Korean J Orthod.
2023 Jul;53(4):219-231. 10.4041/kjod23.015.
Differences in positions of cone-beam computed tomography landmarks in patients with skeletal Class III facial asymmetry according to midsagittal planes
- Affiliations
-
- 1Department of Orthodontics, School of Dentistry, Kyungpook National University, Daegu, Korea
- KMID: 2545038
- DOI: http://doi.org/10.4041/kjod23.015
Abstract
Objective
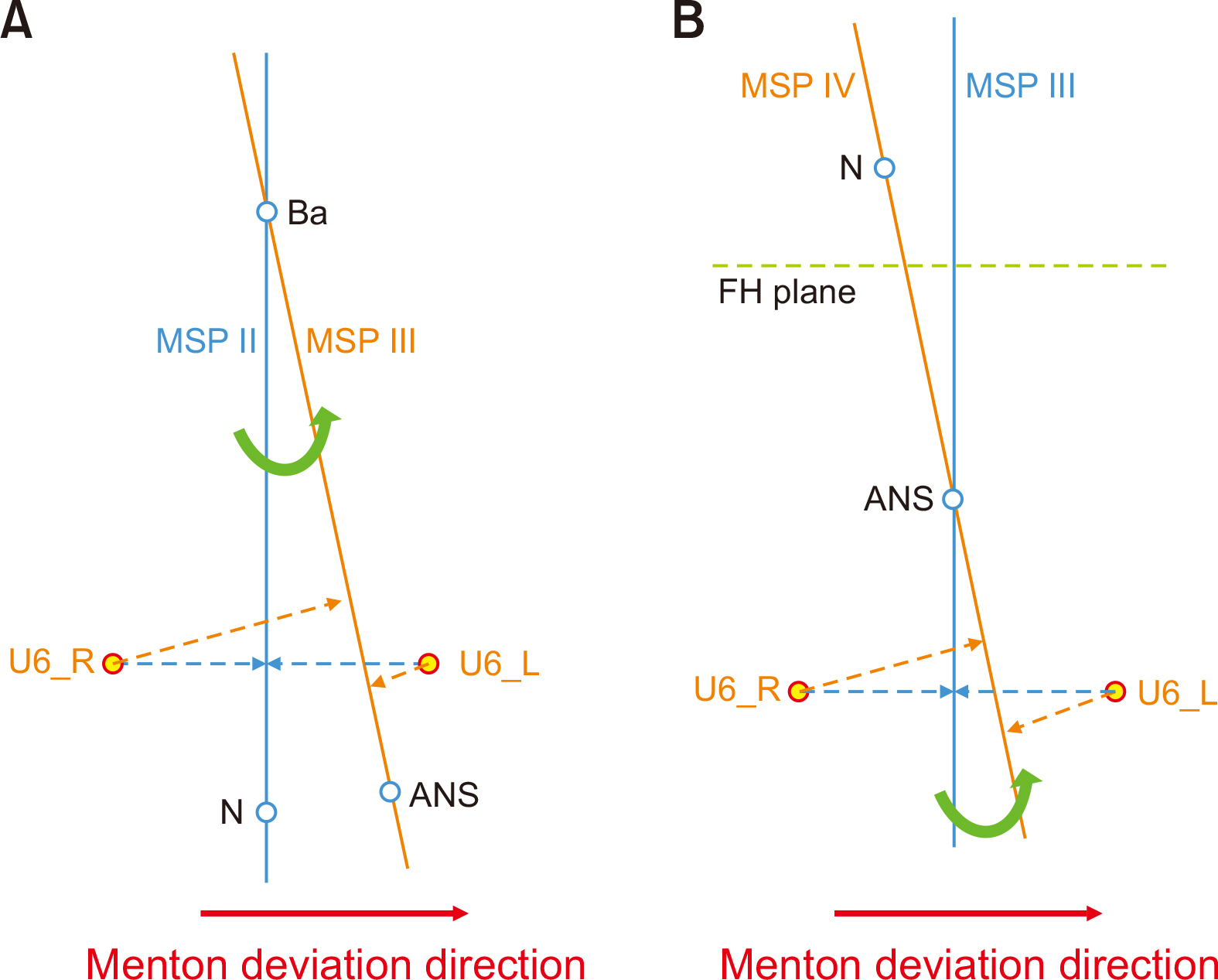
This study aimed to clarify differences in the positions of cone-beam computed tomography (CBCT) landmarks according to different midsagittal planes (MSPs) in patients with skeletal Class III facial asymmetry.
Methods
Pre-treatment CBCT data from 60 patients with skeletal Class III were used. The patients were classified into symmetric (menton deviations of < 2 mm) or asymmetric (menton deviations of > 4 mm) groups. Six MSPs were established based on previous studies, and three-dimensional analyses were performed for the planes in both the groups. The measurement outcomes were compared statistically.
Results
A statistically significant interaction (p < 0.01) was observed between MSPs and facial asymmetry. No significant differences were observed among MSPs in the symmetric group. However, significant differences in linear measurements were identified among MSPs in the asymmetric group. Specifically, the upper facial MSP revealed both maxillary and mandibular transverse asymmetries. On the other hand, anterior nasal spine (ANS)-associated MSP could not identify maxillary asymmetry. Furthermore, the menton deviation was approximately 3 mm lower when estimated using the ANS-associated MSP than that using upper facial MSP.
Conclusions
The choice of MSP can significantly affect treatment outcomes while diagnosing patients with asymmetry. Therefore, care should be taken when selecting MSP in clinical practice.
Figure
Reference
-
1. Hajeer MY, Ayoub AF, Millett DT. 2004; Three-dimensional assessment of facial soft-tissue asymmetry before and after orthognathic surgery. Br J Oral Maxillofac Surg. 42:396–404. https://doi.org/10.1016/j.bjoms.2004.05.006. DOI: 10.1016/j.bjoms.2004.05.006. PMID: 15336764.
Article2. Damstra J, Fourie Z, De Wit M, Ren Y. 2012; A three-dimensional comparison of a morphometric and conventional cephalometric midsagittal planes for craniofacial asymmetry. Clin Oral Investig. 16:285–94. https://doi.org/10.1007/s00784-011-0512-4. DOI: 10.1007/s00784-011-0512-4. PMID: 21271348. PMCID: PMC3259389.
Article3. Shin SM, Kim YM, Kim NR, Choi YS, Park SB, Kim YI. 2016; Statistical shape analysis-based determination of optimal midsagittal reference plane for evaluation of facial asymmetry. Am J Orthod Dentofacial Orthop. 150:252–60. https://doi.org/10.1016/j.ajodo.2016.01.017. DOI: 10.1016/j.ajodo.2016.01.017. PMID: 27476357.
Article4. Green MN, Bloom JM, Kulbersh R. 2017; A simple and accurate craniofacial midsagittal plane definition. Am J Orthod Dentofacial Orthop. 152:355–63. https://doi.org/10.1016/j.ajodo.2016.12.025. DOI: 10.1016/j.ajodo.2016.12.025. PMID: 28863916.
Article5. Dobai A, Markella Z, Vízkelety T, Fouquet C, Rosta A, Barabás J. 2018; Landmark-based midsagittal plane analysis in patients with facial symmetry and asymmetry based on CBCT analysis tomography. J Orofac Orthop. 79:371–9. https://doi.org/10.1007/s00056-018-0151-3. DOI: 10.1007/s00056-018-0151-3. PMID: 30255320.6. Yoon KW, Yoon SJ, Kang BC, Kim YH, Kook MS, Lee JS, et al. 2014; Deviation of landmarks in accordance with methods of establishing reference planes in three-dimensional facial CT evaluation. Imaging Sci Dent. 44:207–12. https://doi.org/10.5624/isd.2014.44.3.207. DOI: 10.5624/isd.2014.44.3.207. PMID: 25279341. PMCID: PMC4182355.7. Kim TY, Baik JS, Park JY, Chae HS, Huh KH, Choi SC. 2011; Determination of midsagittal plane for evaluation of facial asymmetry using three-dimensional computed tomography. Imaging Sci Dent. 41:79–84. https://doi.org/10.5624/isd.2011.41.2.79. DOI: 10.5624/isd.2011.41.2.79. PMID: 21977479. PMCID: PMC3174462.8. Kim HJ, Kim BC, Kim JG, Zhengguo P, Kang SH, Lee SH. 2014; Construction and validation of the midsagittal reference plane based on the skull base symmetry for three-dimensional cephalometric craniofacial analysis. J Craniofac Surg. 25:338–42. https://doi.org/10.1097/SCS.0000000000000380. DOI: 10.1097/SCS.0000000000000380. PMID: 24469365.9. An S, Lee JY, Chung CJ, Kim KH. 2017; Comparison of different midsagittal plane configurations for evaluating craniofacial asymmetry by expert preference. Am J Orthod Dentofacial Orthop. 152:788–97. https://doi.org/10.1016/j.ajodo.2017.04.024. DOI: 10.1016/j.ajodo.2017.04.024. PMID: 29173858.10. Grissom MK, Gateno J, English JD, Jacob HB, Kuang T, Gonzalez CE, et al. 2022; Midsagittal plane first: building a strong facial reference frame for computer-aided surgical simulation. J Oral Maxillofac Surg. 80:641–50. https://doi.org/10.1016/j.joms.2021.11.016. DOI: 10.1016/j.joms.2021.11.016. PMID: 34942153. PMCID: PMC8983510.11. Lee EH, Yu HS, Lee KJ, Han SS, Jung HD, Hwang CJ. 2020; Comparison of three midsagittal planes for three-dimensional cone beam computed tomography head reorientation. Korean J Orthod. 50:3–12. https://doi.org/10.4041/kjod.2020.50.1.3. DOI: 10.4041/kjod.2020.50.1.3. PMID: 32042715. PMCID: PMC6995832.12. Cho HJ. 2009; A three-dimensional cephalometric analysis. J Clin Orthod. 43:235–52. discussion 235quiz 273https://pubmed.ncbi.nlm.nih.gov/19458456/. PMID: 19458456.13. Trpkova B, Prasad NG, Lam EW, Raboud D, Glover KE, Major PW. 2003; Assessment of facial asymmetries from posteroanterior cephalograms: validity of reference lines. Am J Orthod Dentofacial Orthop. 123:512–20. https://doi.org/10.1016/S0889-5406(02)57034-7. DOI: 10.1016/S0889-5406(02)57034-7. PMID: 12750669.14. Field A. Carmichael M, editor. 2013. Repeated-measures designs (GLM 4). Discovering statistics using IBM SPSS statistics. 4th ed. Sage;London: p. 543–90.15. Nagasaka S, Fujimura T, Segoshi K. 2003; Development of a non-radiographic cephalometric system. Eur J Orthod. 25:77–85. https://doi.org/10.1093/ejo/25.1.77. DOI: 10.1093/ejo/25.1.77. PMID: 12608727.16. Kwon TG, Park HS, Ryoo HM, Lee SH. 2006; A comparison of craniofacial morphology in patients with and without facial asymmetry--a three-dimensional analysis with computed tomography. Int J Oral Maxillofac Surg. 35:43–8. https://doi.org/10.1016/j.ijom.2005.04.006. DOI: 10.1016/j.ijom.2005.04.006. PMID: 15925488.17. Williams RP, Rinchuse DJ, Zullo TG. 2014; Perceptions of midline deviations among different facial types. Am J Orthod Dentofacial Orthop. 145:249–55. https://doi.org/10.1016/j.ajodo.2013.02.034. DOI: 10.1016/j.ajodo.2013.02.034. PMID: 24485740.18. Johnston CD, Burden DJ, Stevenson MR. 1999; The influence of dental to facial midline discrepancies on dental attractiveness ratings. Eur J Orthod. 21:517–22. https://doi.org/10.1093/ejo/21.5.517. DOI: 10.1093/ejo/21.5.517. PMID: 10565092.19. Kim KS, Kim YJ, Lee KH, Kim YH, Kook YA. 2006; Level of perception of changed lip protrusion and asymmetry of the lower facial height. Korean J Orthod. 36:434–41. https://scienceon.kisti.re.kr/commons/util/originalView.do?cn=JAKO200609906156890&oCn=JAKO200609906156890&dbt=JAKO&journal=NJOU00293807.20. Noh HK, Park HS. 2021; Does maxillary yaw exist in patients with skeletal Class III facial asymmetry? Am J Orthod Dentofacial Orthop. 160:573–87. https://doi.org/10.1016/j.ajodo.2020.05.025. DOI: 10.1016/j.ajodo.2020.05.025. PMID: 34332794.21. Haraguchi S, Takada K, Yasuda Y. 2002; Facial asymmetry in subjects with skeletal Class III deformity. Angle Orthod. 72:28–35. https://pubmed.ncbi.nlm.nih.gov/11843270/. DOI: 10.1043/0003-3219(2002)072<0028:FAISWS>2.0.CO;2. PMID: 11843270.22. Posnick JC, Fantuzzo JJ, Orchin JD. 2006; Deliberate operative rotation of the maxillo-mandibular complex to alter the A-point to B-point relationship for enhanced facial esthetics. J Oral Maxillofac Surg. 64:1687–95. https://doi.org/10.1016/j.joms.2005.11.118. DOI: 10.1016/j.joms.2005.11.118. PMID: 17052598.23. Tyan S, Park HS, Janchivdorj M, Han SH, Kim SJ, Ahn HW. 2016; Three-dimensional analysis of molar compensation in patients with facial asymmetry and mandibular prognathism. Angle Orthod. 86:421–30. https://doi.org/10.2319/030915-142.1. DOI: 10.2319/030915-142.1. PMID: 26192894. PMCID: PMC8601728.24. Ahn J, Kim SJ, Lee JY, Chung CJ, Kim KH. 2017; Transverse dental compensation in relation to sagittal and transverse skeletal discrepancies in skeletal Class III patients. Am J Orthod Dentofacial Orthop. 151:148–56. https://doi.org/10.1016/j.ajodo.2016.06.031. DOI: 10.1016/j.ajodo.2016.06.031. PMID: 28024769.25. Kim HJ, Hong M, Park HS. 2019; Analysis of dental compensation in patients with facial asymmetry using cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 156:493–501. https://doi.org/10.1016/j.ajodo.2018.10.025. DOI: 10.1016/j.ajodo.2018.10.025. PMID: 31582121.26. Lee JY, Han SH, Ryu HS, Lee HM, Kim SC. 2018; Cone-beam computed tomography analysis of transverse dental compensation in patients with skeletal Class III malocclusion and facial asymmetry. Korean J Orthod. 48:357–66. https://doi.org/10.4041/kjod.2018.48.6.357. DOI: 10.4041/kjod.2018.48.6.357. PMID: 30450328. PMCID: PMC6234112.27. Marianetti TM, Boccieri A, Pascali M. 2016; Reshaping of the anterior nasal spine: an important step in rhinoplasty. Plast Reconstr Surg Glob Open. 4:e1026. https://doi.org/10.1097/GOX.0000000000001026. DOI: 10.1097/GOX.0000000000001026. PMID: 27757343. PMCID: PMC5055009.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cone-beam computed tomography analysis of transverse dental compensation in patients with skeletal Class III malocclusion and facial asymmetry
- Differences in facial soft tissue deviations in Class III patients with different types of mandibular asymmetry: A cone-beam computed tomography study
- Comparison of three midsagittal planes for three-dimensional cone beam computed tomography head reorientation
- Cone-beam computed tomography based evaluation of rotational patterns of dentofacial structures in skeletal Class III deformity with mandibular asymmetry
- Determination of midsagittal plane for evaluation of facial asymmetry using three-dimensional computed tomography