J Korean Med Sci.
2023 Sep;38(38):e295. 10.3346/jkms.2023.38.e295.
Triglyceride-Rich Lipoproteins and Remnant Cholesterol in Cardiovascular Disease
- Affiliations
-
- 1Division of Endocrinology, Department of Internal Medicine, Hallym University Sacred Heart Hospital, Anyang, Korea
- 2Division of Cardiology, Department of Internal Medicine, Hallym University Sacred Heart Hospital, Anyang, Korea
- KMID: 2546218
- DOI: http://doi.org/10.3346/jkms.2023.38.e295
Abstract
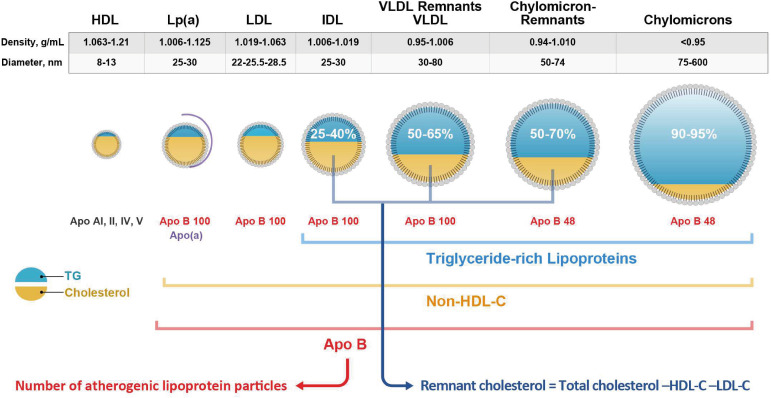
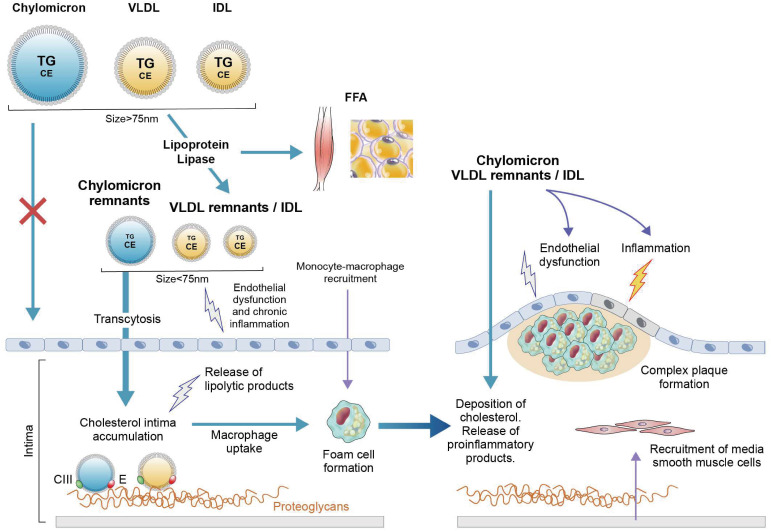
- Despite the well-established benefits of statin treatments in lowering low-density lipoprotein cholesterol (LDL-C), a significant residual risk for atherosclerotic cardiovascular disease (ASCVD) remains. Triglycerides (TGs) have long been recognized as potential residual risk factors in this context, but recent studies now disclose the substantial role of TG-rich lipoproteins (TRLs) and cholesterol components of metabolized TRLs (commonly referred to as remnant cholesterol) in atherogenesis, not just TGs alone. Evidence derived through diverse sources, including preclinical studies of pathogenic mechanisms, epidemiologic investigations, and genetic research, has consistently supported the considerable contribution of TRLs and remnant cholesterol in predicting occurrences of ASCVD. As emerging biomarkers for predicting atherosclerosis, they have thus become prioritized therapeutic targets, meant to augment LDL-C lowering efforts in individuals at high risk of ASCVD. However, routine clinical testing for remnant cholesterol and TRLs is still in question, necessitating further research into appropriate treatment plans if levels are elevated. New therapies targeting proteins in TG metabolic pathways, particularly angiopoietin-like protein 3 and apolipoprotein C-III, have shown potential advantages in patients with mild-to-moderate hypertriglyceridemia by reducing blood levels of TGs and remnant cholesterol. The aim of this review is to summarize existing evidence linking elevated TRLs and remnant cholesterol with development of ASCVD and to explore additional guidance for clinical therapy.
Figure
Reference
-
1. Wong ND, Zhao Y, Quek RGW, Blumenthal RS, Budoff MJ, Cushman M, et al. Residual atherosclerotic cardiovascular disease risk in statin-treated adults: the multi-ethnic study of atherosclerosis. J Clin Lipidol. 2017; 11(5):1223–1233. PMID: 28754224.
Article2. Nordestgaard BG, Benn M, Schnohr P, Tybjaerg-Hansen A. Nonfasting triglycerides and risk of myocardial infarction, ischemic heart disease, and death in men and women. JAMA. 2007; 298(3):299–308. PMID: 17635890.
Article3. Packard CJ. Remnants, LDL, and the quantification of lipoprotein-associated risk in atherosclerotic cardiovascular disease. Curr Atheroscler Rep. 2022; 24(3):133–142. PMID: 35175548.
Article4. Ginsberg HN, Packard CJ, Chapman MJ, Borén J, Aguilar-Salinas CA, Averna M, et al. Triglyceride-rich lipoproteins and their remnants: metabolic insights, role in atherosclerotic cardiovascular disease, and emerging therapeutic strategies-a consensus statement from the European Atherosclerosis Society. Eur Heart J. 2021; 42(47):4791–4806. PMID: 34472586.
Article5. Burnett JR, Hooper AJ, Hegele RA. Remnant cholesterol and atherosclerotic cardiovascular disease risk. J Am Coll Cardiol. 2020; 76(23):2736–2739. PMID: 33272367.
Article6. Huet F, Roubille C, Roubille F. Is hypertriglyceridemia atherogenic? Curr Opin Lipidol. 2019; 30(4):291–299. PMID: 31145120.
Article7. Kulkarni KR. Cholesterol profile measurement by vertical auto profile method. Clin Lab Med. 2006; 26(4):787–802. PMID: 17110240.
Article8. Balling M, Afzal S, Varbo A, Langsted A, Davey Smith G, Nordestgaard BG. VLDL cholesterol accounts for one-half of the risk of myocardial infarction associated with apoB-containing lipoproteins. J Am Coll Cardiol. 2020; 76(23):2725–2735. PMID: 33272366.
Article9. Jepsen AM, Langsted A, Varbo A, Bang LE, Kamstrup PR, Nordestgaard BG. Increased remnant cholesterol explains part of residual risk of all-cause mortality in 5414 patients with ischemic heart disease. Clin Chem. 2016; 62(4):593–604. PMID: 26888894.
Article10. Varbo A, Nordestgaard BG. Directly measured vs. calculated remnant cholesterol identifies additional overlooked individuals in the general population at higher risk of myocardial infarction. Eur Heart J. 2021; 42(47):4833–4843. PMID: 34023898.
Article11. Martin SS, Blaha MJ, Elshazly MB, Toth PP, Kwiterovich PO, Blumenthal RS, et al. Comparison of a novel method vs the Friedewald equation for estimating low-density lipoprotein cholesterol levels from the standard lipid profile. JAMA. 2013; 310(19):2061–2068. PMID: 24240933.
Article12. Castañer O, Pintó X, Subirana I, Amor AJ, Ros E, Hernáez Á, et al. Remnant cholesterol, not LDL cholesterol, is associated with incident cardiovascular disease. J Am Coll Cardiol. 2020; 76(23):2712–2724. PMID: 33272365.
Article13. Wadström BN, Wulff AB, Pedersen KM, Jensen GB, Nordestgaard BG. Elevated remnant cholesterol increases the risk of peripheral artery disease, myocardial infarction, and ischaemic stroke: a cohort-based study. Eur Heart J. 2022; 43(34):3258–3269. PMID: 34661640.
Article14. Huh JH, Han KD, Cho YK, Roh E, Kang JG, Lee SJ, et al. Remnant cholesterol and the risk of cardiovascular disease in type 2 diabetes: a nationwide longitudinal cohort study. Cardiovasc Diabetol. 2022; 21(1):228. PMID: 36324177.
Article15. Lee SJ, Kim SE, Go TH, Kang DR, Jeon HS, Kim YI, et al. Remnant cholesterol, LDL cholesterol and incident cardiovascular disease among Koreans: a national population-based study. Eur J Prev Cardiol. 2023; zwad036.16. Langsted A, Madsen CM, Nordestgaard BG. Contribution of remnant cholesterol to cardiovascular risk. J Intern Med. 2020; 288(1):116–127. PMID: 32181933.
Article17. Yang J, Wang Y, Xi Z, Ma Y, Shao C, Wang W, et al. Remnant-like particle cholesterol and the risk of major adverse cardiovascular events: a systematic review and meta-analysis. J Cardiovasc Dev Dis. 2022; 9(12):452. PMID: 36547449.
Article18. Varbo A, Benn M, Tybjærg-Hansen A, Jørgensen AB, Frikke-Schmidt R, Nordestgaard BG. Remnant cholesterol as a causal risk factor for ischemic heart disease. J Am Coll Cardiol. 2013; 61(4):427–436. PMID: 23265341.
Article19. Khera AV, Won HH, Peloso GM, O’Dushlaine C, Liu D, Stitziel NO, et al. Association of rare and common variation in the lipoprotein lipase gene with coronary artery disease. JAMA. 2017; 317(9):937–946. PMID: 28267856.
Article20. Stitziel NO, Khera AV, Wang X, Bierhals AJ, Vourakis AC, Sperry AE, et al. ANGPTL3 deficiency and protection against coronary artery disease. J Am Coll Cardiol. 2017; 69(16):2054–2063. PMID: 28385496.
Article21. Jørgensen AB, Frikke-Schmidt R, Nordestgaard BG, Tybjærg-Hansen A. Loss-of-function mutations in APOC3 and risk of ischemic vascular disease. N Engl J Med. 2014; 371(1):32–41. PMID: 24941082.
Article22. Ference BA, Kastelein JJ, Ray KK, Ginsberg HN, Chapman MJ, Packard CJ, et al. Association of triglyceride-lowering LPL variants and LDL-C-lowering LDLR variants with risk of coronary heart disease. JAMA. 2019; 321(4):364–373. PMID: 30694319.
Article23. Helgadottir A, Gretarsdottir S, Thorleifsson G, Hjartarson E, Sigurdsson A, Magnusdottir A, et al. Variants with large effects on blood lipids and the role of cholesterol and triglycerides in coronary disease. Nat Genet. 2016; 48(6):634–639. PMID: 27135400.
Article24. Borén J, Chapman MJ, Krauss RM, Packard CJ, Bentzon JF, Binder CJ, et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease: pathophysiological, genetic, and therapeutic insights: a consensus statement from the European Atherosclerosis Society Consensus Panel. Eur Heart J. 2020; 41(24):2313–2330. PMID: 32052833.
Article25. Doi T, Nordestgaard BG, Langsted A. Can remnant cholesterol (triglyceride-rich lipoproteins) reclassify estimated risk of atherosclerotic cardiovascular disease? Curr Opin Endocrinol Diabetes Obes. 2023; 30(2):128–135. PMID: 36722437.
Article26. Schwartz EA, Reaven PD. Lipolysis of triglyceride-rich lipoproteins, vascular inflammation, and atherosclerosis. Biochim Biophys Acta. 2012; 1821(5):858–866. PMID: 22001233.
Article27. Higgins LJ, Rutledge JC. Inflammation associated with the postprandial lipolysis of triglyceride-rich lipoproteins by lipoprotein lipase. Curr Atheroscler Rep. 2009; 11(3):199–205. PMID: 19361351.
Article28. Doi H, Kugiyama K, Oka H, Sugiyama S, Ogata N, Koide SI, et al. Remnant lipoproteins induce proatherothrombogenic molecules in endothelial cells through a redox-sensitive mechanism. Circulation. 2000; 102(6):670–676. PMID: 10931808.
Article29. de Sousa JC, Soria C, Ayrault-Jarrier M, Pastier D, Bruckert E, Amiral J, et al. Association between coagulation factors VII and X with triglyceride rich lipoproteins. J Clin Pathol. 1988; 41(9):940–944. PMID: 3056986.
Article30. Wang L, Gill R, Pedersen TL, Higgins LJ, Newman JW, Rutledge JC. Triglyceride-rich lipoprotein lipolysis releases neutral and oxidized FFAs that induce endothelial cell inflammation. J Lipid Res. 2009; 50(2):204–213. PMID: 18812596.
Article31. Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. 2019 ESC/EAS guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020; 41(1):111–188. PMID: 31504418.32. Frick MH, Elo O, Haapa K, Heinonen OP, Heinsalmi P, Helo P, et al. Helsinki Heart Study: primary-prevention trial with gemfibrozil in middle-aged men with dyslipidemia. Safety of treatment, changes in risk factors, and incidence of coronary heart disease. N Engl J Med. 1987; 317(20):1237–1245. PMID: 3313041.
Article33. Keech A, Simes RJ, Barter P, Best J, Scott R, Taskinen MR, et al. Effects of long-term fenofibrate therapy on cardiovascular events in 9795 people with type 2 diabetes mellitus (the FIELD study): randomised controlled trial. Lancet. 2005; 366(9500):1849–1861. PMID: 16310551.
Article34. ACCORD Study Group. Ginsberg HN, Elam MB, Lovato LC, Crouse JR 3rd, Leiter LA, et al. Effects of combination lipid therapy in type 2 diabetes mellitus. N Engl J Med. 2010; 362(17):1563–1574. PMID: 20228404.
Article35. Jun M, Foote C, Lv J, Neal B, Patel A, Nicholls SJ, et al. Effects of fibrates on cardiovascular outcomes: a systematic review and meta-analysis. Lancet. 2010; 375(9729):1875–1884. PMID: 20462635.
Article36. Van Regemorter E, Jadoul M, Gillion V. Triglyceride lowering with pemafibrate to reduce cardiovascular risk. N Engl J Med. 2023; 388(10):954–955. PMID: 36884330.
Article37. Witztum JL, Gaudet D, Freedman SD, Alexander VJ, Digenio A, Williams KR, et al. Volanesorsen and triglyceride levels in familial chylomicronemia syndrome. N Engl J Med. 2019; 381(6):531–542. PMID: 31390500.
Article38. Tardif JC, Karwatowska-Prokopczuk E, Amour ES, Ballantyne CM, Shapiro MD, Moriarty PM, et al. Apolipoprotein C-III reduction in subjects with moderate hypertriglyceridaemia and at high cardiovascular risk. Eur Heart J. 2022; 43(14):1401–1412. PMID: 35025993.
Article39. Raal FJ, Rosenson RS, Reeskamp LF, Hovingh GK, Kastelein JJ, Rubba P, et al. Evinacumab for homozygous familial hypercholesterolemia. N Engl J Med. 2020; 383(8):711–720. PMID: 32813947.
Article40. Adam RC, Mintah IJ, Alexa-Braun CA, Shihanian LM, Lee JS, Banerjee P, et al. Angiopoietin-like protein 3 governs LDL-cholesterol levels through endothelial lipase-dependent VLDL clearance. J Lipid Res. 2020; 61(9):1271–1286. PMID: 32646941.
Article41. Gaudet D, Karwatowska-Prokopczuk E, Baum SJ, Hurh E, Kingsbury J, Bartlett VJ, et al. Vupanorsen, an N-acetyl galactosamine-conjugated antisense drug to ANGPTL3 mRNA, lowers triglycerides and atherogenic lipoproteins in patients with diabetes, hepatic steatosis, and hypertriglyceridaemia. Eur Heart J. 2020; 41(40):3936–3945. PMID: 32860031.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hypertriglyceridemia and Cardiovascular Diseases: Revisited
- Relationship between Childhood and Adolescent Obesity and Remnant Lipoprotein
- Hypertriglyceridemia in Obese Children and Adolescents
- Serum Lipoprotein Composition in Diabetes Mellitus
- The Correlation between the Triglyceride to High Density Lipoprotein Cholesterol Ratio and Computed Tomography-Measured Visceral Fat and Cardiovascular Disease Risk Factors in Local Adult Male Subjects