Korean J Orthod.
2023 Nov;53(6):402-419. 10.4041/kjod23.106.
Differences in facial soft tissue deviations in Class III patients with different types of mandibular asymmetry: A cone-beam computed tomography study
- Affiliations
-
- 1Department of Orthodontics, School of Dentistry, Kyungpook National University, Daegu, Korea
- KMID: 2548484
- DOI: http://doi.org/10.4041/kjod23.106
Abstract
Objective
This study assessed the differences in soft tissue deviations of the nose, lips, and chin between different mandibular asymmetry types in Class III patients.
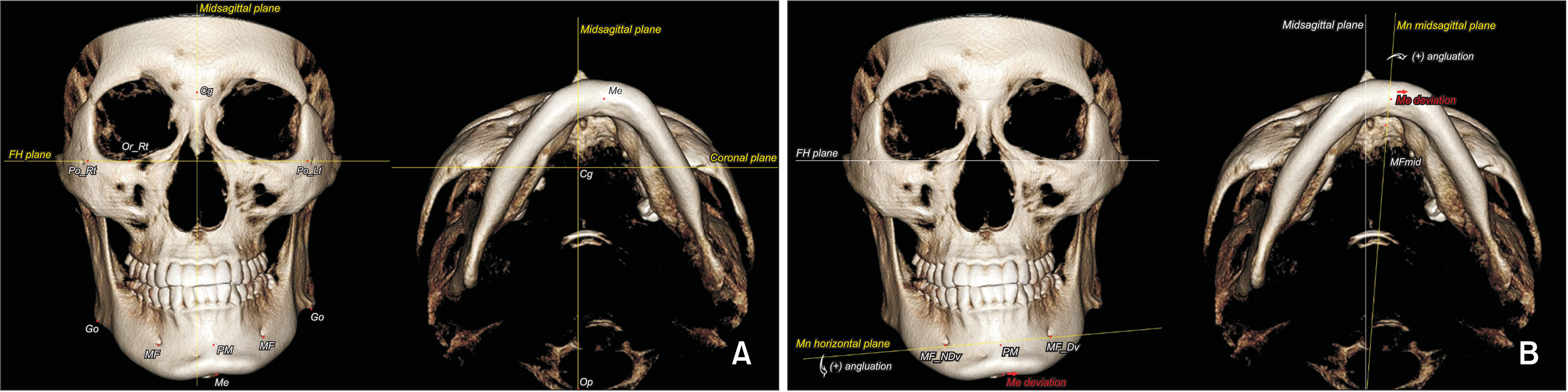
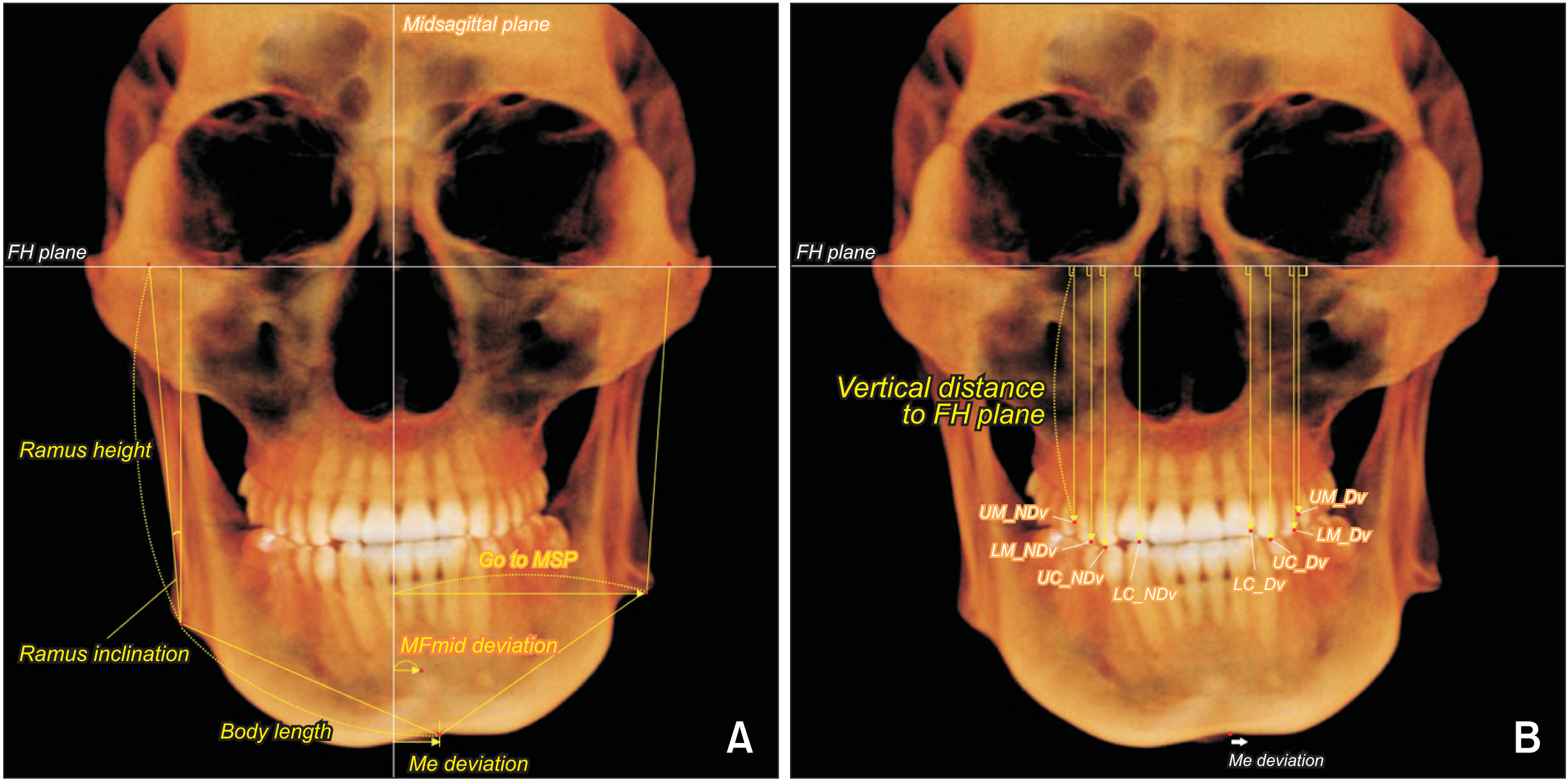
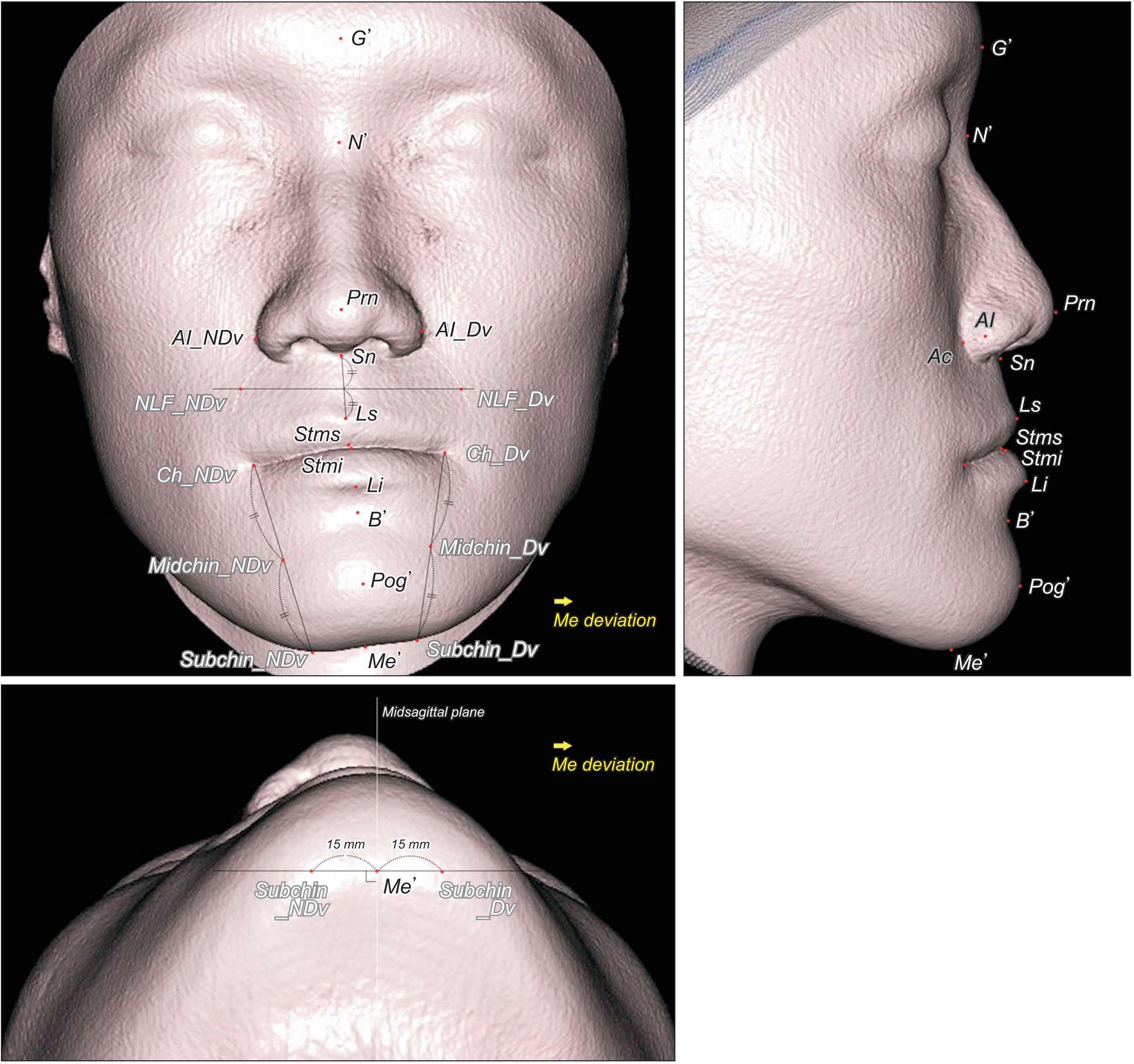
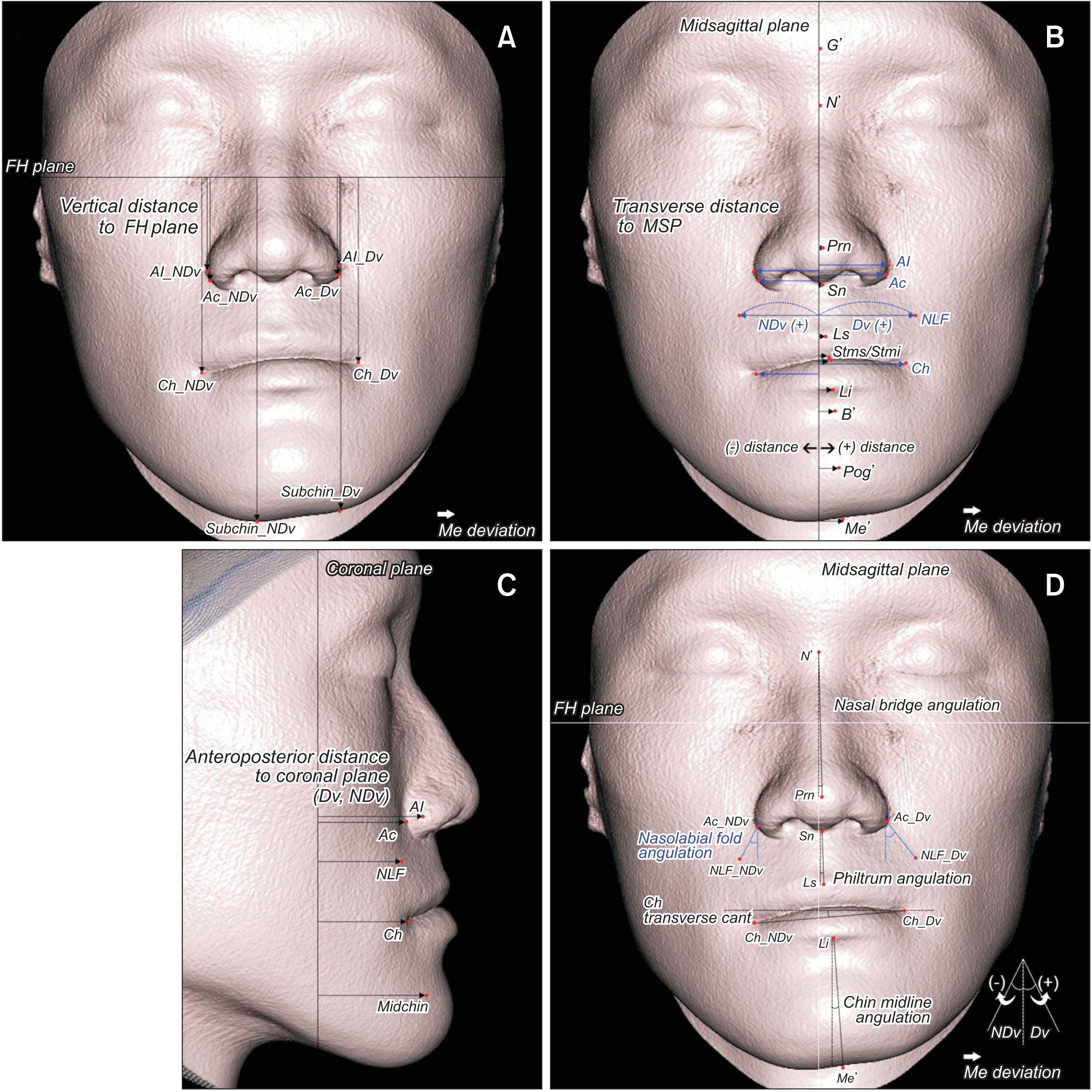
Methods
Cone-beam computed tomography data from 90 Class III patients with moderate-to-severe facial asymmetry were investigated. The sample was divided into three groups based on the extent of mandibular rolling, yawing, and translation. Soft tissue landmarks on the nose, lips, and chin were investigated vertically, transversely, and anteroposteriorly. A paired t test was performed to compare variables between the deviated (Dv) and nondeviated (NDv) sides, and one-way analysis of variance with Tukey’s post-hoc test was performed for intergroup comparisons. Pearson’s correlation coefficient was calculated to assess the relationship between the soft and hard tissue deviations.
Results
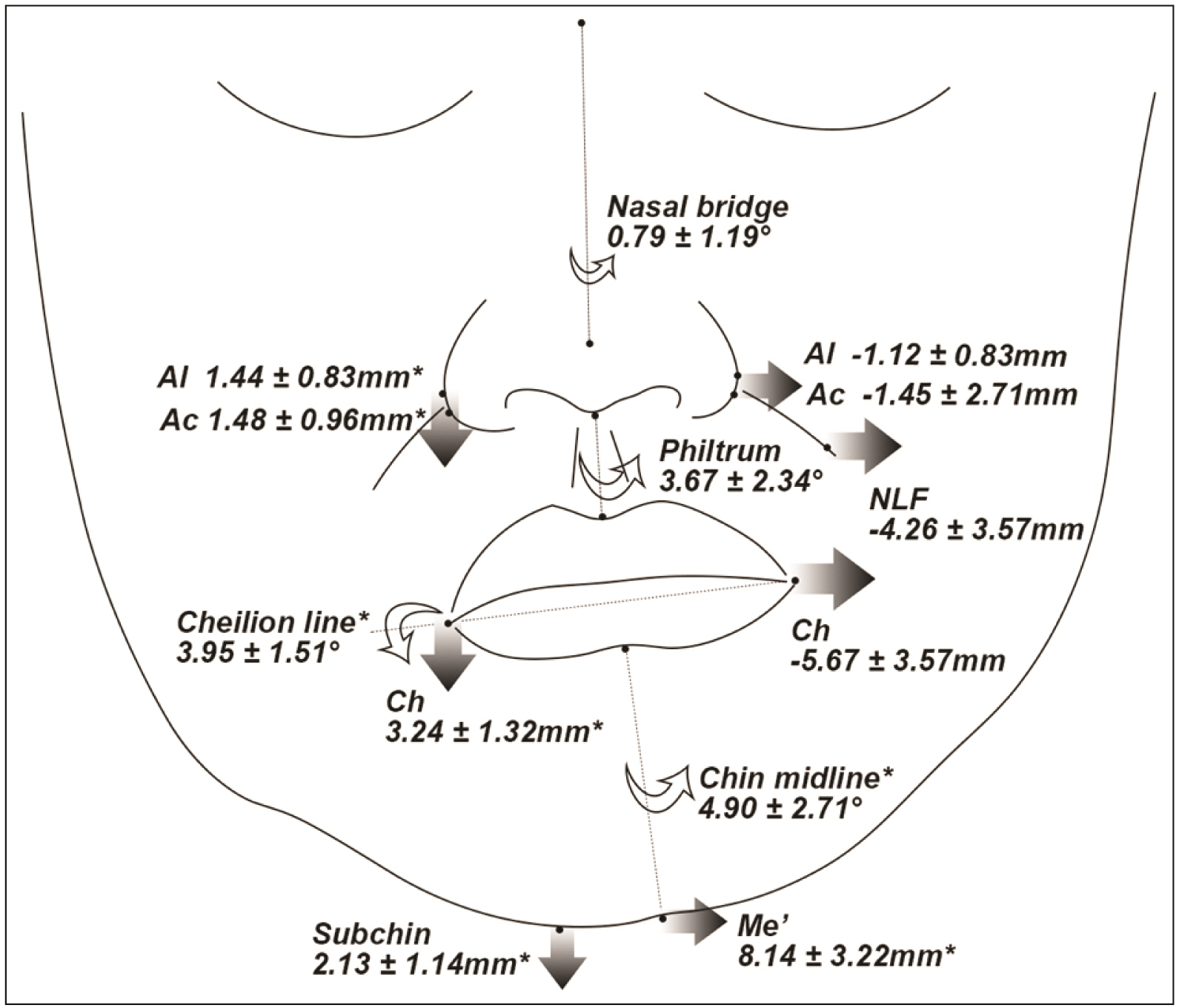
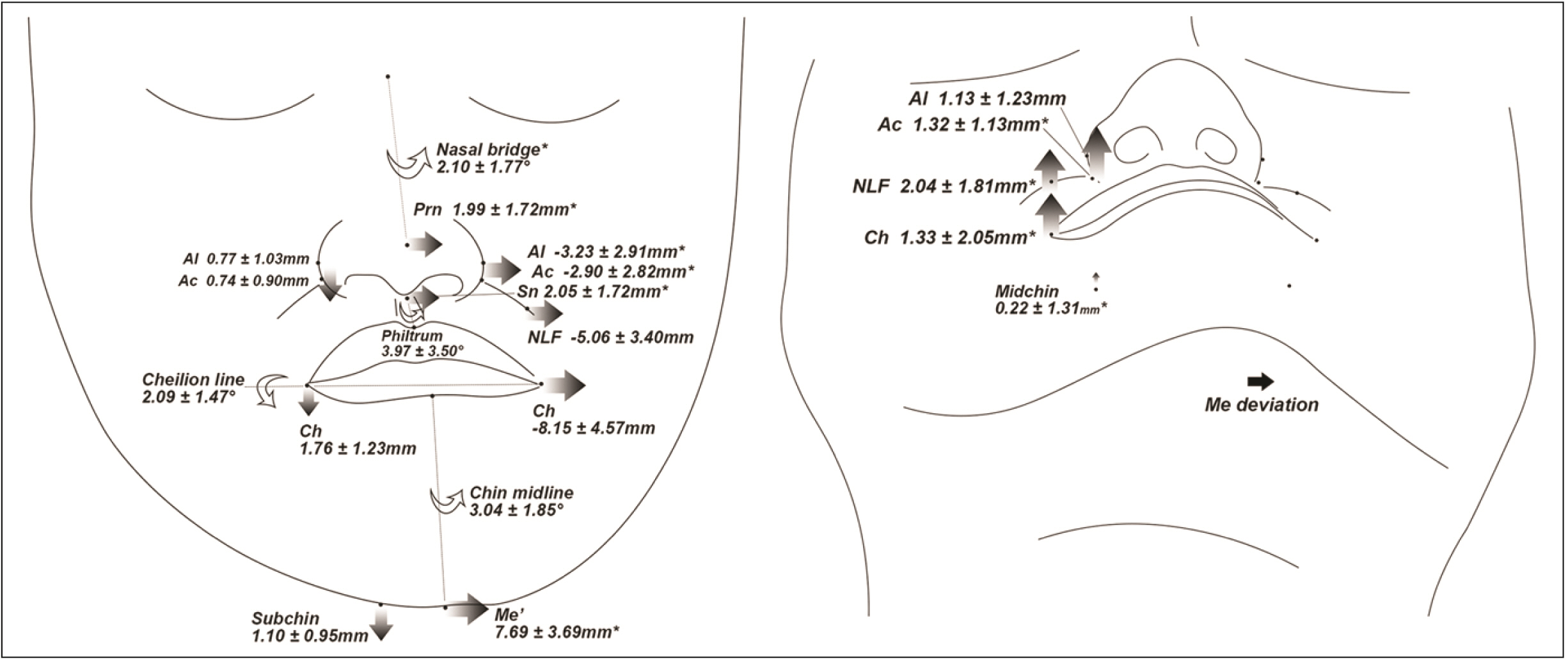
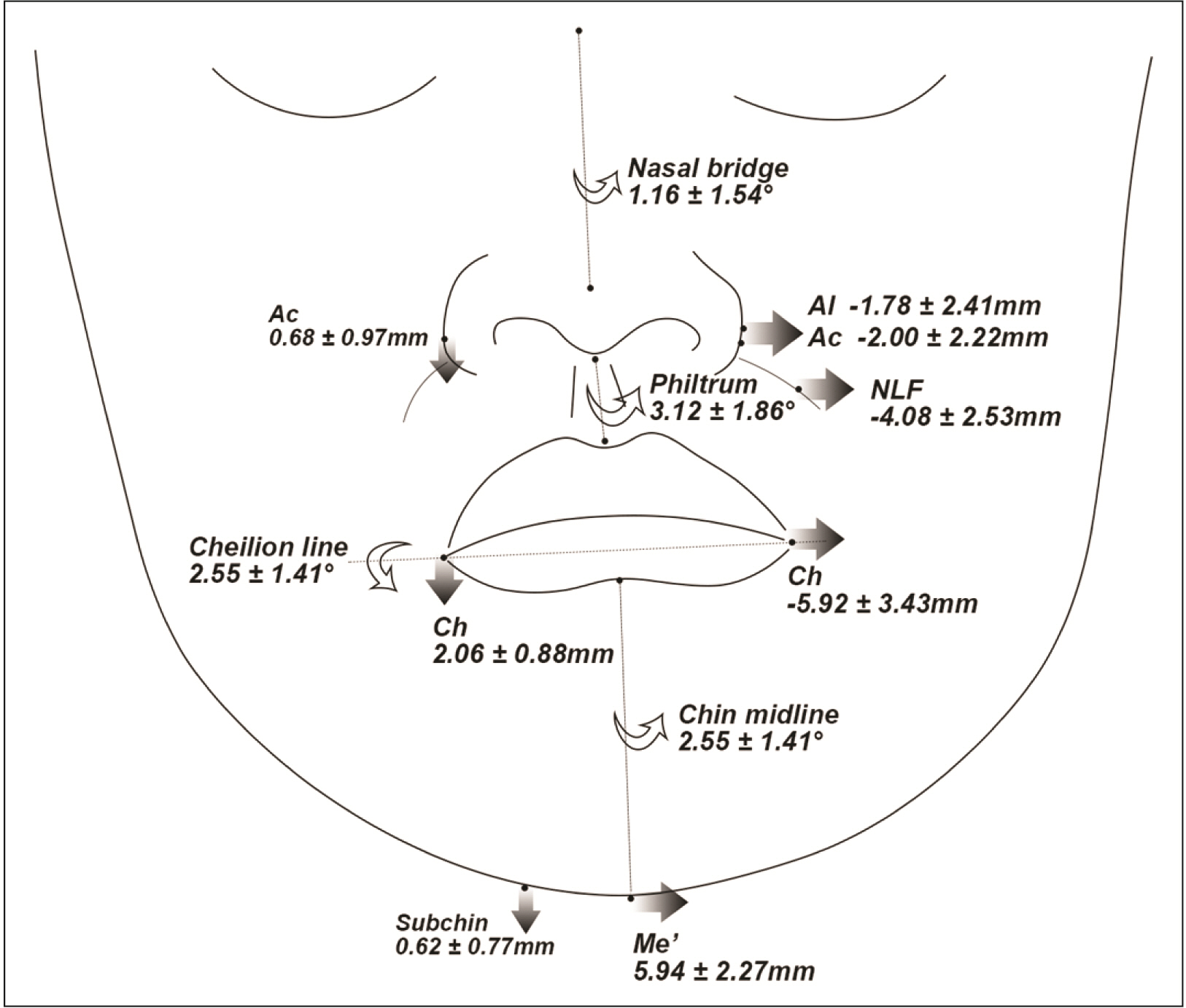
The roll-dominant group showed significantly greater differences in the vertical positions of the soft tissue landmarks between the Dv and NDv than other groups (P < 0.05), whereas the yaw-dominant group exhibited larger differences in the transverse and anteroposterior directions (P < 0.05). Moreover, transverse lip cant was correlated with the menton (Me) deviation and mandibular rolling in the roll-dominant group (P < 0.001); the angulation of the nasal bridge or philtrum was correlated with the Me deviation and mandibular yawing in the yaw-dominant group (P < 0.01).
Conclusions
The threedimensional deviations of facial soft tissue differed based on the mandibular asymmetry types in Class III patients with similar amounts of Me deviation. A precise understanding of soft tissue deviation in each asymmetry type would help achieve satisfactory facial esthetics.
Keyword
Figure
Reference
-
1. Hwang DS, Kim YI, Park SB, Lee JY. 2012; Midfacial soft tissue changes after leveling Le Fort I osteotomy with differential reduction. Cone-beam computed tomography volume superimposition. Angle Orthod. 82:424–31. https://doi.org/10.2319/052411-342.1. DOI: 10.2319/052411-342.1. PMID: 21888537. PMCID: PMC8865816.
Article2. Haraguchi S, Takada K, Yasuda Y. 2002; Facial asymmetry in subjects with skeletal Class III deformity. Angle Orthod. 72:28–35. https://pubmed.ncbi.nlm.nih.gov/11843270/. DOI: 10.1043/0003-3219(2002)072<0028:FAISWS>2.0.CO;2. PMID: 11843270.3. Lee ST, Mori Y, Minami K, An CH, Park JW, Kwon TG. 2013; Does skeletal surgery for asymmetric mandibular prognathism influence the soft tissue contour and thickness? J Oral Maxillofac Surg. 71:1577–87. https://doi.org/10.1016/j.joms.2013.04.008. DOI: 10.1016/j.joms.2013.04.008. PMID: 23800674.
Article4. Nur RB, Çakan DG, Arun T. 2016; Evaluation of facial hard and soft tissue asymmetry using cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 149:225–37. https://doi.org/10.1016/j.ajodo.2015.07.038. DOI: 10.1016/j.ajodo.2015.07.038. PMID: 26827979.
Article5. Yamamoto S, Miyachi H, Fujii H, Ochiai S, Watanabe S, Shimozato K. 2016; Intuitive facial imaging method for evaluation of postoperative swelling: a combination of 3-dimensional computed tomography and laser surface scanning in orthognathic surgery. J Oral Maxillofac Surg. 74:2506.e1–10. https://doi.org/10.1016/j.joms.2016.08.039. DOI: 10.1016/j.joms.2016.08.039. PMID: 27669371.
Article6. Severt TR, Proffit WR. 1997; The prevalence of facial asymmetry in the dentofacial deformities population at the University of North Carolina. Int J Adult Orthodon Orthognath Surg. 12:171–6. https://pubmed.ncbi.nlm.nih.gov/9511487/. DOI: 10.1055/b-0034-71589. PMID: 9511487.7. Thiesen G, Gribel BF, Freitas MPM, Oliver DR, Kim KB. 2018; Mandibular asymmetries and associated factors in orthodontic and orthognathic surgery patients. Angle Orthod. 88:545–51. https://doi.org/10.2319/111517-785.1. DOI: 10.2319/111517-785.1. PMID: 29667467. PMCID: PMC8183131.
Article8. Chew MT. 2006; Spectrum and management of dentofacial deformities in a multiethnic Asian population. Angle Orthod. 76:806–9. https://pubmed.ncbi.nlm.nih.gov/17029514/.9. Kim WS, Lee KH, Hwang HS. 2005; Comparison of asymmetric degree between maxillofacial hard and soft tissue in facial asymmetric subjects using three-dimensional computed tomography. Korean J Orthod. 35:163–73. https://e-kjo.org/journal/view.html?volume=35&number=3&spage=163.10. Hwang HS, Min YS, Lee SC, Sun MK, Lim HS. 2009; Change of lip-line cant after 1-jaw orthognathic surgery in patients with mandibular asymmetry. Am J Orthod Dentofacial Orthop. 136:564–9. https://doi.org/10.1016/j.ajodo.2007.10.060. DOI: 10.1016/j.ajodo.2007.10.060. PMID: 19815160.
Article11. Kim SJ, Choi JY, Baek SH. 2012; Evaluation of canting correction of the maxillary transverse occlusal plane and change of the lip canting in Class III two-jaw orthognathic surgery. Angle Orthod. 82:1092–7. https://doi.org/10.2319/011512-36.1. DOI: 10.2319/011512-36.1. PMID: 22515938. PMCID: PMC8813154.
Article12. Yao F, Lawson W, Westreich RW. 2009; Effect of midfacial asymmetry on nasal axis deviation: indications for use of the subalar graft. Arch Facial Plast Surg. 11:157–64. https://doi.org/10.1001/archfaci.2009.1. DOI: 10.1001/archfaci.2009.1. PMID: 19451449.
Article13. Kim JY, Jung HD, Jung YS, Hwang CJ, Park HS. 2014; A simple classification of facial asymmetry by TML system. J Craniomaxillofac Surg. 42:313–20. https://doi.org/10.1016/j.jcms.2013.05.019. DOI: 10.1016/j.jcms.2013.05.019. PMID: 23810748.
Article14. Tyan S, Park HS, Janchivdorj M, Han SH, Kim SJ, Ahn HW. 2016; Three-dimensional analysis of molar compensation in patients with facial asymmetry and mandibular prognathism. Angle Orthod. 86:421–30. https://doi.org/10.2319/030915-142.1. DOI: 10.2319/030915-142.1. PMID: 26192894. PMCID: PMC8601728.
Article15. Ackerman JL, Proffit WR, Sarver DM, Ackerman MB, Kean MR. 2007; Pitch, roll, and yaw: describing the spatial orientation of dentofacial traits. Am J Orthod Dentofacial Orthop. 131:305–10. https://doi.org/10.1016/j.ajodo.2006.05.032. DOI: 10.1016/j.ajodo.2006.05.032. PMID: 17346584.
Article16. Chen YJ, Yao CC, Chang ZC, Lai HH, Lu SC, Kok SH. 2016; A new classification of mandibular asymmetry and evaluation of surgical-orthodontic treatment outcomes in Class III malocclusion. J Craniomaxillofac Surg. 44:676–83. https://doi.org/10.1016/j.jcms.2016.03.011. DOI: 10.1016/j.jcms.2016.03.011. PMID: 27107473.17. Baek C, Paeng JY, Lee JS, Hong J. 2012; Morphologic evaluation and classification of facial asymmetry using 3-dimensional computed tomography. J Oral Maxillofac Surg. 70:1161–9. https://doi.org/10.1016/j.joms.2011.02.135. DOI: 10.1016/j.joms.2011.02.135. PMID: 21763045.18. Cho JH, Kim EJ, Kim BC, Cho KH, Lee KH, Hwang HS. 2007; Correlations of frontal lip-line canting with craniofacial morphology and muscular activity. Am J Orthod Dentofacial Orthop. 132:278.e7–14. https://doi.org/10.1016/j.ajodo.2007.01.015. DOI: 10.1016/j.ajodo.2007.01.015. PMID: 17826591.
Article19. Suzuki-Okamura E, Higashihori N, Kawamoto T, Moriyama K. 2015; Three-dimensional analysis of hard and soft tissue changes in patients with facial asymmetry undergoing 2-jaw surgery. Oral Surg Oral Med Oral Pathol Oral Radiol. 120:299–306. https://doi.org/10.1016/j.oooo.2015.05.020. DOI: 10.1016/j.oooo.2015.05.020. PMID: 26297389.
Article20. Lo LJ, Weng JL, Ho CT, Lin HH. 2018; Three-dimensional region-based study on the relationship between soft and hard tissue changes after orthognathic surgery in patients with prognathism. PLoS One. 13:e0200589. https://doi.org/10.1371/journal.pone.0200589. DOI: 10.1371/journal.pone.0200589. PMID: 30067766. PMCID: PMC6070212. PMID: 9081652a3e154b0fa4fd381bced25e4d.
Article21. Kim HJ, Noh HK, Park HS. 2023; Use of a novel body mandibular plane (mental foramen-protuberance menti) in analyzing mandibular asymmetry compared with conventional border mandibular plane. Angle Orthod. 93:195–204. https://doi.org/10.2319/072522-513.1. DOI: 10.2319/072522-513.1. PMID: 36689739. PMCID: PMC9933560.
Article22. Kim HJ, Noh HK, Park HS. 2023; Mandibular asymmetry types and differences in dental compensations of Class III patients analyzed with cone-beam computed tomography. Angle Orthod. [Epub ahead of print] https://doi.org/10.2319/013023-73.1. DOI: 10.2319/013023-73.1. PMID: 37407513. PMCID: PMC10633797.
Article23. Baek ES, Hwang S, Choi YJ, Roh MR, Nguyen T, Kim KH, et al. 2018; Quantitative and perceived visual changes of the nasolabial fold following orthodontic retraction of lip protrusion. Angle Orthod. 88:465–73. https://doi.org/10.2319/100317-665.1. DOI: 10.2319/100317-665.1. PMID: 29561659. PMCID: PMC8191930.
Article24. Shah SM, Joshi MR. 1978; An assessment of asymmetry in the normal craniofacial complex. Angle Orthod. 48:141–8. https://pubmed.ncbi.nlm.nih.gov/277077/. DOI: 10.1043/0003-3219(1978)048<0141:AAOAIT>2.0.CO;2. PMID: 277077.25. Kim YH, Jeon J, Rhee JT, Hong J. 2010; Change of lip cant after bimaxillary orthognathic surgery. J Oral Maxillofac Surg. 68:1106–11. https://doi.org/10.1016/j.joms.2009.07.030. DOI: 10.1016/j.joms.2009.07.030. PMID: 20202735.
Article26. Kim CH, Lee JH, Cho JY, Lee JH, Kim KW. 2007; Skeletal stability after simultaneous mandibular angle resection and sagittal split ramus osteotomy for correction of mandible prognathism. J Oral Maxillofac Surg. 65:192–7. https://doi.org/10.1016/j.joms.2005.12.064. DOI: 10.1016/j.joms.2005.12.064. PMID: 17236920.
Article27. Xiao Y, Sun X, Wang L, Zhang Y, Chen K, Wu G. 2017; The application of 3D printing technology for simultaneous orthognathic surgery and mandibular contour osteoplasty in the treatment of craniofacial deformities. Aesthetic Plast Surg. 41:1413–24. https://doi.org/10.1007/s00266-017-0914-z. DOI: 10.1007/s00266-017-0914-z. PMID: 28639069.
Article28. Kim YM, Rha KS, Weissman JD, Hwang PH, Most SP. 2011; Correlation of asymmetric facial growth with deviated nasal septum. Laryngoscope. 121:1144–8. https://doi.org/10.1002/lary.21785. DOI: 10.1002/lary.21785. PMID: 21495046.
Article29. D'Ascanio L, Lancione C, Pompa G, Rebuffini E, Mansi N, Manzini M. 2010; Craniofacial growth in children with nasal septum deviation: a cephalometric comparative study. Int J Pediatr Otorhinolaryngol. 74:1180–3. https://doi.org/10.1016/j.ijporl.2010.07.010. DOI: 10.1016/j.ijporl.2010.07.010. PMID: 20696485.30. Meyer-Marcotty P, Stellzig-Eisenhauer A, Bareis U, Hartmann J, Kochel J. 2011; Three-dimensional perception of facial asymmetry. Eur J Orthod. 33:647–53. https://doi.org/10.1093/ejo/cjq146. DOI: 10.1093/ejo/cjq146. PMID: 21355063.
Article31. Shin YM, Lee ST, Nam KY, Kwon TG. 2017; Nasal deviation in patients with asymmetric mandibular prognathism. J Craniofac Surg. 28:e700–4. https://doi.org/10.1097/SCS.0000000000003894. DOI: 10.1097/SCS.0000000000003894. PMID: 28891902.
Article32. Waite PD, Matukas VJ. 1991; Indications for simultaneous orthognathic and septorhinoplastic surgery. J Oral Maxillofac Surg. 49:133–40. https://doi.org/10.1016/0278-2391(91)90099-8. DOI: 10.1016/0278-2391(91)90099-8. PMID: 1990090.
Article33. Raffaini M, Cocconi R, Spinelli G, Agostini T. 2018; Simultaneous rhinoseptoplasty and orthognathic surgery: outcome analysis of 250 consecutive patients using a modified Le Fort I osteotomy. Aesthetic Plast Surg. 42:1090–100. https://doi.org/10.1007/s00266-018-1121-2. DOI: 10.1007/s00266-018-1121-2. PMID: 29560545.
Article34. Kwon TG, Kang SM, Hwang HD. 2014; Three-dimensional soft tissue change after paranasal augmentation with porous polyethylene. Int J Oral Maxillofac Surg. 43:816–23. https://doi.org/10.1016/j.ijom.2014.03.004. DOI: 10.1016/j.ijom.2014.03.004. PMID: 24685262.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Differences in positions of cone-beam computed tomography landmarks in patients with skeletal Class III facial asymmetry according to midsagittal planes
- Cone-beam computed tomography analysis of transverse dental compensation in patients with skeletal Class III malocclusion and facial asymmetry
- Location and shape of the mandibular lingula: Comparison of skeletal class I and class III patients using panoramic radiography and cone-beam computed tomography
- Cone-beam computed tomography based evaluation of rotational patterns of dentofacial structures in skeletal Class III deformity with mandibular asymmetry
- Evaluation of facial soft tissue thickness in asymmetric mandibular deformities after orthognathic surgery