J Korean Med Sci.
2023 May;38(21):e161. 10.3346/jkms.2023.38.e161.
Efficacy of Acetylcysteine and Selenium in Aneurysmal Subarachnoid Hemorrhage Patients: A Prospective, Multicenter, Single Blind Randomized Controlled Trial
- Affiliations
-
- 1Department of Neurosurgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Department of Medical Science, Asan Medical Institute of Convergence Science and Technology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 3Department of Neurosurgery, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
- 4Department of Neurosurgery, Seoul National University Bundang Hospital, Seongnam, Korea
- KMID: 2542598
- DOI: http://doi.org/10.3346/jkms.2023.38.e161
Abstract
- Background
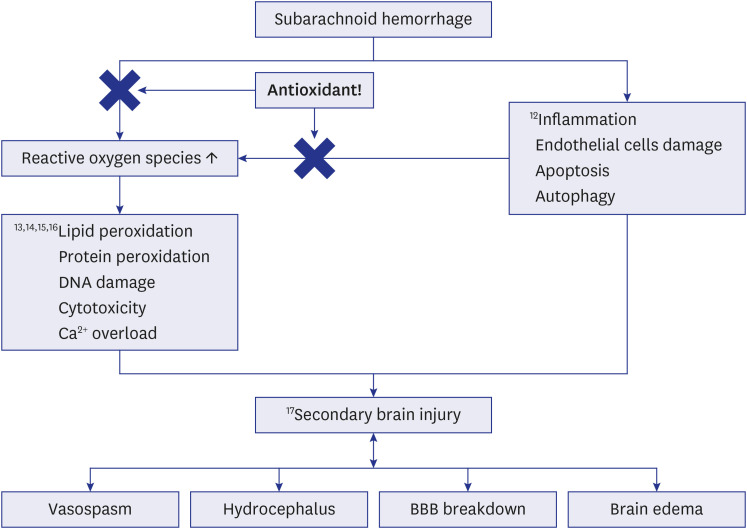
Subarachnoid hemorrhage (SAH) patients have oxidative stress results in inflammation, tissue degeneration and neuronal damage. These deleterious effects cause aggravation of the perihematomal edema (PHE), vasospasm, and even hydrocephalus. We hypothesized that antioxidants may have a neuroprotective role in acute aneurysmal SAH (aSAH) patients.
Methods
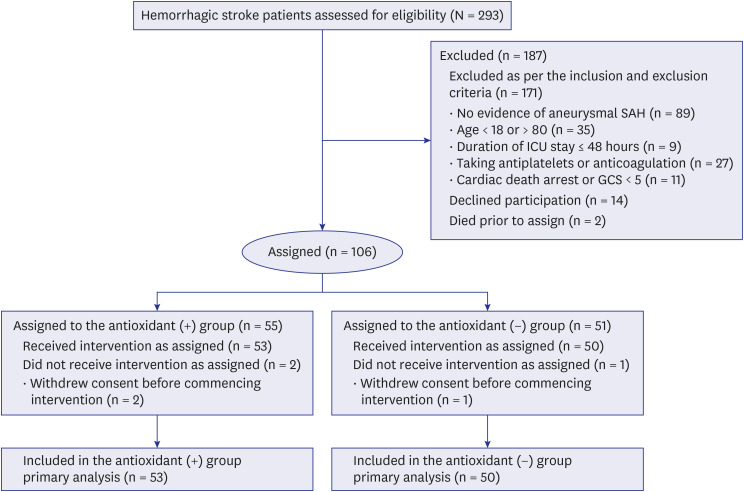
We conducted a prospective, multicenter randomized (single blind) trial between January 2017 and October 2019, investigating whether antioxidants (acetylcysteine and selenium) have the potential to improve the neurologic outcome in aSAH patients. The antioxidant patient group received antioxidants of acetylcysteine (2,000 mg/day) and selenium (1,600 µg/day) intravenously (IV) for 14 days. These drugs were administrated within 24 hours of admission. The non-antioxidant patient group received a placebo IV.
Results
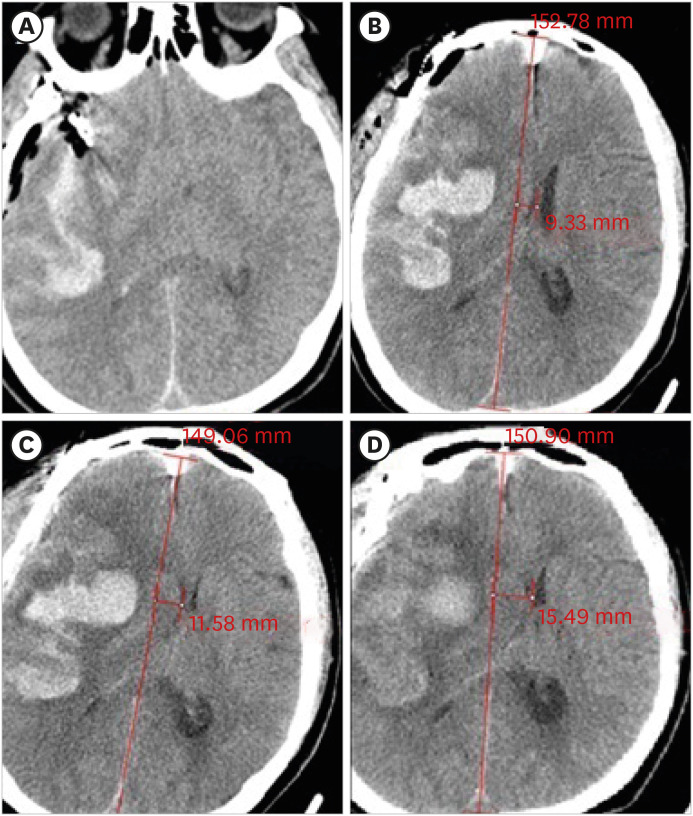
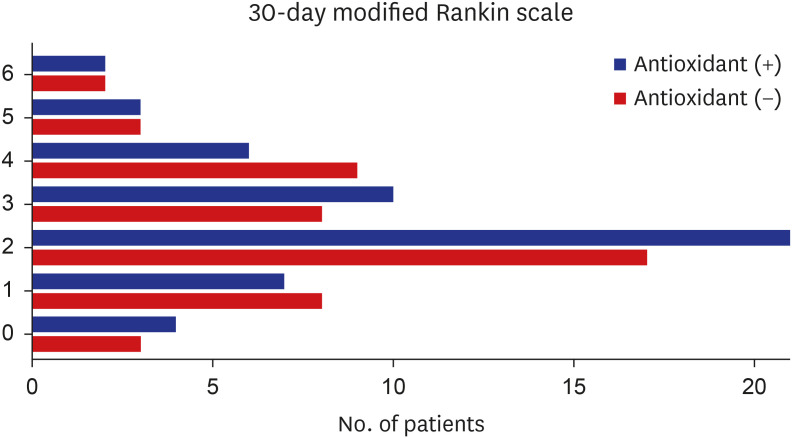
In total, 293 patients were enrolled with 103 patients remaining after applying the inclusion and exclusion criteria. No significant differences were observed in the baseline characteristics between the antioxidant (n = 53) and non-antioxidant (n = 50) groups. Among clinical factors, the duration of intensive care unit (ICU) stay was significantly shortened in patients who received antioxidants (11.2, 95% confidence interval [CI], 9.7–14.5 vs. 8.3, 95% CI, 6.2–10.2 days, P = 0.008). However, no beneficial effects were observed on radiological outcomes.
Conclusion
In conclusion, antioxidant treatment failed to show the reduction of PHE volume, mid-line shifting, vasospasm and hydrocephalus in acute SAH patients. A significant reduction in ICU stay was observed but need more optimal dosing schedule and precise outcome targets are required to clarify the clinical impacts of antioxidants in these patients.
Keyword
Figure
Reference
-
1. Maher M, Schweizer TA, Macdonald RL. Treatment of spontaneous subarachnoid hemorrhage: guidelines and gaps. Stroke. 2020; 51(4):1326–1332. PMID: 31964292.2. Etminan N, Chang HS, Hackenberg K, de Rooij NK, Vergouwen MD, Rinkel GJ, et al. Worldwide incidence of aneurysmal subarachnoid hemorrhage according to region, time period, blood pressure, and smoking prevalence in the population: a systematic review and meta-analysis. JAMA Neurol. 2019; 76(5):588–597. PMID: 30659573.3. Hijdra A, Braakman R, van Gijn J, Vermeulen M, van Crevel H. Aneurysmal subarachnoid hemorrhage. Complications and outcome in a hospital population. Stroke. 1987; 18(6):1061–1067. PMID: 3686578.4. Wardlaw JM, White PM. The detection and management of unruptured intracranial aneurysms. Brain. 2000; 123(Pt 2):205–221. PMID: 10648430.5. Kreiter KT, Copeland D, Bernardini GL, Bates JE, Peery S, Claassen J, et al. Predictors of cognitive dysfunction after subarachnoid hemorrhage. Stroke. 2002; 33(1):200–208. PMID: 11779911.6. Šćepanović V, Tasić G, Repac N, Nikolić I, Janićijević A, Todorović D, et al. The role of oxidative stress as a risk factor for rupture of posterior inferior cerebellar artery aneurysms. Mol Biol Rep. 2018; 45(6):2157–2165. PMID: 30238410.7. Starke RM, Chalouhi N, Ali MS, Jabbour PM, Tjoumakaris SI, Gonzalez LF, et al. The role of oxidative stress in cerebral aneurysm formation and rupture. Curr Neurovasc Res. 2013; 10(3):247–255. PMID: 23713738.8. Gebel JM Jr, Jauch EC, Brott TG, Khoury J, Sauerbeck L, Salisbury S, et al. Natural history of perihematomal edema in patients with hyperacute spontaneous intracerebral hemorrhage. Stroke. 2002; 33(11):2631–2635. PMID: 12411653.9. Xi G, Wagner KR, Keep RF, Hua Y, de Courten-Myers GM, Broderick JP, et al. Role of blood clot formation on early edema development after experimental intracerebral hemorrhage. Stroke. 1998; 29(12):2580–2586. PMID: 9836771.10. Chen S, Luo J, Reis C, Manaenko A, Zhang J. Hydrocephalus after subarachnoid hemorrhage: pathophysiology, diagnosis, and treatment. BioMed Res Int. 2017; 2017:8584753. PMID: 28373987.11. Saito I, Asano T, Sano K, Takakura K, Abe H, Yoshimoto T, et al. Neuroprotective effect of an antioxidant, ebselen, in patients with delayed neurological deficits after aneurysmal subarachnoid hemorrhage. Neurosurgery. 1998; 42(2):269–277. PMID: 9482177.12. Toda N, Ayajiki K, Okamura T. Cerebral blood flow regulation by nitric oxide: recent advances. Pharmacol Rev. 2009; 61(1):62–97. PMID: 19293146.13. Eigel BN, Gursahani H, Hadley RW. ROS are required for rapid reactivation of Na+/Ca2+ exchanger in hypoxic reoxygenated guinea pig ventricular myocytes. Am J Physiol Heart Circ Physiol. 2004; 286(3):H955–H963. PMID: 14592940.14. Li Q, Pogwizd SM, Prabhu SD, Zhou L. Inhibiting Na+/K+ ATPase can impair mitochondrial energetics and induce abnormal Ca2+ cycling and automaticity in guinea pig cardiomyocytes. PLoS One. 2014; 9(4):e93928. PMID: 24722410.15. Chrissobolis S, Miller AA, Drummond GR, Kemp-Harper BK, Sobey CG. Oxidative stress and endothelial dysfunction in cerebrovascular disease. Front Biosci (Landmark Ed). 2011; 16(5):1733–1745. PMID: 21196259.16. Gu Y, Dee CM, Shen J. Interaction of free radicals, matrix metalloproteinases and caveolin-1 impacts blood-brain barrier permeability. Front Biosci (Schol Ed). 2011; 3(4):1216–1231. PMID: 21622267.17. Qu J, Chen W, Hu R, Feng H. The injury and therapy of reactive oxygen species in intracerebral hemorrhage looking at mitochondria. Oxid Med Cell Longev. 2016; 2016:2592935. PMID: 27293511.18. Kocaogullar Y, Ilik K, Esen H, Koc O, Guney O. Preventive effects of intraperitoneal selenium on cerebral vasospasm in experimental subarachnoid hemorrhage. J Neurosurg Anesthesiol. 2010; 22(1):53–58. PMID: 19779374.19. Asano T, Takakura K, Sano K, Kikuchi H, Nagai H, Saito I, et al. Effects of a hydroxyl radical scavenger on delayed ischemic neurological deficits following aneurysmal subarachnoid hemorrhage: results of a multicenter, placebo-controlled double-blind trial. J Neurosurg. 1996; 84(5):792–803. PMID: 8622153.20. Brealey D, Brand M, Hargreaves I, Heales S, Land J, Smolenski R, et al. Association between mitochondrial dysfunction and severity and outcome of septic shock. Lancet. 2002; 360(9328):219–223. PMID: 12133657.21. Heyland D, Muscedere J, Wischmeyer PE, Cook D, Jones G, Albert M, et al. A randomized trial of glutamine and antioxidants in critically ill patients. N Engl J Med. 2013; 368(16):1489–1497. PMID: 23594003.22. Koekkoek WA, van Zanten AR. Antioxidant vitamins and trace elements in critical illness. Nutr Clin Pract. 2016; 31(4):457–474. PMID: 27312081.23. Bulger EM, Maier RV. Antioxidants in critical illness. Arch Surg. 2001; 136(10):1201–1207. PMID: 11585516.24. Munakata A, Ohkuma H, Nakano T, Shimamura N, Asano K, Naraoka M. Effect of a free radical scavenger, edaravone, in the treatment of patients with aneurysmal subarachnoid hemorrhage. Neurosurgery. 2009; 64(3):423–428.25. Zhang S, Wang L, Liu M, Wu B. Tirilazad for aneurysmal subarachnoid haemorrhage. Cochrane Database Syst Rev. 2010; (2):CD006778. PMID: 20166088.26. Jang YG, Ilodigwe D, Macdonald RL. Metaanalysis of tirilazad mesylate in patients with aneurysmal subarachnoid hemorrhage. Neurocrit Care. 2009; 10(1):141–147. PMID: 18810661.27. Broderick JP, Adeoye O, Elm J. Evolution of the modified Rankin scale and its use in future stroke trials. Stroke. 2017; 48(7):2007–2012. PMID: 28626052.28. Hunt WE, Hess RM. Surgical risk as related to time of intervention in the repair of intracranial aneurysms. J Neurosurg. 1968; 28(1):14–20. PMID: 5635959.29. Frontera JA, Claassen J, Schmidt JM, Wartenberg KE, Temes R, Connolly ES Jr, et al. Prediction of symptomatic vasospasm after subarachnoid hemorrhage: the modified fisher scale. Neurosurgery. 2006; 59(1):21–27. PMID: 16823296.30. Rass V, Helbok R. How to diagnose delayed cerebral ischaemia and symptomatic vasospasm and prevent cerebral infarction in patients with subarachnoid haemorrhage. Curr Opin Crit Care. 2021; 27(2):103–114. PMID: 33405414.31. Connolly ES Jr, Rabinstein AA, Carhuapoma JR, Derdeyn CP, Dion J, Higashida RT, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2012; 43(6):1711–1737. PMID: 22556195.32. Frontera JA, Fernandez A, Schmidt JM, Claassen J, Wartenberg KE, Badjatia N, et al. Defining vasospasm after subarachnoid hemorrhage: what is the most clinically relevant definition? Stroke. 2009; 40(6):1963–1968. PMID: 19359629.33. Ragland J, Lee K. Critical care management and monitoring of intracranial pressure. J Neurocrit Care. 2016; 9(2):105–112.34. Manzanares W, Dhaliwal R, Jiang X, Murch L, Heyland DK. Antioxidant micronutrients in the critically ill: a systematic review and meta-analysis. Crit Care. 2012; 16(2):R66. PMID: 22534505.35. Kanamaru K, Weir BK, Simpson I, Witbeck T, Grace M. Effect of 21-aminosteroid U-74006F on lipid peroxidation in subarachnoid clot. J Neurosurg. 1991; 74(3):454–459. PMID: 1993911.36. Erşahin M, Toklu HZ, Cetinel S, Yüksel M, Erzik C, Berkman MZ, et al. Alpha lipoic acid alleviates oxidative stress and preserves blood brain permeability in rats with subarachnoid hemorrhage. Neurochem Res. 2010; 35(3):418–428. PMID: 19823933.37. Hall ED, Andrus PK, Althaus JS, VonVoigtlander PF. Hydroxyl radical production and lipid peroxidation parallels selective post-ischemic vulnerability in gerbil brain. J Neurosci Res. 1993; 34(1):107–112. PMID: 8380874.38. Cui JB, Chen QQ, Liu TT, Li SJ. Risk factors for early-onset ventilator-associated pneumonia in aneurysmal subarachnoid hemorrhage patients. Braz J Med Biol Res. 2018; 51(7):e6830. PMID: 29791584.39. Hanafy KA, Selim MH. Antioxidant strategies in neurocritical care. Neurotherapeutics. 2012; 9(1):44–55. PMID: 22135010.40. Shang H, Cui D, Yang D, Liang S, Zhang W, Zhao W. The radical scavenger edaravone improves neurologic function and perihematomal glucose metabolism after acute intracerebral hemorrhage. J Stroke Cerebrovasc Dis. 2015; 24(1):215–222. PMID: 25440340.41. Manaenko A, Lekic T, Ma Q, Zhang JH, Tang J. Hydrogen inhalation ameliorated mast cell-mediated brain injury after intracerebral hemorrhage in mice. Crit Care Med. 2013; 41(5):1266–1275. PMID: 23388512.42. Angstwurm MW, Engelmann L, Zimmermann T, Lehmann C, Spes CH, Abel P, et al. Selenium in Intensive Care (SIC): results of a prospective randomized, placebo-controlled, multiple-center study in patients with severe systemic inflammatory response syndrome, sepsis, and septic shock. Crit Care Med. 2007; 35(1):118–126. PMID: 17095947.43. Heyland DK, Dhaliwal R, Suchner U, Berger MM. Antioxidant nutrients: a systematic review of trace elements and vitamins in the critically ill patient. Intensive Care Med. 2005; 31(3):327–337. PMID: 15605227.44. Kirkpatrick PJ, Turner CL, Smith C, Hutchinson PJ, Murray GD. STASH Collaborators. Simvastatin in aneurysmal subarachnoid haemorrhage (STASH): a multicentre randomised phase 3 trial. Lancet Neurol. 2014; 13(7):666–675. PMID: 24837690.45. Haley EC Jr, Kassell NF, Apperson-Hansen C, Maile MH, Alves WM. A randomized, double-blind, vehicle-controlled trial of tirilazad mesylate in patients with aneurysmal subarachnoid hemorrhage: a cooperative study in North America. J Neurosurg. 1997; 86(3):467–474. PMID: 9046304.46. Cherubini A, Polidori MC, Bregnocchi M, Pezzuto S, Cecchetti R, Ingegni T, et al. Antioxidant profile and early outcome in stroke patients. Stroke. 2000; 31(10):2295–2300. PMID: 11022053.47. Angstwurm MW, Schottdorf J, Schopohl J, Gaertner R. Selenium replacement in patients with severe systemic inflammatory response syndrome improves clinical outcome. Crit Care Med. 1999; 27(9):1807–1813. PMID: 10507602.48. Huang TS, Shyu YC, Chen HY, Lin LM, Lo CY, Yuan SS, et al. Effect of parenteral selenium supplementation in critically ill patients: a systematic review and meta-analysis. PLoS One. 2013; 8(1):e54431. PMID: 23372722.49. Manzanares W, Langlois PL, Heyland DK. Pharmaconutrition with selenium in critically ill patients: what do we know? Nutr Clin Pract. 2015; 30(1):34–43. PMID: 25524883.50. Carter RF. Acute selenium poisoning. Med J Aust. 1966; 1(13):525–528. PMID: 5908595.51. Kelly FJ. Vitamin E supplementation in the critically ill patient: too narrow a view? Nutr Clin Pract. 1994; 9(4):141–145. PMID: 8078452.52. Andrews PJ, Avenell A, Noble DW, Campbell MK, Croal BL, Simpson WG, et al. Randomised trial of glutamine, selenium, or both, to supplement parenteral nutrition for critically ill patients. BMJ. 2011; 342:d1542. PMID: 21415104.53. Berger MM, Soguel L, Shenkin A, Revelly JP, Pinget C, Baines M, et al. Influence of early antioxidant supplements on clinical evolution and organ function in critically ill cardiac surgery, major trauma, and subarachnoid hemorrhage patients. Crit Care. 2008; 12(4):R101. PMID: 18687132.54. Zhang T, Wu P, Zhang JH, Li Y, Xu S, Wang C, et al. Docosahexaenoic acid alleviates oxidative stress-based apoptosis via improving mitochondrial dynamics in early brain injury after subarachnoid hemorrhage. Cell Mol Neurobiol. 2018; 38(7):1413–1423. PMID: 30084007.55. Xie YK, Zhou X, Yuan HT, Qiu J, Xin DQ, Chu XL, et al. Resveratrol reduces brain injury after subarachnoid hemorrhage by inhibiting oxidative stress and endoplasmic reticulum stress. Neural Regen Res. 2019; 14(10):1734–1742. PMID: 31169191.56. Han Y, Su J, Liu X, Zhao Y, Wang C, Li X. Naringin alleviates early brain injury after experimental subarachnoid hemorrhage by reducing oxidative stress and inhibiting apoptosis. Brain Res Bull. 2017; 133:42–50. PMID: 28011192.57. Hall ED, Wang JA, Miller DM, Cebak JE, Hill RL. Newer pharmacological approaches for antioxidant neuroprotection in traumatic brain injury. Neuropharmacology. 2019; 145(Pt B):247–258. PMID: 30086292.58. Manzanares W, Lemieux M, Elke G, Langlois PL, Bloos F, Heyland DK. High-dose intravenous selenium does not improve clinical outcomes in the critically ill: a systematic review and meta-analysis. Crit Care. 2016; 20(1):356. PMID: 27788688.59. Park GJ, Ro YS, Yoon H, Lee SG, Jung E, Moon SB, et al. Serum vitamin E level and functional prognosis after traumatic brain injury with intracranial injury: a multicenter prospective study. Front Neurol. 2022; 13:1008717. PMID: 36341128.60. Jeong HG, Cha BG, Kang DW, Kim DY, Ki SK, Kim SI, et al. Ceria nanoparticles synthesized with aminocaproic acid for the treatment of subarachnoid hemorrhage. Stroke. 2018; 49(12):3030–3038. PMID: 30571409.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Trial of a Calcium Channel Blocker in Patients with Aneurysmal Subarachnoid Hemorrhage
- Computerized Tomography Findings Suggesting Non-aneurysmal Spontaneous Subarachnoid Hemorrhage
- Frequency of Aneurysmal Subarachnoid Hemorrhage in Perimesencephalic Subarachnoid Hemorrhage and Need of 4-vessel Angiography
- Hemodynamics of Poor-grade Subarachnoid Hemorrhage
- Clinical Trial of Nimodipine in Patients with Aneurysmal Subarachnoid Hemorrhage