J Cerebrovasc Endovasc Neurosurg.
2016 Sep;18(3):296-301. 10.7461/jcen.2016.18.3.296.
Pseudoaneurysm Formation after Repetitive Suction Thrombectomy Using a Penumbra Suction Catheter
- Affiliations
-
- 1Department of Neurosurgery, School of Medicine, Regional Cerebrovascular Center, Research Institute for Brain Sciences, Chungnam National University & Hospital, Daejeon, Korea. solesoul@daum.net
- KMID: 2355658
- DOI: http://doi.org/10.7461/jcen.2016.18.3.296
Abstract
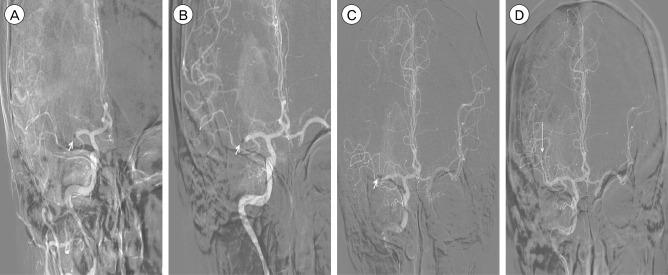
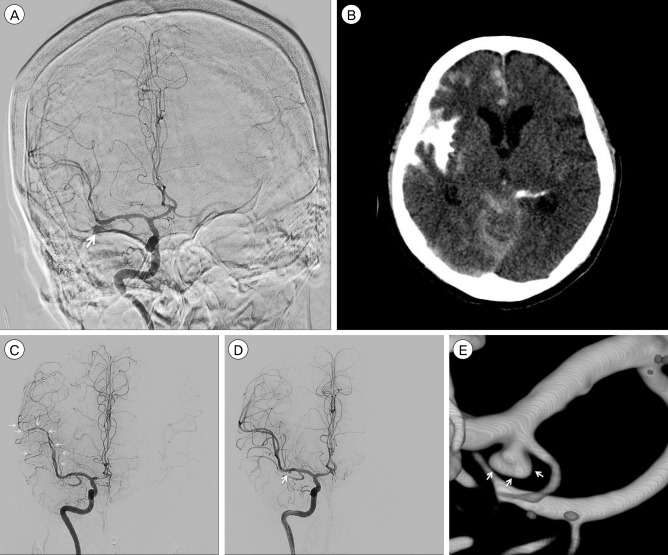
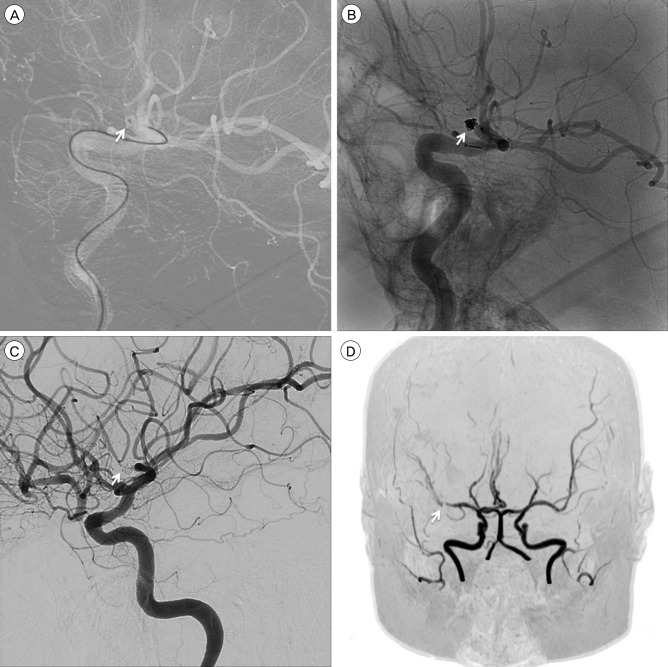
- With the recent advent of suction catheters, the use of manual aspiration thrombectomy (MAT) for patients with acute ischemic stroke with large vessel occlusion has increased. Although contrast leakage and subarachnoid hemorrhage have been reported during MAT procedures, pseudoaneurysm formation due to vessel injury by suction catheters has not been. We discuss the case of a 60-year-old woman who presented to our emergency room with dysarthria and left-sided weakness. She underwent suction thrombectomy 5 times for acute middle cerebral artery occlusion and significant contrast leakage occurred during the procedure. On follow-up angiogram on post-operative day 15, we noticed a pseudoaneurysm, which was treated with detachable coil embolization. Surgeons who perform suction thrombectomy should keep in mind the possibility of vessel injury that results in the formation of a pseudoaneurysm, especially at the branching site or tortuous segments.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Delayed Rupture of an Anterior Communicating Artery Pseudoaneurysm Caused by Distal Occlusion Thrombectomy Using a Stent Retriever: A Case Report and Mechanism of Injury
Dong-Hyun Shim, Youngrok Do, Jin Kuk Do, Sung Won Youn
Neurointervention. 2022;17(2):121-125. doi: 10.5469/neuroint.2022.00101.
Reference
-
1. Instructions for use solitaire Fr revascularization device supplied with the device in the product package. ev3 Neurovascular, Inc. 70648-001 Rev:02-12.2. Delgado Almandoz JE, Kayan Y, Young ML, Fease JL, Scholz JM, Milner AM, et al. Comparison of clinical outcomes in patients with acute ischemic strokes treated with mechanical thrombectomy using either Solumbra or ADAPT techniques. J Neurointerv Surg. 2015; 12. 14. [Epub ahead of print].
Article3. Cohen JE, Rajz G, Itshayek E, Shoshan Y, Umansky F, Gomori JM. Endovascular management of traumatic and iatrogenic aneurysms of the pericallosal artery. Report of two cases. J Neurosurg. 2005; 3. 102(3):555–557. PMID: 15796396.4. Cohen JE, Gomori JM, Segal R, Spivak A, Margolin E, Sviri G, et al. Results of endovascular treatment of traumatic intracranial aneurysms. Neurosurgery. 2008; 9. 63(3):476–485. PMID: 18812959.
Article5. de Sousa AA, Dantas FL, de Cardoso GT, Costa BS. Distal anterior cerebral artery aneurysms. Surg neurol. 1999; 8. 52(2):128–135. discussion 135-6. PMID: 10447278.
Article6. Eom YI, Hwang YH, Hong JM, Choi JW, Lim YC, Kang DH, et al. Forced arterial suction thrombectomy with the penumbra reperfusion catheter in acute basilar artery occlusion: a retrospective comparison study in 2 Korean university hospitals. AJNR Am J Neuroradiol. 2014; 12. 35(12):2354–2359. PMID: 25034774.
Article7. Frei D, Gerber J, Turk A, McPherson M, Heck D, Hui F, et al. The SPEED study: initial clinical evaluation of the Penumbra novel 054 Reperfusion Catheter. J Neurointerv Surg. 2013; 5. 5(Suppl 1):i74–i76. PMID: 23299104.
Article8. Jankowitz B, Aghaebrahim A, Zirra A, Spataru O, Zaidi S, Jumaa M, et al. Manual aspiration thrombectomy: adjunctive endovascular recanalization technique in acute stroke interventions. Stroke. 2012; 5. 43(5):1408–1411. PMID: 22382156.9. John S, Hussain MS, Toth G, Bain M, Uchino K, Hui FK. Initial Experience using the 5MAX™ ACE reperfusion catheter in Intra-Arterial therapy for acute ischemic stroke. J Cerebrovasc Endovasc Neurosurg. 2014; 12. 16(4):350–357. PMID: 25599043.
Article10. Kang DH, Hwang YH, Kim YS, Park J, Kwon O, Jung C. Direct thrombus retrieval using the reperfusion catheter of the penumbra system: forced-suction thrombectomy in acute ischemic stroke. AJNR Am J Neuroradiol. 2011; 2. 32(2):283–287. PMID: 21087940.
Article11. Kim SK, Yoon W, Moon SM, Park MS, Jeong GW, Kang HK. Outcomes of manual aspiration thrombectomy for acute ischemic stroke refractory to stent-based thrombectomy. J Neurointerv Surg. 2015; 7. 7(7):473–477. PMID: 24811741.12. Kowoll A, Weber A, Mpotsaris A, Behme D, Weber W. Direct aspiration first pass technique for the treatment of acute ischemic stroke: initial experience at a European stroke center. J Neurointerv Surg. 2016; 3. 8(3):230–234. PMID: 25583533.
Article13. Navia P, Larrea JA, Pardo E, Arce A, Martínez-Zabaleta M, Díez-González N, et al. Initial experience using the 3MAX cerebral reperfusion catheter in the endovascular treatment of acute ischemic stroke of distal arteries. J Neurointerv Surg. 2016; 8. 8(8):787–790. PMID: 26180095.
Article14. Shindo A, Kawanishi M, Kawakita K, Okauchi M, Kawai N, Hayashi N, et al. Treatment of acute cerebral artery occlusion using the Penumbra system: our early experience. Neurol Med Chir (Tokyo). 2014; 6. 54(6):441–449. PMID: 24759097.
Article15. Son S, Choi DS, Oh MK, Hong J, Kim SK, Kang H, et al. Comparison of Solitaire thrombectomy and Penumbra suction thrombectomy in patients with acute ischemic stroke caused by basilar artery occlusion. J Neurointerv Surg. 2016; 1. 8(1):13–18. PMID: 25411420.
Article16. Sui M, Mei Q, Sun K. Surgical treatment achieves better outcome in severe traumatic pericallosal aneurysm: case report and literature review. Int J Clin Exp Med. 2015; 2. 8(2):1598–1603. PMID: 25932088.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Forced Arterial Suction Thrombectomy Using Distal Access Catheter in Acute Ischemic Stroke
- Suction thrombectomy of distal medium vessel occlusion using microcatheter during mechanical thrombectomy for acute ischemic stroke: A case series
- Real-Time Visualization of Thrombus during Suction Thrombectomy : Contrast-in-Stasis Technique
- Directly Retrieved Entire Clot from Forced Suction Thrombectomy Using the Penumbra System in Acute Middle Cerebral Artery Occlusion
- Comparison of Intubation Efficiency by Suction Device in a Hemorrhagic Airway Manikin Model: Yankauer Suction Tip vs. Polyvinyl Chloride Catheter Suction Tip