Neurointervention.
2024 Nov;19(3):139-147. 10.5469/neuroint.2024.00171.
First-Line Aspiration Thrombectomy of M2 Occlusions with a Novel Reperfusion Catheter (REDTM 62): Real-World Experience from Two Tertiary Comprehensive Stroke Centers
- Affiliations
-
- 1Department of Radiology and Neuroradiology, Sana Kliniken Duisburg, Duisburg, Germany
- 2Department of Diagnostic and Interventional Neuroradiology, Medical School Hannover, Hannover, Germany
- 3Department of Radiology and Neuroradiology, Klinikum Vest, Recklinghausen, Germany
- KMID: 2560217
- DOI: http://doi.org/10.5469/neuroint.2024.00171
Abstract
- Purpose
The direct aspiration first pass technique (ADAPT) is an effective and safe endovascular treatment for distal medium vessel occlusions (DMVOs). We evaluated technical features and initial results of a novel reperfusion catheter (REDTM 62) used for frontline aspiration thrombectomy of M2 occlusions in acute ischemic stroke patients. Appropriate aspiration catheters are crucial for a successful ADAPT maneuver; however, the selection of catheters suitable for smaller-sized vessels is scarce compared to the ones for large vessel occlusions.
Materials and Methods
All patients treated with ADAPT using REDTM 62 as the frontline treatment approach for acute M2 occlusions between December 2022 and February 2024 were retrospectively enrolled. Demographic data, procedural timings and safety, recanalization rates, and outcome data were recorded.
Results
Twenty patients with a median admission National Institutes of Health Stroke Scale (NIHSS) score of 8 were identified. Successful revascularization (DMVO-thrombolysis in cerebral infarction [TICI]≥2b) with REDTM 62 aspiration thrombectomy was obtained in 65.0% (13/20) of cases. The first pass effect was 45.0% (9/20). In 2 cases, the REDTM 62 did not reach the clot due to marked distal vessel tortuosity. Stent retrievers were additionally used in 9 cases and led to an overall DMVO-TICI 2c/3 of 90.0% (18/20). Mean procedural time was 48 minutes. No complications directly related to ADAPT occurred. In-hospital mortality rate was 20.0% (4/20). The median discharge NIHSS score was 2.5. A good functional outcome at discharge (modified Rankin scale 0-2) was achieved in 55.0% (11/20) of cases.
Conclusion
Our initial experiences with the novel REDTM 62 reperfusion catheter for treatment of M2 occlusions is in line with published data. ADAPT using this catheter may be considered as a safe and effective first-line treatment option. Further studies are warranted to validate the initial results.
Keyword
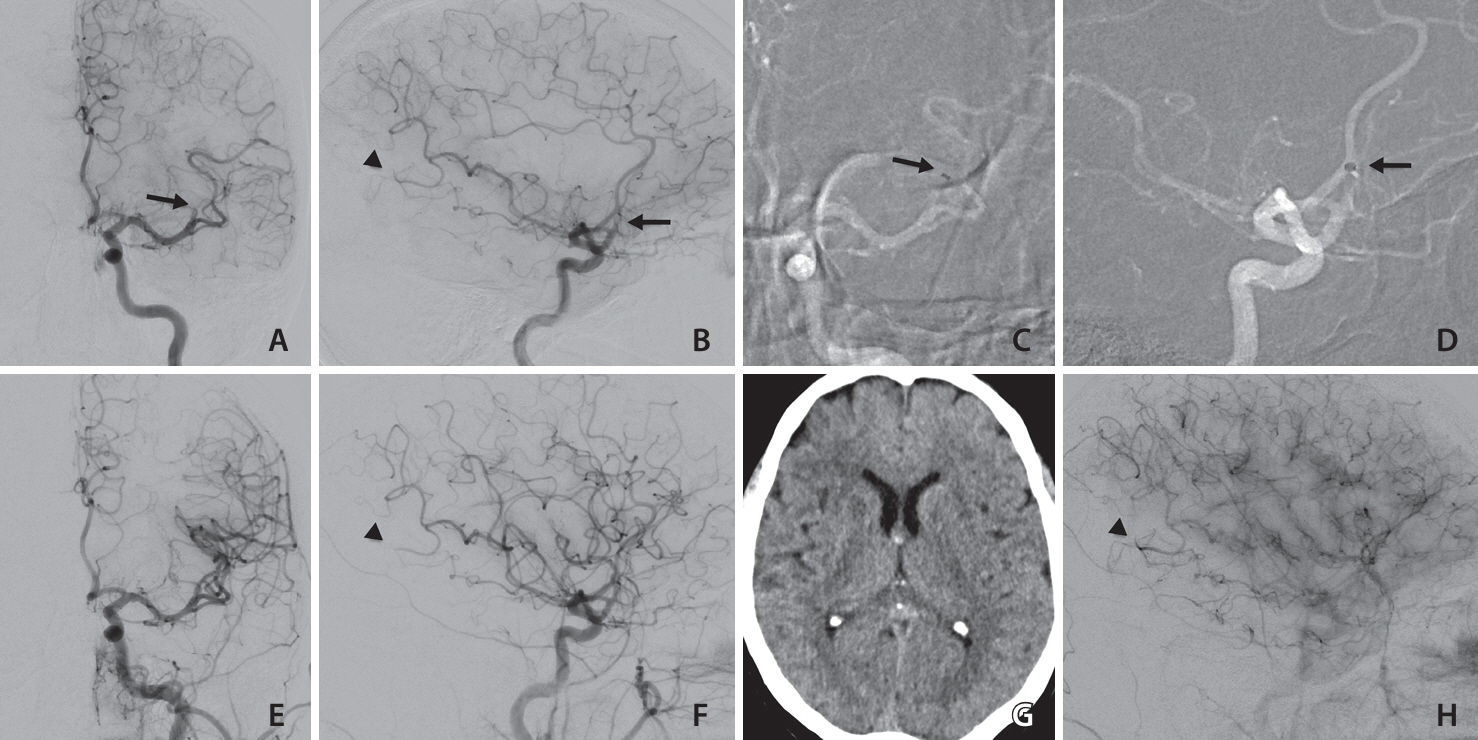
Figure
Reference
-
1. Saver JL, Chapot R, Agid R, Hassan A, Jadhav AP, Liebeskind DS, Distal Thrombectomy Summit Group, et al. Thrombectomy for distal, medium vessel occlusions: a consensus statement on present knowledge and promising directions. Stroke. 2020; 51:2872–2884.2. Sarraj A, Sangha N, Hussain MS, Wisco D, Vora N, Elijovich L, et al. Endovascular therapy for acute ischemic stroke with occlusion of the middle cerebral artery M2 segment. JAMA Neurol. 2016; 73:1291–1296.3. Román LS, Menon BK, Blasco J, Hernández-Pérez M, Dávalos A, Majoie CBLM, HERMES Collaborators, et al. Imaging features and safety and efficacy of endovascular stroke treatment: a meta-analysis of individual patient-level data. Lancet Neurol. 2018; 17:895–904.4. Almekhlafi M, Ospel JM, Saposnik G, Kashani N, Demchuk A, Hill MD, et al. Endovascular treatment decisions in patients with M2 segment MCA occlusions. AJNR Am J Neuroradiol. 2020; 41:280–285.5. Grossberg JA, Rebello LC, Haussen DC, Bouslama M, Bowen M, Barreira CM, et al. Beyond large vessel occlusion strokes: distal occlusion thrombectomy. Stroke. 2018; 49:1662–1668.6. Gory B, Lapergue B, Blanc R, Labreuche J, Ben Machaa M, Duhamel A, ASTER Trial Investigators, et al. Contact aspiration versus stent retriever in patients with acute ischemic stroke with M2 occlusion in the ASTER randomized trial (contact aspiration versus stent retriever for successful revascularization). Stroke. 2018; 49:461–464.7. Lapergue B, Blanc R, Gory B, Labreuche J, Duhamel A, Marnat G, ASTER Trial Investigators, et al. Effect of endovascular contact aspiration vs stent retriever on revascularization in patients with acute ischemic stroke and large vessel occlusion: the ASTER randomized clinical trial. JAMA. 2017; 318:443–452.8. Romano DG, Frauenfelder G, Caragliano A, Semeraro V, Pitrone A, Bozzi A, et al. Multicentric experience with an intermediate aspiration catheter for distal M2 ischemic stroke. J Stroke Cerebrovasc Dis. 2020; 29:105389.9. Saber H, Narayanan S, Palla M, Saver JL, Nogueira RG, Yoo AJ, et al. Mechanical thrombectomy for acute ischemic stroke with occlusion of the M2 segment of the middle cerebral artery: a meta-analysis. J Neurointerv Surg. 2018; 10:620–624.10. Kim YW, Son S, Kang DH, Hwang YH, Kim YS. Endovascular thrombectomy for M2 occlusions: comparison between forced arterial suction thrombectomy and stent retriever thrombectomy. J Neurointerv Surg. 2017; 9:626–630.11. Nikoubashman O, Nikoubashman A, Büsen M, Wiesmann M. Necessary catheter diameters for mechanical thrombectomy with ADAPT. AJNR Am J Neuroradiol. 2017; 38:2277–2281.12. Osborn AG. Diagnostic cerebral angiography. Lippincott Williams & Wilkins;1999.13. Romano DG, Frauenfelder G, Napoletano R, Botto A, Locatelli G, Panza MP, et al. ADAPT with new Catalyst 5 reperfusion catheter for distal M2 ischemic stroke: preliminary experience. World Neurosurg. 2020; 135:e650–e656.14. Ospel JM, Goyal M. A review of endovascular treatment for medium vessel occlusion stroke. J Neurointerv Surg. 2021; 13:623–630.15. Grieb D, Greling B, Schulz K, Boxberg F, Melber K, Abu-Fares O, et al. Endovascular treatment of distal medium vessel occlusions using microcatheter aspiration thrombectomy. Interv Neuroradiol. 2024; 30:234–241.16. von Kummer R, Broderick JP, Campbell BC, Demchuk A, Goyal M, Hill MD, et al. The Heidelberg bleeding classification: classification of bleeding events after ischemic stroke and reperfusion therapy. Stroke. 2015; 46:2981–2986.17. Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in acute stroke treatment. Stroke. 1993; 24:35–41.18. Kunz WG, Almekhlafi MA, Goyal M. Distal vessel occlusions: when to consider endovascular thrombectomy. Stroke. 2018; 49:1581–1583.19. Goyal M, Ospel JM, Menon BK, Hill MD. MeVO: the next frontier? J Neurointerv Surg. 2020; 12:545–547.20. Turk AS, Frei D, Fiorella D, Mocco J, Baxter B, Siddiqui A, et al. ADAPT FAST study: a direct aspiration first pass technique for acute stroke thrombectomy. J Neurointerv Surg. 2018; 10:i4–i7.21. Grieb D, Meila D, Sommer CM, Schulz K, Abu-Fares O, Donnerstag F, et al. Feasibility and safety of ADAPT in acute distal posterior cerebral artery occlusions. Eur J Radiol. 2023; 165:110936.22. Vargas J, Spiotta AM, Fargen K, Turner RD, Chaudry I, Turk A. Experience with A direct aspiration first pass technique (ADAPT) for thrombectomy in distal cerebral artery occlusions causing acute ischemic stroke. World Neurosurg. 2017; 99:31–36.23. Premat K, Bartolini B, Baronnet-Chauvet F, Shotar E, Degos V, Muresan P, et al. Single-center experience using the 3MAX reperfusion catheter for the treatment of acute ischemic stroke with distal arterial occlusions. Clin Neuroradiol. 2018; 28:553–562.24. Altenbernd J, Kuhnt O, Hennigs S, Hilker R, Loehr C. Frontline ADAPT therapy to treat patients with symptomatic M2 and M3 occlusions in acute ischemic stroke: initial experience with the Penumbra ACE and 3MAX reperfusion system. J Neurointerv Surg. 2018; 10:434–439.25. Navia P, Larrea JA, Pardo E, Arce A, Martínez-Zabaleta M, Díez-González N, et al. Initial experience using the 3MAX cerebral reperfusion catheter in the endovascular treatment of acute ischemic stroke of distal arteries. J Neurointerv Surg. 2016; 8:787–790.26. Grieb D, Schlunz-Hendann M, Brinjikji W, Melber K, Greling B, Lanfermann H, et al. Mechanical thrombectomy of M2 occlusions with distal access catheters using ADAPT. J Neuroradiol. 2019; 46:231–237.27. Turk AS 3rd, Siddiqui A, Fifi JT, De Leacy RA, Fiorella DJ, Gu E, et al. Aspiration thrombectomy versus stent retriever thrombectomy as first-line approach for large vessel occlusion (COMPASS): a multicentre, randomised, open label, blinded outcome, non-inferiority trial. Lancet. 2019; 393:998–1008.28. Penumbra [Internet]. Penumbra;[cited 2023 Oct 31]. Available from: https://www.penumbrainc.com/eu/products/red-reperfusion-catheters/.29. Park JS, Kwak HS. Manual aspiration thrombectomy using penumbra catheter in patients with acute M2 occlusion: a single-center analysis. J Korean Neurosurg Soc. 2016; 59:352–356.30. Meyer L, Stracke P, Wallocha M, Broocks G, Sporns P, Piechowiak EI, et al. Aspiration versus stent retriever thrombectomy for distal, medium vessel occlusion stroke in the posterior circulation: a subanalysis of the TOPMOST study. Stroke. 2022; 53:2449–2457.31. Ng PP, Larson TC, Nichols CW, Murray MM, Salzman KL, Smith RH. Intraprocedural predictors of post-stent retriever thrombectomy subarachnoid hemorrhage in middle cerebral artery stroke. J Neurointerv Surg. 2019; 11:127–132.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Forced Arterial Suction Thrombectomy Using Distal Access Catheter in Acute Ischemic Stroke
- Manual Aspiration Thrombectomy Using Penumbra Catheter in Patients with Acute M2 Occlusion : A Single-Center Analysis
- Initial Experience Using the 5MAX(TM) ACE Reperfusion Catheter in Intra-arterial Therapy for Acute Ischemic Stroke
- Aspiration-Retriever Technique for Stroke with Large Bore Intermediate Catheter : A Single Center Experience
- The Limitations of Thrombectomy with Solitaire(TM) AB as First-line Treatment in Acute Ischemic Stroke: A Single Center Experience