J Stroke.
2023 Jan;25(1):16-25. 10.5853/jos.2022.04077.
Sex and Gender Differences in Stroke and Their Practical Implications in Acute Care
- Affiliations
-
- 1Department of Diagnostic Imaging, Foothills Medical Center, University of Calgary, Calgary, AB, Canada
- 2Department of Clinical Neurosciences, Foothills Medical Center, University of Calgary, Calgary, AB, Canada
- 3Department of Neurology, University of Manitoba, Winnipeg, MB, Canada
- KMID: 2539055
- DOI: http://doi.org/10.5853/jos.2022.04077
Abstract
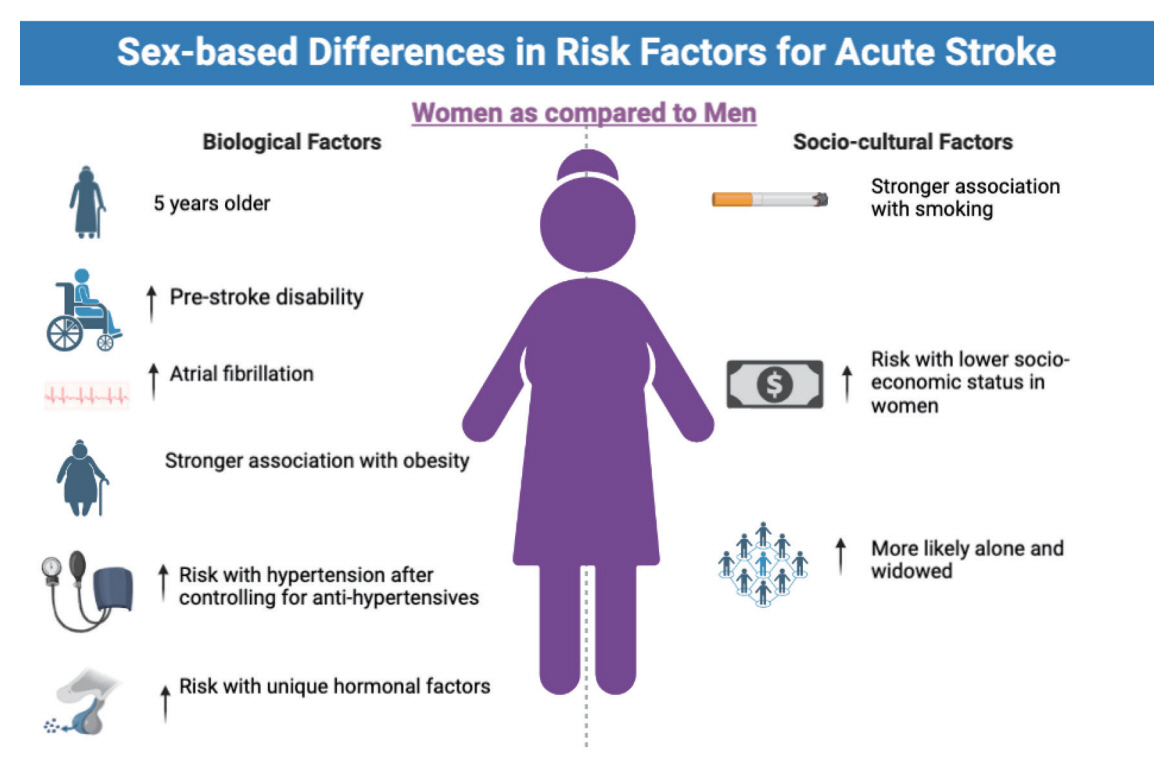
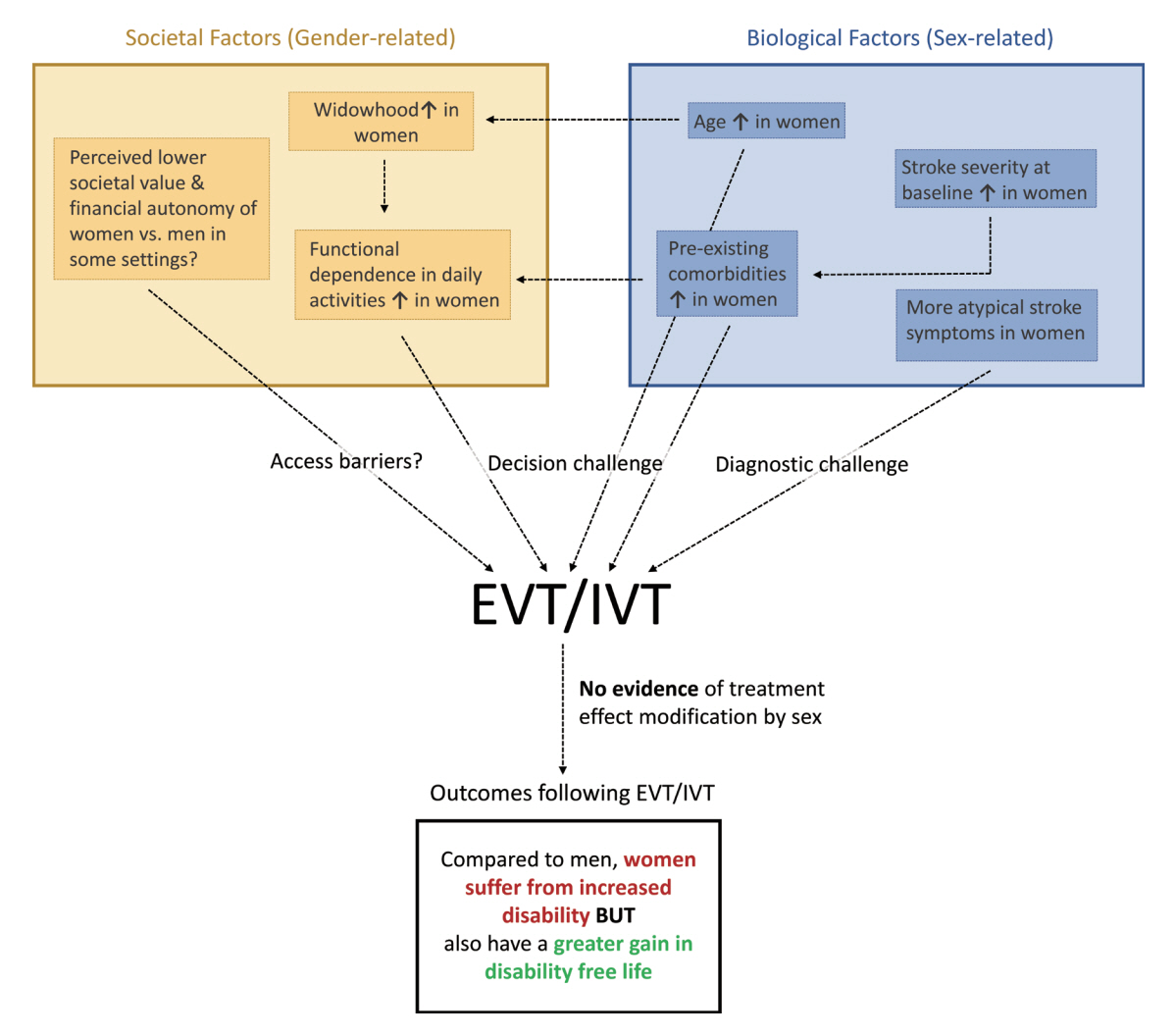
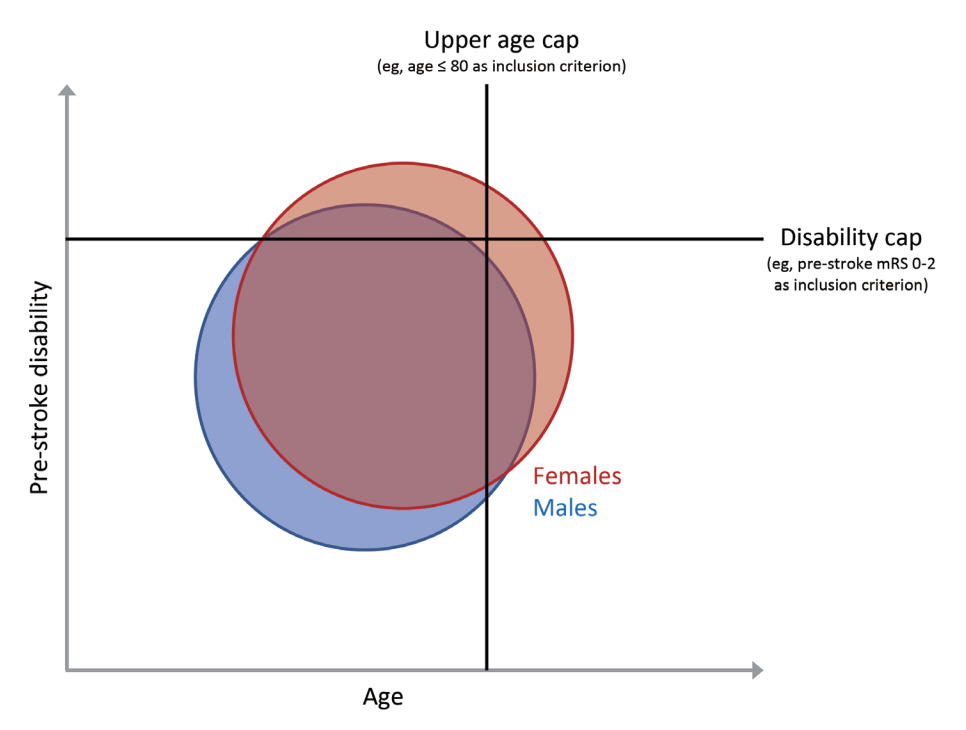
- There are several controversies regarding the role of sex and gender in the pathophysiology and management of acute stroke. Assessing the role of sex, i.e., biological/pathophysiological factors, and gender, i.e., sociocultural factors, in isolation is often not possible since they are closely intertwined with each other. To complicate matters even more, the functional baseline status of women and men at the time of their first stroke is substantially different, whereby women have, on average, a poorer reported/ascertained baseline function compared to men. These differences in baseline variables account for a large part of the differences in post-stroke outcomes between women and men. Adjusting for these baseline differences is difficult, and in many cases, residual confounding cannot be excluded. Despite these obstacles, a better understanding of how patient sex and gender differences influence acute stroke and stroke care pathways is crucial to avoid biases and allow us to provide the best possible care for all acute stroke patients. Disregarding patient sex and gender on one hand and ignoring potential confounding factors in sex- and gender-stratified analyses on the other hand, may cause researchers to come to erroneous conclusions and physicians to provide suboptimal care. This review outlines sex- and gender-related factors in key aspects of acute stroke, including acute stroke epidemiology, diagnosis, access to care, treatment outcomes, and post-acute care. We also attempt to outline knowledge gaps, which deserve to be studied in further detail, and practical implications for physicians treating acute stroke patients in their daily practice.
Keyword
Figure
Reference
-
References
1. Moleiro C, Pinto N. Sexual orientation and gender identity: review of concepts, controversies and their relation to psychopathology classification systems. Front Psychol. 2015; 6:1511.2. Day S, Mason R, Lagosky S, Rochon PA. Integrating and evaluating sex and gender in health research. Health Res Policy Syst. 2016; 14:75.3. Labovitz DL. Stroke epidemiology and intersectionality. Stroke. 2020; 51:2886–2887.4. Ganesh A, Fraser JF, Gordon Perue GL, Amin-Hanjani S, Leslie-Mazwi TM, Greenberg SM, et al. Endovascular treatment and thrombolysis for acute ischemic stroke in patients with premorbid disability or dementia: a scientific statement from the American Heart Association/American Stroke Association. Stroke. 2022; 53:e204–e217.5. Reeves MJ, Bushnell CD, Howard G, Gargano JW, Duncan PW, Lynch G, et al. Sex differences in stroke: epidemiology, clinical presentation, medical care, and outcomes. Lancet Neurol. 2008; 7:915–926.6. Rexrode KM, Madsen TE, Yu AYX, Carcel C, Lichtman JH, Miller EC. The impact of sex and gender on stroke. Circ Res. 2022; 130:512–528.7. Heron M. Deaths: leading causes for 2019. Natl Vital Stat Rep. 2021; 70:1–114.8. Koton S, Sang Y, Schneider ALC, Rosamond WD, Gottesman RF, Coresh J. Trends in stroke incidence rates in older US adults: an update from the Atherosclerosis Risk in Communities (ARIC) cohort study. JAMA Neurol. 2020; 77:109–113.9. Appelros P, Stegmayr B, Terént A. Sex differences in stroke epidemiology: a systematic review. Stroke. 2009; 40:1082–1090.10. Persky RW, Turtzo LC, McCullough LD. Stroke in women: disparities and outcomes. Curr Cardiol Rep. 2010; 12:6–13.11. Mainz J, Andersen G, Valentin JB, Gude MF, Johnsen SP. Disentangling sex differences in use of reperfusion therapy in patients with acute ischemic stroke. Stroke. 2020; 51:2332–2338.12. Madsen TE, DeCroce-Movson E, Hemendinger M, McTaggart RA, Yaghi S, Cutting S, et al. Sex differences in 90-day outcomes after mechanical thrombectomy for acute ischemic stroke. J Neurointerv Surg. 2019; 11:221–225.13. Uchida K, Yoshimura S, Sakai N, Yamagami H, Morimoto T. Sex differences in management and outcomes of acute ischemic stroke with large vessel occlusion. Stroke. 2019; 50:1915–1918.14. Willers C, Lekander I, Ekstrand E, Lilja M, Pessah-Rasmussen H, Sunnerhagen KS, et al. Sex as predictor for achieved health outcomes and received care in ischemic stroke and intracerebral hemorrhage: a register-based study. Biol Sex Differ. 2018; 9:11.15. Niewada M, Kobayashi A, Sandercock PA, Kamin´ski B, Członkowska A; International Stroke Trial Collaborative Group. Influence of gender on baseline features and clinical outcomes among 17,370 patients with confirmed ischaemic stroke in the international stroke trial. Neuroepidemiology. 2005; 24:123–128.16. Roquer J, Campello AR, Gomis M. Sex differences in first-ever acute stroke. Stroke. 2003; 34:1581–1585.17. Renoux C, Coulombe J, Li L, Ganesh A, Silver L, Rothwell PM; Oxford Vascular Study. Confounding by pre-morbid functional status in studies of apparent sex differences in severity and outcome of stroke. Stroke. 2017; 48:2731–2738.18. Reeves MJ, Fonarow GC, Zhao X, Smith EE, Schwamm LH; Get With The Guidelines-Stroke Steering Committee & Investigators. Quality of care in women with ischemic stroke in the GWTG program. Stroke. 2009; 40:1127–1133.19. World Medical Association. World Medical Association Statement on Access of Women and Children to Health Care [Internet]. Ferney-Voltaire, France: WMA;[cited 2022 Dec 18]. Available from: https://www.wma.net/policiespost/wma-resolution-on-access-of-women-and-childrento-health-care-and-the-role-of-women-in-the-medicalprofession/.20. Ospel JM, Schaafsma JD, Leslie-Mazwi TM, Amin-Hanjani S, Asdaghi N, Gordon-Perue GL, et al. Toward a better understanding of sex-and gender-related differences in endovascular stroke treatment: a scientific statement from the American Heart Association/American Stroke Association. Stroke. 2022; 53:e396–e406.21. al-Rajeh S, Larbi EB, Bademosi O, Awada A, Yousef A, al-Freihi H, et al. Stroke register: experience from the eastern province of Saudi Arabia. Cerebrovasc Dis. 1998; 8:86–89.22. Al-Rukn S, Mazya M, Akhtar N, Hashim H, Mansouri B, Faouzi B, et al. Stroke in the Middle-East and North Africa: a 2-year prospective observational study of intravenous thrombolysis treatment in the region. Results from the SITS-MENA registry. Int J Stroke. 2020; 15:980–987.23. Foerch C, Misselwitz B, Humpich M, Steinmetz H, Neumann-Haefelin T, Sitzer M; Arbeitsgruppe Schlaganfall Hessen. Sex disparity in the access of elderly patients to acute stroke care. Stroke. 2007; 38:2123–2126.24. Bushnell C, Howard VJ, Lisabeth L, Caso V, Gall S, Kleindorfer D, et al. Sex differences in the evaluation and treatment of acute ischaemic stroke. Lancet Neurol. 2018; 17:641–650.25. Yu AYX, Penn AM, Lesperance ML, Croteau NS, Balshaw RF, Votova K, et al. Sex differences in presentation and outcome after an acute transient or minor neurologic event. JAMA Neurol. 2019; 76:962–968.26. Goadsby PJ, Lipton RB, Ferrari MD. Migraine--current understanding and treatment. N Engl J Med. 2002; 346:257–270.27. Yu AYX, Hill MD, Asdaghi N, Boulanger JM, Camden MC, Campbell BCV, et al. Sex differences in diagnosis and diagnostic revision of suspected minor cerebral ischemic events. Neurology. 2021; 96:e732–e739.28. Strong B, Lisabeth LD, Reeves M. Sex differences in IV thrombolysis treatment for acute ischemic stroke: a systematic review and meta-analysis. Neurology. 2020; 95:e11–e22.29. Kapral MK, Devon J, Winter AL, Wang J, Peters A, Bondy SJ. Gender differences in stroke care decision-making. Med Care. 2006; 44:70–80.30. Vahidy FS, Rahbar MH, Lal AP, Grotta JC, Savitz SI. Patient refusal of thrombolytic therapy for suspected acute ischemic stroke. Int J Stroke. 2015; 10:882–886.31. Pérez-Sánchez S, Barragán-Prieto A, Ortega-Quintanilla J, Domínguez-Mayoral A, Gamero-García MÁ, Zapata-Arriaza E, et al. Sex differences by hospital-level in performance and outcomes of endovascular treatment for acute ischemic stroke. J Stroke. 2020; 22:258–261.32. Lorenzano S, Ahmed N, Falcou A, Mikulik R, Tatlisumak T, Roffe C, et al. Does sex influence the response to intravenous thrombolysis in ischemic stroke?: answers from safe implementation of treatments in Stroke-International Stroke Thrombolysis Register. Stroke. 2013; 44:3401–3406.33. Spaander FH, Zinkstok SM, Baharoglu IM, Gensicke H, Polymeris A, Traenka C, et al. Sex differences and functional outcome after intravenous thrombolysis. Stroke. 2017; 48:699–703.34. Lekoubou A, Bishu KG, Ovbiagele B. Stroke thrombectomy utilization rates by sex: what were things like before 2015? J Stroke Cerebrovasc Dis. 2020; 29:104587.35. Otite FO, Saini V, Sur NB, Patel S, Sharma R, Akano EO, et al. Ten-year trend in age, sex, and racial disparity in tPA (Alteplase) and thrombectomy use following stroke in the United States. Stroke. 2021; 52:2562–2570.36. Weber R, Krogias C, Eyding J, Bartig D, Meves SH, Katsanos AH, et al. Age and sex differences in ischemic stroke treatment in a nationwide analysis of 1.11 million hospitalized cases. Stroke. 2019; 50:3494–3502.37. Sheth SA, Lee S, Warach SJ, Gralla J, Jahan R, Goyal M, et al. Sex differences in outcome after endovascular stroke therapy for acute ischemic stroke. Stroke. 2019; 50:2420–2427.38. Dmytriw AA, Ku JC, Yang VXD, Hui N, Uchida K, Morimoto T, et al. Do outcomes between women and men differ after endovascular thrombectomy? A meta-analysis. AJNR Am J Neuroradiol. 2021; 42:910–915.39. Chalos V, de Ridder IR, Lingsma HF, Brown S, van Oostenbrugge RJ, Goyal M, et al. Does sex modify the effect of endovascular treatment for ischemic stroke? Stroke. 2019; 50:2413–2419.40. Deb-Chatterji M, Schlemm E, Flottmann F, Meyer L, Alegiani A, Brekenfeld C, et al. Sex differences in outcome after thrombectomy for acute ischemic stroke are explained by confounding factors. Clin Neuroradiol. 2021; 31:1101–1109.41. Holloway RG, Arnold RM, Creutzfeldt CJ, Lewis EF, Lutz BJ, McCann RM, et al. Palliative and end-of-life care in stroke: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014; 45:1887–1916.42. Saver JL, Goyal M, van der Lugt A, Menon BK, Majoie CB, Dippel DW, et al. Time to treatment with endovascular thrombectomy and outcomes from ischemic stroke: a meta-analysis. JAMA. 2016; 316:1279–1288.43. Gardener H, Sacco RL, Rundek T, Battistella V, Cheung YK, Elkind MSV. Race and ethnic disparities in stroke incidence in the Northern Manhattan study. Stroke. 2020; 51:1064–1069.44. Petrea RE, Beiser AS, Seshadri S, Kelly-Hayes M, Kase CS, Wolf PA. Gender differences in stroke incidence and poststroke disability in the Framingham heart study. Stroke. 2009; 40:1032–1037.45. Peters SAE, Carcel C, Millett ERC, Woodward M. Sex differences in the association between major risk factors and the risk of stroke in the UK Biobank cohort study. Neurology. 2020; 95:e2715–e2726.46. Peters SA, Huxley RR, Woodward M. Comparison of the sex-specific associations between systolic blood pressure and the risk of cardiovascular disease: a systematic review and meta-analysis of 124 cohort studies, including 1.2 million individuals. Stroke. 2013; 44:2394–2401.47. Madsen TE, Howard G, Kleindorfer DO, Furie KL, Oparil S, Manson JE, et al. Sex differences in hypertension and stroke risk in the REGARDS study: a longitudinal cohort study. Hypertension. 2019; 74:749–755.48. Demel SL, Kittner S, Ley SH, McDermott M, Rexrode KM. Stroke risk factors unique to women. Stroke. 2018; 49:518–523.49. Li C, Hedblad B, Rosvall M, Buchwald F, Khan FA, Engström G. Stroke incidence, recurrence, and case-fatality in relation to socioeconomic position: a population-based study of middle-aged Swedish men and women. Stroke. 2008; 39:2191–2196.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Sex and Gender Medicine in Pancreatobiliary Diseases
- Sex or gender differences in treatment outcomes of sepsis and septic shock
- Gender Differences in the Functional Recovery after Acute Stroke
- Organization of Stroke Care System: Stroke Unit and Stroke Center
- Psychotropics Metabolism: Gender-Related Issues