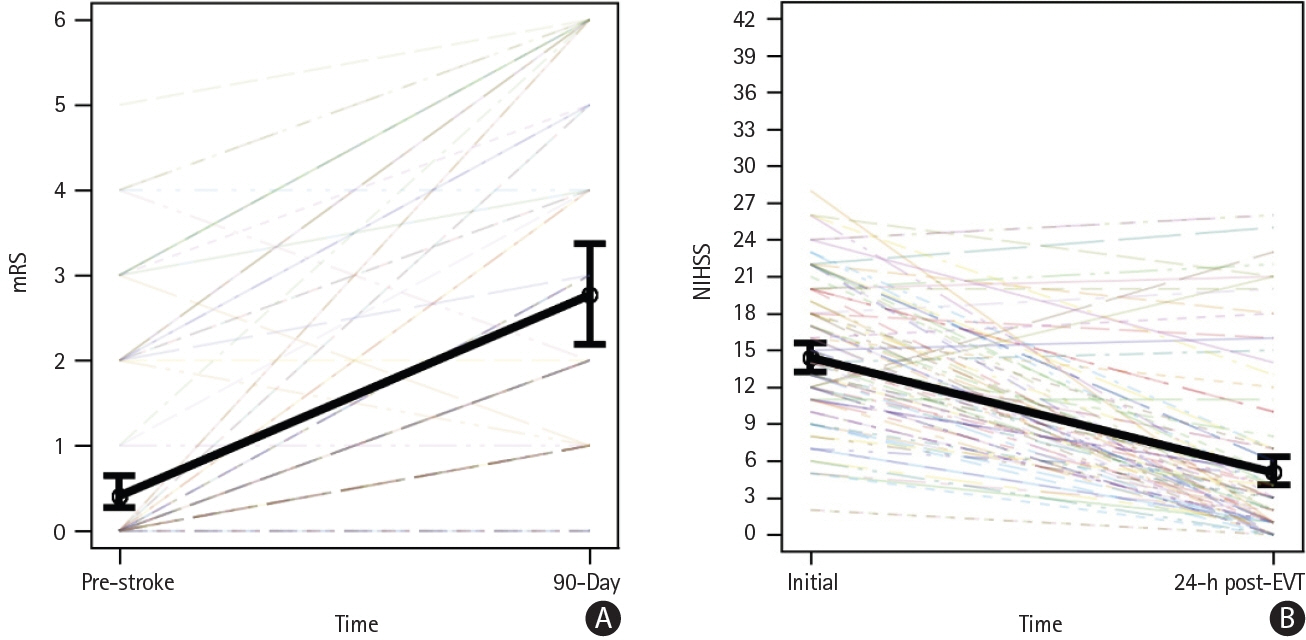
Ninety-four of 155 (60.6%) patients achieved eTICI 2c/3 and were included in the analysis. Eighty of these 94 (85.1%) patients showed infarct growth between 2 and 24 hours post-reperfusion. Infarct growth ≥5 mL was seen in 39/94 (41.5%) patients, and infarct growth ≥10 mL was seen in 20/94 (21.3%) patients. Median infarct growth between 2 and 24 hours post-reperfusion was 4.5 mL (interquartile range: 0.4–9.2 mL). Post-reperfusion infarct growth was associated with the 24-hour NIHSS in multivariable analysis (odds ratio: 1.16 [95% confidence interval 1.09–1.24], P<0.01).
Conclusion
Infarcts continue to grow after EVT, even if near-complete reperfusion is achieved. Investigating the underlying mechanisms may inform future therapeutic approaches for mitigating the process and help improve patient outcome.
Keyword
Figure
Reference
-
References
1. Ospel JM, Hill MD, Menon BK, Demchuk A, McTaggart R, Nogueira R, et al. Strength of association between infarct volume and clinical outcome depends on the magnitude of infarct size: results from the ESCAPE-NA1 trial. AJNR Am J Neuroradiol. 2021; 42:1375–1379.2. Ospel JM, Menon BK, Qiu W, Kashani N, Mayank A, Singh N, et al. A detailed analysis of infarct patterns and volumes at 24-hour noncontrast CT and diffusion-weighted MRI in acute ischemic stroke due to large vessel occlusion: results from the ESCAPE-NA1 trial. Radiology. 2021; 300:152–159.3. Ospel JM, Holodinsky JK, Goyal M. Management of acute ischemic stroke due to large-vessel occlusion: JACC focus seminar. J Am Coll Cardiol. 2020; 75:1832–1843.4. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018; 49:e46–e110.
Article5. Almekhlafi MA, Mishra S, Desai JA, Nambiar V, Volny O, Goel A, et al. Not all “successful” angiographic reperfusion patients are an equal validation of a modified TICI scoring system. Interv Neuroradiol. 2014; 20:21–27.
Article6. Gauberti M, Lapergue B, Martinez de Lizarrondo S, Vivien D, Richard S, Bracard S, et al. Ischemia-reperfusion injury after endovascular thrombectomy for ischemic stroke. Stroke. 2018; 49:3071–3074.7. Bala F, Ospel J, Mulpur B, Kim BJ, Yoo J, Menon BK, et al. Infarct growth despite successful endovascular reperfusion in acute ischemic stroke: a meta-analysis. AJNR Am J Neuroradiol. 2021; 42:1472–1478.8. Goyal M, McTaggart R, Ospel JM, van der Lugt A, Tymianski M, Wiest R, et al. How can imaging in acute ischemic stroke help us to understand tissue fate in the era of endovascular treatment and cerebroprotection? Neuroradiology. 2022; 64:1697–1707.
Article9. Sah RG, d’Esterre CD, Hill MD, Hafeez M, Tariq S, Forkert ND, et al. Diffusion-weighted imaging lesion growth occurs despite recanalization in acute ischemic stroke: implications for future treatment trials. Int J Stroke. 2019; 14:257–264.
Article10. Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O'Neal L, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019; 95:103208.
Article11. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009; 42:377–381.
Article12. Hill MD, Goyal M, Menon BK, Nogueira RG, McTaggart RA, Demchuk AM, et al. Efficacy and safety of nerinetide for the treatment of acute ischaemic stroke (ESCAPE-NA1): a multicentre, double-blind, randomised controlled trial. Lancet. 2020; 395:878–887.13. Liebeskind DS, Bracard S, Guillemin F, Jahan R, Jovin TG, Majoie CB, et al. eTICI reperfusion: defining success in endovascular stroke therapy. J Neurointerv Surg. 2019; 11:433–438.14. Ospel JM, Qiu W, Menon BK, Mayank A, Demchuk A, McTaggart R, et al. Radiologic patterns of intracranial hemorrhage and clinical outcome after endovascular treatment in acute ischemic stroke: results from the ESCAPE-NA1 trial. Radiology. 2021; 300:402–409.
Article15. von Kummer R, Broderick JP, Campbell BC, Demchuk A, Goyal M, Hill MD, et al. The Heidelberg bleeding classification: classification of bleeding events after ischemic stroke and reperfusion therapy. Stroke. 2015; 46:2981–2986.16. Gross GJ, Auchampach JA. Reperfusion injury: does it exist? J Mol Cell Cardiol. 2007; 42:12–18.
Article17. Ospel J, Rex N, Kandregula S, Goyal M. The vessel has been recanalized: now what? Neurotherapeutics. 2023; 20:679–692.
Article18. Goyal M, Ospel JM, Menon B, Almekhlafi M, Jayaraman M, Fiehler J, et al. Challenging the ischemic core concept in acute ischemic stroke imaging. Stroke. 2020; 51:3147–3155.19. Sarraj A, Hassan AE, Grotta J, Blackburn S, Day A, Abraham M, et al. Early infarct growth rate correlation with endovascular thrombectomy clinical outcomes: analysis from the SELECT study. Stroke. 2021; 52:57–69.
Article20. Rex N, Oueidat K, Ospel J, McDonough R, Rinkel L, Baird GL, et al. Modeling diffusion-weighted imaging lesion expansion between 2 and 24 h after endovascular thrombectomy in acute ischemic stroke. Neuroradiology. 2024; 66:621–629.
Article21. Banks JL, Marotta CA. Outcomes validity and reliability of the modified Rankin scale: implications for stroke clinical trials: a literature review and synthesis. Stroke. 2007; 38:1091–1096.
Article22. d’Esterre CD, Sah RG, Assis Z, Talai AS, Demchuk AM, Hill MD, et al. Defining reperfusion post endovascular therapy in ischemic stroke using MR-dynamic contrast enhanced perfusion. Br J Radiol. 2020; 93:20190890.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Frontline Contact Aspiration Treatment for Emergent Large Vessel Occlusion: A Review Focused on Practical Techniques
- Endovascular Treatment of Large Vessel Occlusion Strokes Due to Intracranial Atherosclerotic Disease
- First-Line Aspiration Thrombectomy of M2 Occlusions with a Novel Reperfusion Catheter (REDTM 62): Real-World Experience from Two Tertiary Comprehensive Stroke Centers
- Unfavorable Vascular Anatomy during Endovascular Treatment of Stroke: Challenges and Bailout Strategies
- Hemodynamics of Leptomeningeal Collaterals after Large Vessel Occlusion and Blood Pressure Management with Endovascular Treatment