Clin Endosc.
2019 Mar;52(2):129-136. 10.5946/ce.2018.042.
Chronological Review of Endoscopic Indices in Inflammatory Bowel Disease
- Affiliations
-
- 1Department of Internal Medicine, Kyungpook National University School of Medicine, Daegu, Korea.
- 2Department of Internal Medicine, Kosin University College of Medicine, Busan, Korea. moonone70@hanmail.net
- KMID: 2447669
- DOI: http://doi.org/10.5946/ce.2018.042
Abstract
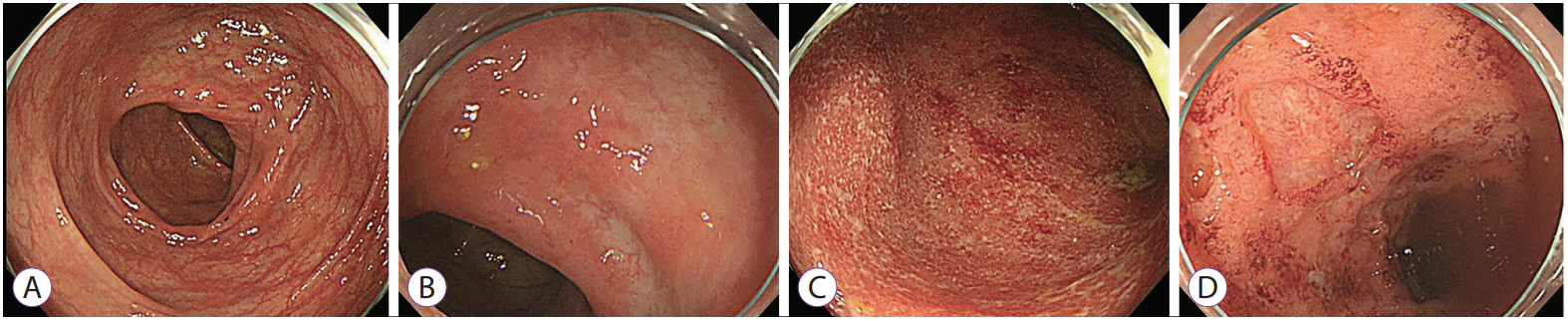
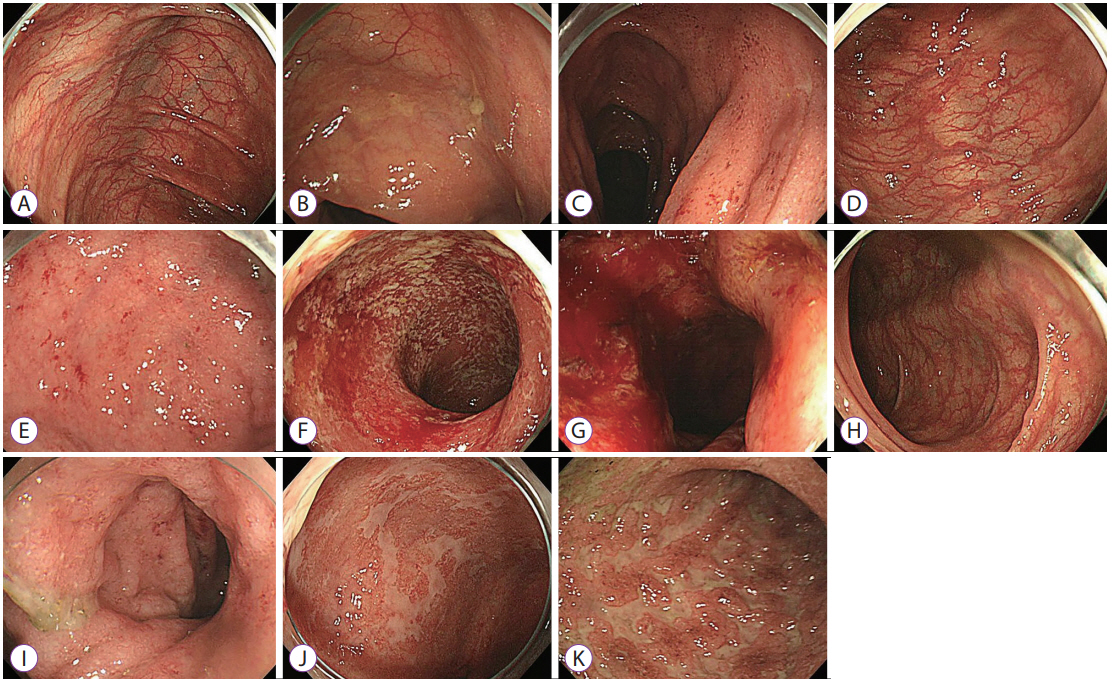
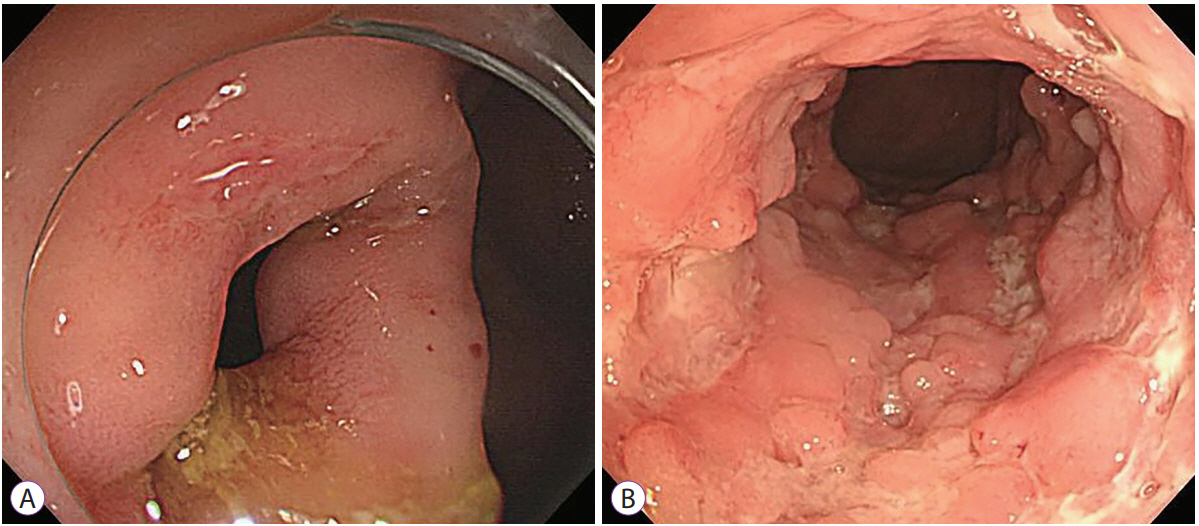
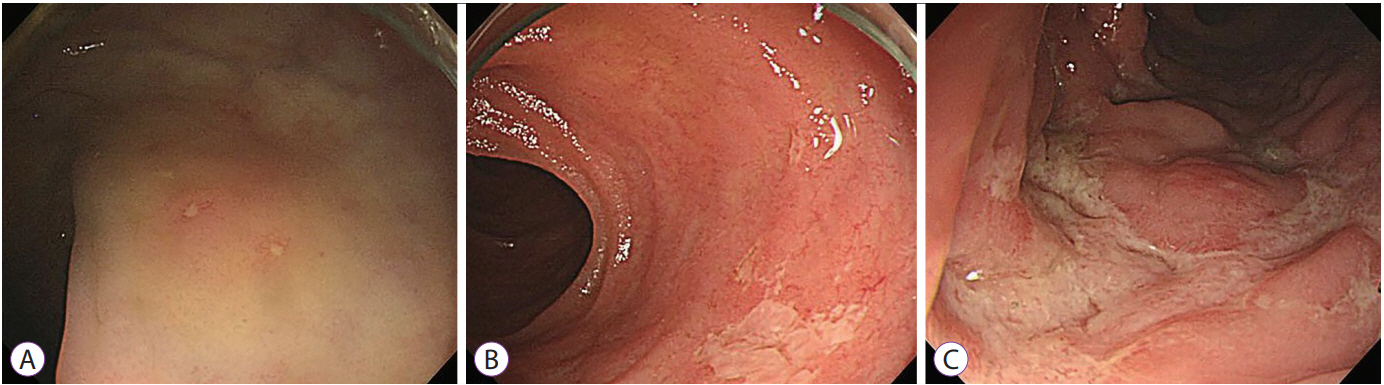
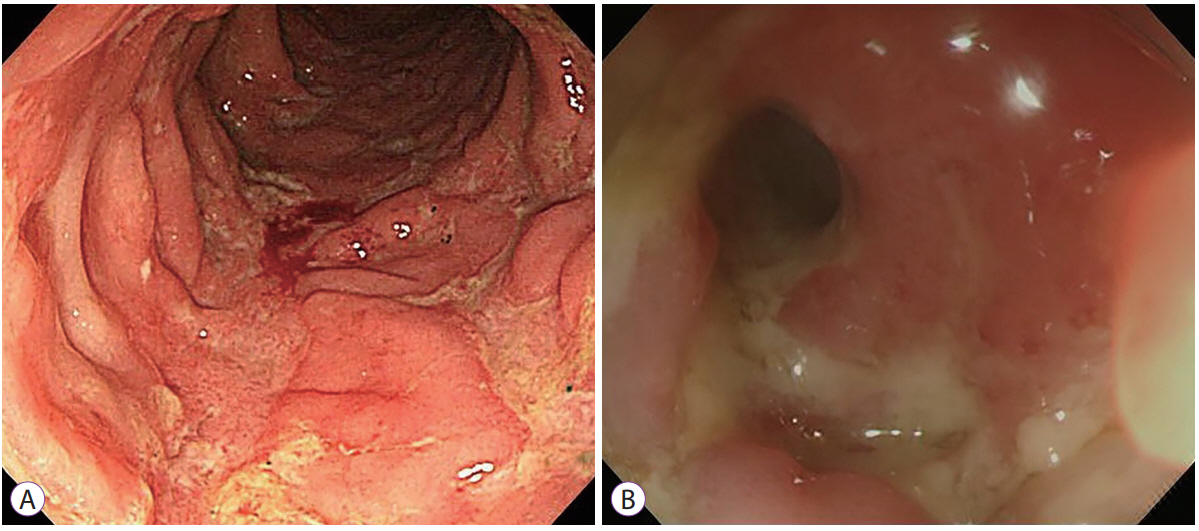
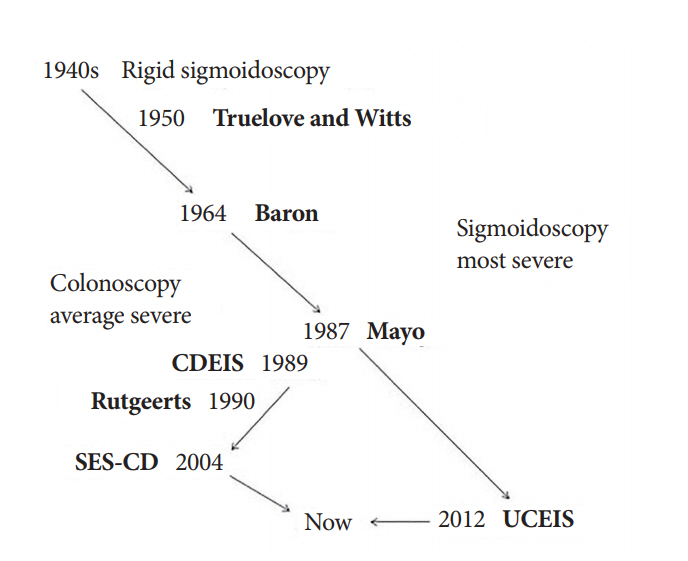
- Inflammatory bowel disease (IBD) is considered a chronic condition characterized by mucosal or transmural inflammation in the gastrointestinal tract. Endoscopic diagnosis and surveillance in patients with IBD have become crucial. In addition, endoscopy is a useful modality in estimation and evaluation of the disease, treatment results, and efficacy of treatment delivery and surveillance. In relation to these aspects, endoscopic disease activity has been commonly estimated in clinical practices and trials. At present, many endoscopic indices of ulcerative colitis have been introduced, including the Truelove and Witts Endoscopy Index, Baron Index, Powell-Tuck Index, Sutherland Index, Mayo Clinic Endoscopic Sub-Score, Rachmilewitz Index, Modified Baron Index, Endoscopic Activity Index, Ulcerative Colitis Endoscopic Index of Severity, Ulcerative Colitis Colonoscopic Index of Severity, and Modified Mayo Endoscopic Score. Endoscopic indices have been also suggested for Crohn's disease, such as the Crohn's Disease Endoscopic Index of Severity, Simple Endoscopic Score for Crohn's Disease, and Rutgeerts Postoperative Endoscopic Index. However, most endoscopic indices have not been validated owing to the complexity of their parameters and inter-observer variations. Therefore, a chronological approach for understanding the various endoscopic indices relating to IBD is needed to improve the management.
MeSH Terms
Figure
Reference
-
1. Neurath MF, Travis SP. Mucosal healing in inflammatory bowel diseases: a systematic review. Gut. 2012; 61:1619–1635.
Article2. Frøslie KF, Jahnsen J, Moum BA, Vatn MH. Mucosal healing in inflammatory bowel disease: results from a Norwegian population-based cohort. Gastroenterology. 2007; 133:412–422.
Article3. Feagan BG, Lémann M, Befrits R, et al. Recommendations for the treatment of Crohn’s disease with tumor necrosis factor antagonists: an expert consensus report. Inflamm Bowel Dis. 2012; 18:152–160.
Article4. Annese V, Daperno M, Rutter MD, et al. European evidence based consensus for endoscopy in inflammatory bowel disease. J Crohns Colitis. 2013; 7:982–1018.
Article5. Dave M, Loftus EV Jr. Mucosal healing in inflammatory bowel disease-a true paradigm of success? Gastroenterol Hepatol (N Y). 2012; 8:29–38.6. Ardizzone S, Cassinotti A, Duca P, et al. Mucosal healing predicts late outcomes after the first course of corticosteroids for newly diagnosed ulcerative colitis. Clin Gastroenterol Hepatol. 2011; 9:483–489.e3.
Article7. Peyrin-Biroulet L, Ferrante M, Magro F, et al. Results from the 2nd Scientific Workshop of the ECCO (I): impact of mucosal healing on the course of inflammatory bowel disease. J Crohns Colitis. 2011; 5:477–483.
Article8. Truelove SC, Witts LJ. Cortisone in ulcerative colitis; final report on a therapeutic trial. Br Med J. 1955; 2:1041–1048.9. Baron JH, Connell AM, Lennard-Jones JE. Variation between observers in describing mucosal appearances in proctocolitis. Br Med J. 1964; 1:89–92.
Article10. Powell-Tuck J, Day DW, Buckell NA, Wadsworth J, Lennard-Jones JE. Correlations between defined sigmoidoscopic appearances and other measures of disease activity in ulcerative colitis. Dig Dis Sci. 1982; 27:533–537.
Article11. Sutherland LR, Martin F, Greer S, et al. 5-Aminosalicylic acid enema in the treatment of distal ulcerative colitis, proctosigmoiditis, and proctitis. Gastroenterology. 1987; 92:1894–1898.
Article12. Schroeder KW, Tremaine WJ, Ilstrup DM. Coated oral 5-aminosalicylic acid therapy for mildly to moderately active ulcerative colitis. A randomized study. N Engl J Med. 1987; 317:1625–1629.13. Osada T, Ohkusa T, Yokoyama T, et al. Comparison of several activity indices for the evaluation of endoscopic activity in UC: inter- and intraobserver consistency. Inflamm Bowel Dis. 2010; 16:192–197.
Article14. Rachmilewitz D. Coated mesalazine (5-aminosalicylic acid) versus sulphasalazine in the treatment of active ulcerative colitis: a randomised trial. BMJ. 1989; 298:82–86.
Article15. Feagan BG, Greenberg GR, Wild G, et al. Treatment of ulcerative colitis with a humanized antibody to the alpha4beta7 integrin. N Engl J Med. 2005; 352:2499–2507.16. Feagan BG, Sandborn WJ, D’Haens G, et al. The role of centralized reading of endoscopy in a randomized controlled trial of mesalamine for ulcerative colitis. Gastroenterology. 2013; 145:149–157.e2.
Article17. Naganuma M, Ichikawa H, Inoue N, et al. Novel endoscopic activity index is useful for choosing treatment in severe active ulcerative colitis patients. J Gastroenterol. 2010; 45:936–943.
Article18. Travis SP, Schnell D, Krzeski P, et al. Developing an instrument to assess the endoscopic severity of ulcerative colitis: the Ulcerative Colitis Endoscopic Index of Severity (UCEIS). Gut. 2012; 61:535–542.
Article19. Travis SP, Schnell D, Krzeski P, et al. Reliability and initial validation of the ulcerative colitis endoscopic index of severity. Gastroenterology. 2013; 145:987–995.
Article20. Samuel S, Bruining DH, Loftus EV Jr, et al. Validation of the ulcerative colitis colonoscopic index of severity and its correlation with disease activity measures. Clin Gastroenterol Hepatol. 2013; 11:49–54.e1.
Article21. Lobatón T, Bessissow T, De Hertogh G, et al. The Modified Mayo Endoscopic Score (MMES): a new index for the assessment of extension and severity of endoscopic activity in ulcerative colitis patients. J Crohns Colitis. 2015; 9:846–852.
Article22. Mary JY, Modigliani R. Development and validation of an endoscopic index of the severity for Crohn’s disease: a prospective multicentre study. Groupe d’Etudes Therapeutiques des Affections Inflammatoires du Tube Digestif (GETAID). Gut. 1989; 30:983–989.
Article23. Daperno M, Comberlato M, Bossa F, et al. Inter-observer agreement in endoscopic scoring systems: preliminary report of an ongoing study from the Italian Group for Inflammatory Bowel Disease (IG-IBD). Dig Liver Dis. 2014; 46:969–973.
Article24. Daperno M, D’Haens G, Van Assche G, et al. Development and validation of a new, simplified endoscopic activity score for Crohn’s disease: the SES-CD. Gastrointest Endosc. 2004; 60:505–512.
Article25. Rutgeerts P, Geboes K, Vantrappen G, Kerremans R, Coenegrachts JL, Coremans G. Natural history of recurrent Crohn’s disease at the ileocolonic anastomosis after curative surgery. Gut. 1984; 25:665–672.
Article26. Rutgeerts P, Geboes K, Vantrappen G, Beyls J, Kerremans R, Hiele M. Predictability of the postoperative course of Crohn’s disease. Gastroenterology. 1990; 99:956–963.
Article27. Lee JM, Lee KM. Endoscopic diagnosis and differentiation of inflammatory bowel disease. Clin Endosc. 2016; 49:370–375.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic activity in inflammatory bowel disease: clinical significance and application in practice
- Non-traumatic Small Bowel Perforation: Comparisons of the Clinical Features of 20 Years Ago with Present
- Role of Advanced Endoscopic Imaging Techniques in the Management of Inflammatory Bowel Disease
- Diagnostic Tips for Making the Diagnosis of Inflammatory Bowel Disease
- Small Bowel Endoscopy in Inflammatory Bowel Disease