Intest Res.
2024 Jan;22(1):75-81. 10.5217/ir.2023.00065.
Ischemia-modified albumin: a novel blood marker of endoscopic mucosal healing in inflammatory bowel disease
- Affiliations
-
- 1Department of Gastroenterology Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea
- 2Department of Laboratory Medicine, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea
- 3Department of Gastroenterology and Inflammatory Bowel Disease Center, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2551280
- DOI: http://doi.org/10.5217/ir.2023.00065
Abstract
- Background/Aims
The achievement of endoscopic remission is an important therapeutic goal in the treatment of inflammatory bowel diseases (IBD). We aimed to evaluate the role of fecal calprotectin (FCP) and ischemia-modified albumin (IMA) as biomarkers for evaluating IBD disease activity.
Methods
A total of 48 patients with IBD (20 with ulcerative colitis and 28 with Crohn’s disease) were included in this study. FCP and serum C-reactive protein levels, erythrocyte sedimentation rate, and IMA were measured in patients with IBD and compared with endoscopic findings.
Results
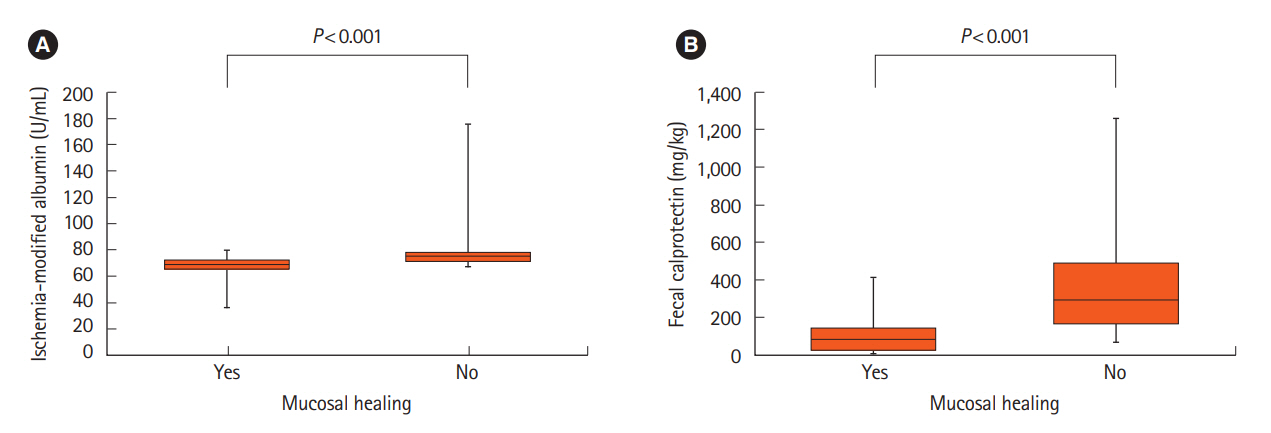
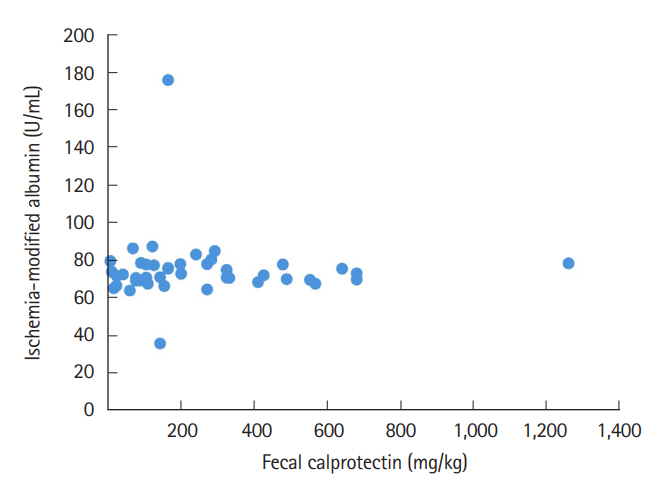
Elevated FCP and serum IMA levels were significantly associated with endoscopic non-mucosal healing. The correlation between FCP and IMA was not significant. Analysis of the receiver operating characteristic curve showed that both FCP and IMA had diagnostic value in predicting non-mucosal healing. When the Ln(FCP)+IMA/10 value was calculated using both factors, the predictive value for non-mucosal healing increased; however, no significant difference was observed.
Conclusions
IMA could be a candidate serum biomarker for predicting endoscopic mucosal healing in IBD.
Keyword
Figure
Cited by 1 articles
-
A novel serum biomarker of endoscopic mucosal healing in inflammatory bowel disease
Hyoun Woo Kang
Intest Res. 2024;22(1):3-4. doi: 10.5217/ir.2023.00198.
Reference
-
1. Turner D, Ricciuto A, Lewis A, et al. STRIDE-II: an Update on the Selecting Therapeutic Targets in Inflammatory Bowel Disease (STRIDE) Initiative of the International Organization for the Study of IBD (IOIBD): determining therapeutic goals for treat-to-target strategies in IBD. Gastroenterology. 2021; 160:1570–1583.
Article2. Pineton de Chambrun G, Peyrin-Biroulet L, Lémann M, Colombel JF. Clinical implications of mucosal healing for the management of IBD. Nat Rev Gastroenterol Hepatol. 2010; 7:15–29.
Article3. Sood A, Mahajan R, Singh A, Midha V, Mehta V. Endoscopy for assessment of mucosal healing in ulcerative colitis: time bound or response guided? Intest Res. 2022; 20:297–302.
Article4. Nardone OM, Shivaji UN, Ferruzza V, Ghosh S, Iacucci M. Soluble blood markers of mucosal healing in inflammatory bowel disease: the future of noninvasive monitoring. Inflamm Bowel Dis. 2020; 26:961–969.
Article5. Moriichi K, Fujiya M, Okumura T. The endoscopic diagnosis of mucosal healing and deep remission in inflammatory bowel disease. Dig Endosc. 2021; 33:1008–1023.
Article6. Krzystek-Korpacka M, Kempiński R, Bromke M, Neubauer K. Biochemical biomarkers of mucosal healing for inflammatory bowel disease in adults. Diagnostics (Basel). 2020; 10:367.
Article7. State M, Negreanu L, Voiosu T, Voiosu A, Balanescu P, Mateescu RB. Surrogate markers of mucosal healing in inflammatory bowel disease: a systematic review. World J Gastroenterol. 2021; 27:1828–1840.
Article8. Jeong Y, Jeon SR, Kim HG, et al. The role of platelet to lymphocyte ratio and neutrophil to lymphocyte ratio in ulcerative colitis. Intest Res. 2021; 19:62–70.
Article9. Con D, Andrew B, Nicolaides S, van Langenberg DR, Vasudevan A. Biomarker dynamics during infliximab salvage for acute severe ulcerative colitis: C-reactive protein (CRP)-lymphocyte ratio and CRP-albumin ratio are useful in predicting colectomy. Intest Res. 2022; 20:101–113.
Article10. Pavlick KP, Laroux FS, Fuseler J, et al. Role of reactive metabolites of oxygen and nitrogen in inflammatory bowel disease. Free Radic Biol Med. 2002; 33:311–322.
Article11. Rezaie A, Parker RD, Abdollahi M. Oxidative stress and pathogenesis of inflammatory bowel disease: an epiphenomenon or the cause? Dig Dis Sci. 2007; 52:2015–2021.
Article12. Bhagavan NV, Lai EM, Rios PA, et al. Evaluation of human serum albumin cobalt binding assay for the assessment of myocardial ischemia and myocardial infarction. Clin Chem. 2003; 49:581–585.
Article13. Shevtsova A, Gordiienko I, Tkachenko V, Ushakova G. Ischemia-modified albumin: origins and clinical implications. Dis Markers. 2021; 2021:9945424.
Article14. Kaplan M, Yuksel M, Ates I, et al. Is ischemia modified albumin a disease activity marker for inflammatory bowel diseases? J Gastroenterol Hepatol. 2016; 31:1120–1125.
Article15. Guntas G, Sahin A, Duran S, et al. Evaluation of ischemia-modified albumin in patients with inflammatory bowel disease. Clin Lab. 2017; 63:341–347.
Article16. Omma A, Sandikci SC, Colak S, Tecer D, Yucel C, Ozbalkan Z. Serum calprotectin and ischemia modified albumin levels as markers of disease activity in Behçet’s disease. Postepy Dermatol Alergol. 2018; 35:609–613.
Article17. Sands BE, Anderson FH, Bernstein CN, et al. Infliximab maintenance therapy for fistulizing Crohn’s disease. N Engl J Med. 2004; 350:876–885.
Article18. Daperno M, D’Haens G, Van Assche G, et al. Development and validation of a new, simplified endoscopic activity score for Crohn’s disease: the SES-CD. Gastrointest Endosc. 2004; 60:505–512.
Article19. Bar-Or D, Lau E, Winkler JV. A novel assay for cobalt-albumin binding and its potential as a marker for myocardial ischemiaa preliminary report. J Emerg Med. 2000; 19:311–315.
Article20. Schoepfer AM, Beglinger C, Straumann A, et al. Fecal calprotectin more accurately reflects endoscopic activity of ulcerative colitis than the Lichtiger Index, C-reactive protein, platelets, hemoglobin, and blood leukocytes. Inflamm Bowel Dis. 2013; 19:332–341.
Article21. Schoepfer AM, Beglinger C, Straumann A, et al. Fecal calprotectin correlates more closely with the simple endoscopic score for Crohn’s disease (SES-CD) than CRP, blood leukocytes, and the CDAI. Am J Gastroenterol. 2010; 105:162–169.
Article22. Satsangi J, Silverberg MS, Vermeire S, Colombel JF. The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications. Gut. 2006; 55:749–753.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic activity in inflammatory bowel disease: clinical significance and application in practice
- Role of Advanced Endoscopic Imaging Techniques in the Management of Inflammatory Bowel Disease
- The evolving understanding of histology as an endpoint in ulcerative colitis
- Chronological Review of Endoscopic Indices in Inflammatory Bowel Disease
- A novel serum biomarker of endoscopic mucosal healing in inflammatory bowel disease