J Korean Neurosurg Soc.
2016 Jul;59(4):352-356. 10.3340/jkns.2016.59.4.352.
Manual Aspiration Thrombectomy Using Penumbra Catheter in Patients with Acute M2 Occlusion : A Single-Center Analysis
- Affiliations
-
- 1Department of Neurosurgery, and Research Institute of Clinical Medicine of Chonbuk National University, Jeonju, Korea.
- 2Biomedical Research Institute of Chonbuk National University Hospital, Jeonju, Korea. kwak8140@jbnu.ac.kr
- 3Department of Radiology, and Research Institute of Clinical Medicine of Chonbuk National University, Jeonju, Korea.
- KMID: 2315969
- DOI: http://doi.org/10.3340/jkns.2016.59.4.352
Abstract
OBJECTIVE
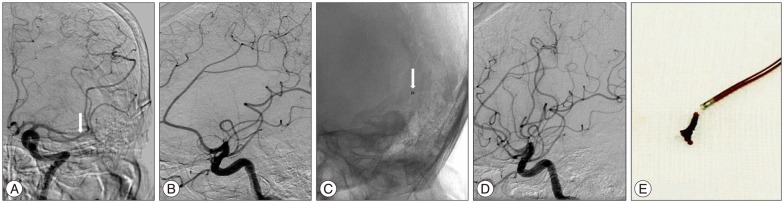
The efficacy and safety of manual aspiration thrombectomy using Penumbra in an acute occlusion of large intracranial arteries has been proven in many previous studies. Our study aimed to retrospectively assess the efficacy and safety of manual aspiration thrombectomy using Penumbra in patients with small vessel occlusions (M2 segment of the MCA).
METHODS
We conducted a retrospective review of 32 patients who underwent manual aspiration thrombectomy using the Penumbra 4 MAX Reperfusion Catheter for treatment of an M2 occlusion between January 2013 and November 2014. We evaluated immediate angiographic results and clinical outcomes through review of patient electronic medical records.
RESULTS
There were slightly more men in this study (M : F=18 : 14) and the median age was 72.5 (age range : 41-90). The rate of successful recanalization (TICI grade ≥2b) was 84% (27/32). NIHSS at discharge and favorable clinical outcomes at 3 months were significantly improved than baseline. Median initial NIHSS score was 10 (range : 4-25) and was 4 (range : 0-14) at discharge. Favorable clinical outcomes (mRS score ≤2 at 3 months) were seen in 25 out of 32 patients (78%). There were no procedure-related symptomatic intracerebral hemorrhages. One patient expired after discharge due to a cardiac problem.
CONCLUSION
Manual aspiration thrombectomy might be safe and is capable of achieving a high rate of successful recanalization and favorable clinical outcomes in patients with distal cerebral vessel occlusion (M2).
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Contact Aspiration versus Stent-Retriever Thrombectomy for Distal Middle Cerebral Artery Occlusions in Acute Ischemic Stroke: Meta-Analysis
Kevin Phan, Julian Maingard, Hong Kuan Kok, Adam A Dmytriw, Sourabh Goyal, Ronil Chandra, Duncan Mark Brooks, Vincent Thijs, Hamed Asadi
Neurointervention. 2018;13(2):100-109. doi: 10.5469/neuroint.2018.00997.Meta-Analysis of Endovascular Treatment for Acute M2 Occlusion
Chul Ho Kim, Sung-Eun Kim, Jin Pyeong Jeon
J Korean Neurosurg Soc. 2019;62(2):193-200. doi: 10.3340/jkns.2017.0299.
Reference
-
1. Broderick JP, Palesch YY, Demchuk AM, Yeatts SD, Khatri P, Hill MD, et al. Endovascular therapy after intravenous t-PA versus t-PA alone for stroke. N Engl J Med. 2013; 368:893–903. PMID: 23390923.
Article2. Flores A, Tomasello A, Cardona P, de Miquel MA, Gomis M, Garcia Bermejo P, et al. Endovascular treatment for M2 occlusions in the era of stentrievers : a descriptive multicenter experience. J Neurointerv Surg. 2015; 7:234–237. PMID: 24578483.
Article3. Hacke W, Kaste M, Bluhmki E, Brozman M, Dávalos A, Guidetti D, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008; 359:1317–1329. PMID: 18815396.
Article4. IMS II Trial Investigators. The Interventional Management of Stroke (IMS) II Study. Stroke. 2007; 38:2127–2135. PMID: 17525387.5. Jankowitz B, Aghaebrahim A, Zirra A, Spataru O, Zaidi S, Jumaa M, et al. Manual aspiration thrombectomy : adjunctive endovascular recanalization technique in acute stroke interventions. Stroke. 2012; 43:1408–1411. PMID: 22382156.6. Kang DH, Hwang YH, Kim YS, Park J, Kwon O, Jung C. Direct thrombus retrieval using the reperfusion catheter of the penumbra system : forced-suction thrombectomy in acute ischemic stroke. AJNR Am J Neuroradiol. 2011; 32:283–287. PMID: 21087940.
Article7. Nogueira RG, Lutsep HL, Gupta R, Jovin TG, Albers GW, Walker GA, et al. Trevo versus Merci retrievers for thrombectomy revascularisation of large vessel occlusions in acute ischaemic stroke (TREVO 2) : a randomised trial. Lancet. 2012; 380:1231–1240. PMID: 22932714.
Article8. Pereira VM, Gralla J, Davalos A, Bonafé A, Castaño C, Chapot R, et al. Prospective, multicenter, single-arm study of mechanical thrombectomy using Solitaire Flow Restoration in acute ischemic stroke. Stroke. 2013; 44:2802–2807. PMID: 23908066.
Article9. Rahme R, Abruzzo TA, Martin RH, Tomsick TA, Ringer AJ, Furlan AJ, et al. Is intra-arterial thrombolysis beneficial for M2 occlusions? Subgroup analysis of the PROACT-II trial. Stroke. 2013; 44:240–242. PMID: 23223507.
Article10. Rahme R, Yeatts SD, Abruzzo TA, Jimenez L, Fan L, Tomsick TA, et al. Early reperfusion and clinical outcomes in patients with M2 occlusion : pooled analysis of the PROACT II, IMS, and IMS II studies. J Neurosurg. 2014; 121:1354–1358. PMID: 25259569.
Article11. Rha JH, Saver JL. The impact of recanalization on ischemic stroke outcome : a meta-analysis. Stroke. 2007; 38:967–973. PMID: 17272772.
Article12. Saver JL, Jahan R, Levy EI, Jovin TG, Baxter B, Nogueira RG, et al. Solitaire flow restoration device versus the Merci Retriever in patients with acute ischaemic stroke (SWIFT) : a randomised, parallel-group, non-inferiority trial. Lancet. 2012; 380:1241–1249. PMID: 22932715.
Article13. Sheth SA, Yoo B, Saver JL, Starkman S, Ali LK, Kim D, et al. M2 occlusions as targets for endovascular therapy : comprehensive analysis of diffusion/perfusion MRI, angiography, and clinical outcomes. J Neurointerv Surg. 2015; 7:478–483. PMID: 24821842.
Article14. Shi ZS, Loh Y, Walker G, Duckwiler GR. MERCI and Multi-MERCI Investigators. Clinical outcomes in middle cerebral artery trunk occlusions versus secondary division occlusions after mechanical thrombectomy : pooled analysis of the Mechanical Embolus Removal in Cerebral Ischemia (MERCI) and Multi MERCI trials. Stroke. 2010; 41:953–960. PMID: 20378867.
Article15. Tomsick T, Broderick J, Carrozella J, Khatri P, Hill M, Palesch Y, et al. Revascularization results in the Interventional Management of Stroke II trial. AJNR Am J Neuroradiol. 2008; 29:582–587. PMID: 18337393.
Article16. Turk AS, Spiotta A, Frei D, Mocco J, Baxter B, Fiorella D, et al. Initial clinical experience with the ADAPT technique : a direct aspiration first pass technique for stroke thrombectomy. J Neurointerv Surg. 2014; 6:231–237. PMID: 23624315.
Article17. Wolpert SM, Bruckmann H, Greenlee R, Wechsler L, Pessin MS, del Zoppo GJ. Neuroradiologic evaluation of patients with acute stroke treated with recombinant tissue plasminogen activator. The rt-PA Acute Stroke Study Group. AJNR Am J Neuroradiol. 1993; 14:3–13. PMID: 8427107.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Forced Arterial Suction Thrombectomy Using Distal Access Catheter in Acute Ischemic Stroke
- Mechanical thrombectomy for acute ischemic stroke with occlusion of the M2 segment of the middle cerebral artery: A literature review
- Pseudoaneurysm Formation after Repetitive Suction Thrombectomy Using a Penumbra Suction Catheter
- Directly Retrieved Entire Clot from Forced Suction Thrombectomy Using the Penumbra System in Acute Middle Cerebral Artery Occlusion
- Endovascular Approach in Patients with Acute Complete Occlusion Due to Middle Cerebral Artery Dissection