J Cerebrovasc Endovasc Neurosurg.
2023 Mar;25(1):87-92. 10.7461/jcen.2022.E2022.07.001.
Pseudoaneurysm formation or dural arteriovenous fistula formation at the middle meningeal artery following revascularization surgery in Moyamoya disease
- Affiliations
-
- 1Department of Neurosurgery, Asan Medical Center, University of Ulsan, College of Medicine, Seoul, Korea
- KMID: 2540812
- DOI: http://doi.org/10.7461/jcen.2022.E2022.07.001
Abstract
- Moyamoya disease (MMD) is a rare progressive steno-occlusive cerebrovascular disorder. Currently, revascularization surgery is used as optimal treatment to overcome MMD. However, revascularization for MMD has reported several complications. Also, iatrogenic complications such as pseudoaneurysms formation or dural arteriovenous fistulas (dAVFs) formation—has been identified in rare cases after the surgical intervention for revascularizations.
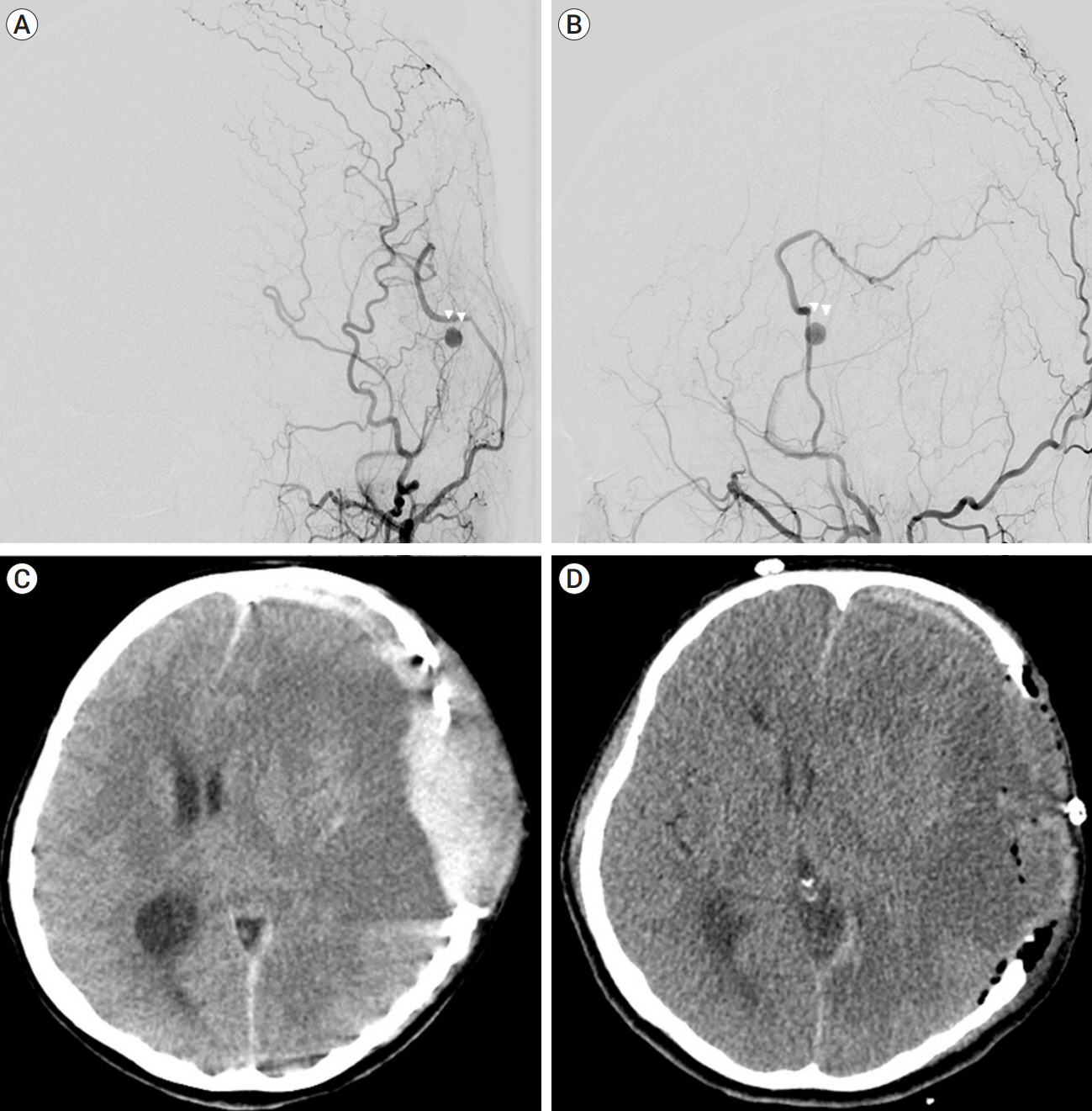
We describe two cases. In first case, the patency of the anastomosis site was good and saccular type pseudoaneurysm formation was found at parietal branch of posterior middle meningeal artery (MMA) in transfemoral cerebral angiography (TFCA) performed on the twelfth day after surgery. We decided to treat pseudoaneurysm by endovascular embolization the next day, but the patient was shown unconsciousness and anisocoria during sleep at that day. Computed tomography showed massive subdural hemorrhage at the ipsilateral side, thus we performed decompressive craniectomy and hematoma evacuation.
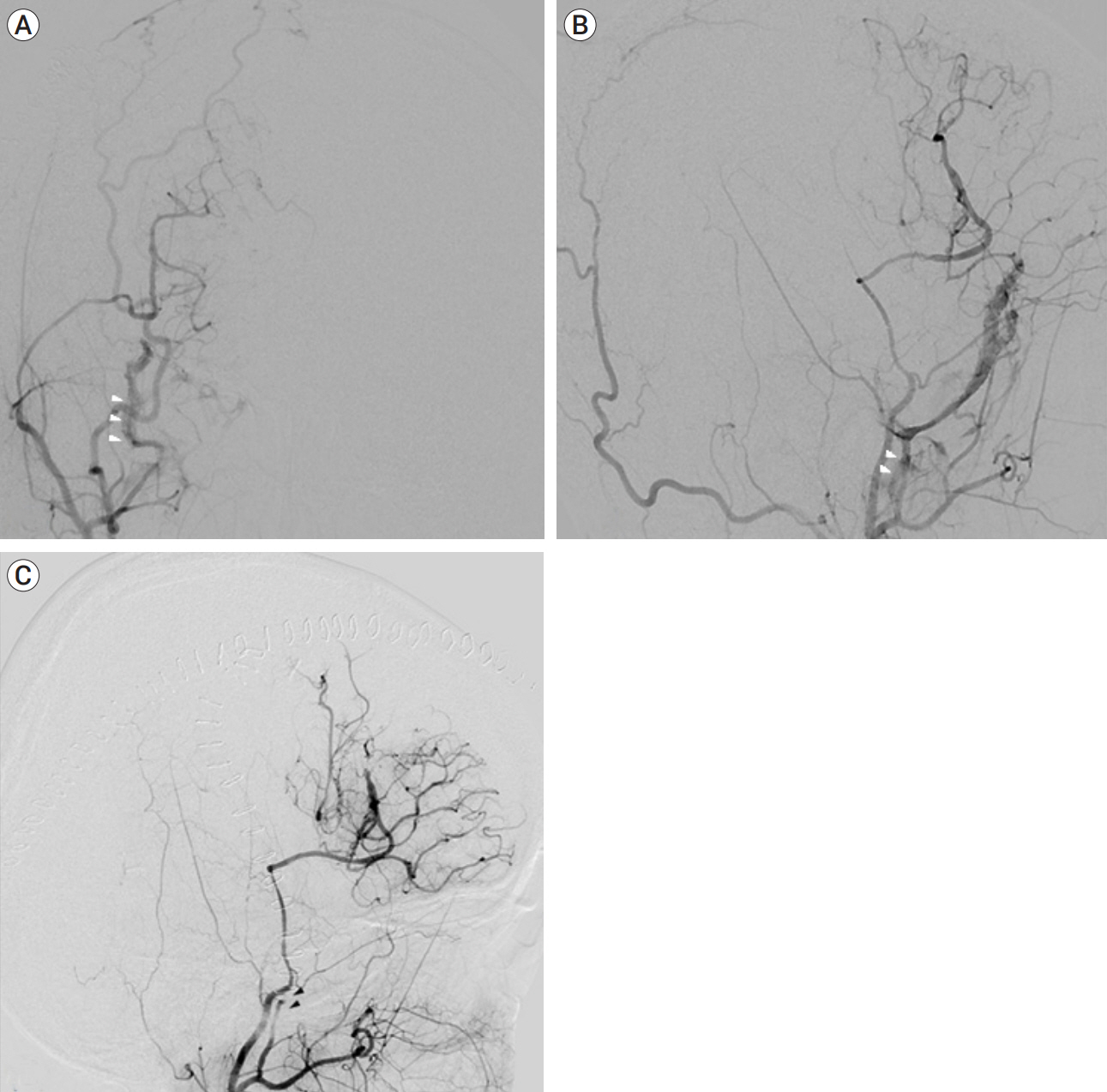
In second case, the patency of the anastomosis site was good and dAVF formation at right MMA was found in TFCA performed on the sixth day after surgery. We performed endovascular obliteration of the arteriovenous fistula under local anesthesia.
Pseudoaneurysm formation or dAVF formation after revascularization surgery is an exceptional case. If patients have such complications, practioner should carefully screen the patients by implementing digital subtraction angiogram to identify anatomic features; as well as consider immediate treatment in any way, including embolization or other surgery
Figure
Reference
-
1. Chiu D, Shedden P, Bratina P, Grotta JC. Clinical features of Moyamoya disease in the United States. Stroke. 1998; Jul. 29(7):1347–51.2. Cognard C, Gobin YP, Pierot L, Bailly AL, Houdart E, Casasco A, et al. Cerebral dural arteriovenous fistulas: clinical and angiographic correlation with a revised classification of venous drainage. Radiology. 1995; Mar. 194(3):671–80.3. Grandhi R, Zwagerman NT, Lee P, Jovin T, Okonkwo DO. Iatrogenic pseudoaneurysm of the middle meningeal artery after external ventricular drain placement. J Neuroimaging. 2015; Jan-Feb. 25(1):140–1.4. Kim H, Jang DK, Han YM, Sung JH, Park IS, Lee KS, et al. Direct bypass versus indirect bypass in adult Moyamoya angiopathy with symptoms or hemodynamic instability: a meta-analysis of comparative studies. World Neurosurg. 2016; Oct. 94:273–84.5. Komiyama M, Yasui T, Tamura K, Nagata Y, Fu Y, Yagura H. Chronic subdural hematoma associated with middle meningeal arteriovenous fistula treated by a combination of embolization and burr hole drainage. Surg Neurol. 1994; Oct. 42(4):316–9.6. Luciani A, Houdart E, Mounayer C, Saint Maurice JP, Merland JJ. Spontaneous closure of dural arteriovenous fistulas: report of three cases and review of the literature. AJNR Am J Neuroradiol. 2001; May. 22(5):992–6.7. Madhusudan HV, Krishnamoorthy N, Suresh PK, Subramaniam V. Superficial temporal artery pseudoaneurysm presenting as extradural hematoma: a case report and review of literature. Asian J Neurosurg. 2015; Apr-Jun. 10(2):63–5.8. Mesiwala AH, Sviri G, Fatemi N, Britz GW, Newell DW. Long-term outcome of superficial temporal artery-middle cerebral artery bypass for patients with Moyamoya disease in the US. Neurosurg Focus. 2008; 24(2):E15.9. Nabors MW, Azzam CJ, Albanna FJ, Gulya AJ, Davis DO, Kobrine AI. Delayed postoperative dural arteriovenous malformations. Report of two cases. J Neurosurg. 1987; May. 66(5):768–72.10. Pourdanesh F, Salehian M, Dehghan P, Dehghani N, Dehghani S. Pseudoaneurysm of the superficial temporal artery following penetrating trauma. J Craniofac Surg. 2013; Jul. 24(4):e334–7.11. Qian C, Yu X, Li J, Chen J, Wang L, Chen G. The efficacy of surgical treatment for the secondary prevention of stroke in symptomatic Moyamoya disease: a meta-analysis. Medicine (Baltimore). 2015; Dec. 94(49):e2218.12. Sakamoto T, Kawaguchi M, Kurehara K, Kitaguchi K, Furuya H, Karasawa J. Risk factors for neurologic deterioration after revascularization surgery in patients with Moyamoya disease. Anesth Analg. 1997; Nov. 85(5):1060–5.13. Skaf GS, Domloj NT, Salameh JA, Atiyeh B. Pseudoaneurysm of the superficial temporal artery: a complication of botulinum toxin injection. Aesthetic Plast Surg. 2012; Aug. 36(4):982–5.14. Sun H, Wilson C, Ozpinar A, Safavi-Abbasi S, Zhao Y, Nakaji P, et al. Perioperative complications and long-term outcomes after bypasses in adults with Moyamoya disease: a systematic review and meta-analysis. World Neurosurg. 2016; Aug. 92:179–88.15. Vadivelu S, Xin X, Loven T, Restrepo G, Chalif DJ, Setton A. Iatrogenic dural arteriovenous fistula and aneurysmal subarachnoid hemorrhage. Neurosurg Focus. 2012; May. 32(5):E1.16. Yilmaz EY, Pritz MB, Bruno A, Lopez-Yunez A, Biller J. Moyamoya: Indiana University Medical Center experience. Arch Neurol. 2001; Aug. 58(8):1274–8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Iatrogenic Dural Arteriovenous Fistula after Superficial Temporal Artery to Middle Cerebral Artery Anastomosis: A Case Report
- Rupture of a Middle Meningeal Artery Pseudoaneurysm in Moyamoya Syndrome Related with Tuberculous Meningitis
- Traumatic Intracerebral and Subarachnoid Hemorrhage Due to a Ruptured Pseudoaneurysm of Middle Meningeal Artery Accompanied by a Medial Sphenoid Wing Dural Arteriovenous Fistula
- Refractory Spontaneous Chronic Subdural Hematoma: A Rare Presentation of an Intracranial Arteriovenous Fistula
- Transcranial Direct Middle Meningeal Artery Puncture for the Onyx Embolization of Dural Arteriovenous Fistula Involving the Superior Sagittal Sinus