J Korean Neurosurg Soc.
2023 Jan;66(1):72-81. 10.3340/jkns.2022.0071.
Differences in Clinical Characteristics and Surgical Outcomes of Patients with Ischemic and Hemorrhagic Pituitary Adenomas
- Affiliations
-
- 1Department of Neurosurgery, Xinqiao Hospital, Army Medical University, Chongqing, China
- 2Multidisciplinary Center for Pituitary Adenomas of Chongqing, Chongqing, China
- 3Department of Endocrinology, Xinqiao Hospital, Army Medical University, Chongqing, China
- 4Department of Pathology, Xinqiao Hospital, Army Medical University, Chongqing, China
- KMID: 2537850
- DOI: http://doi.org/10.3340/jkns.2022.0071
Abstract
Objective
: Ischemia and hemorrhage of pituitary adenomas (PA) caused important clinical syndrome. However, the differences on clinical characteristics and surgical outcomes between these two kinds apoplexy were less reported.
Methods
: A retrospective analysis was made of patients with pituitary apoplexy between January 2013 and June 2018. Baseline and clinical characteristics before surgery were reviewed. All patients underwent transsphenoidal surgery and were followed up at least 1 year.
Results
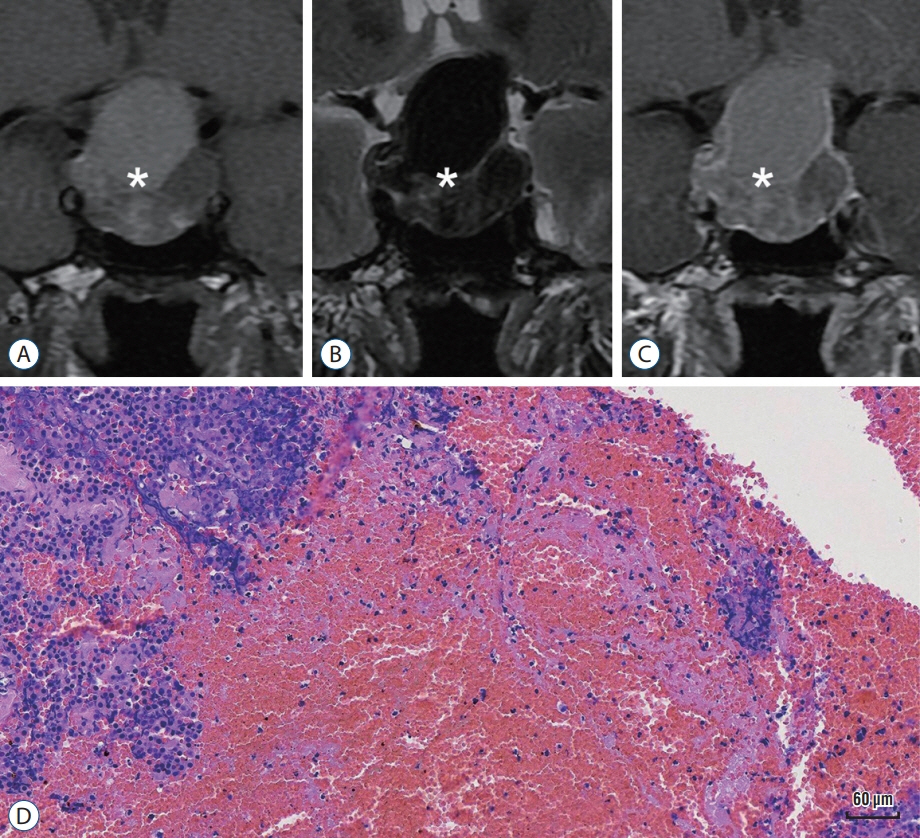
: Total 67 cases (5.8%) among 1147 pituitary tumor patients were enrolled, which consisted of 28 (~2.4%) ischemic PA and 39 (~3.4%) hemorrhagic PA. There were more male patients in the ischemic group compared with hemorrhagic group (78.6% vs 53.8%, p=0.043). However, the mean age, tumor size and functional tumor ratio were significant higher in the hemorrhagic group. Headache was more common in ischemic PA (82.1%) than that of hemorrhagic PA (51.3%, p=0.011). Magnetic resonance imaging findings found that mucosal thickening and enhancement of the sphenoid sinus was observed in 15 ischemic PA patients (n=27, 55.6%), but none in patients with hemorrhagic PA (n=38, p<0.0001). It was worth noting that the rate of pre-surgical hypopituitarism in ischemic PA patients were seemed higher than that in hemorrhagic PA patients, but not significant. The two groups got a total tumor resection rate at 94.1% and 92.9%, independently. No significant difference on the operative time, blood loss in operation and complications in perioperative period was observed in two groups. After operation, cranial nerve symptoms recovered to normal at 81.8% of ischemic PA patients and 82.6% of hemorrhagic PA patients. Importantly, the incidence of postoperative hypopituitarism partially decreased in both groups, among which the rate of hypothyroidism in ischemic PA patients significantly decreased from 46.4% to 18.5% (p=0.044).
Conclusion
: Patients with ischemic PA presented different clinical characteristics to the hemorrhagic ones. Transsphenoidal surgery should be considered for the patients with neuro-ophthalmic deficits and might benefit for pituitary function recovery of the apoplectic adenoma patients, especially pituitary thyroid axis in ischemic PA patients.
Figure
Reference
-
References
1. Agrawal B, Dziurzynski K, Salamat MS, Baskaya M. The temporal association of sphenoid sinus mucosal thickening on MR imaging with pituitary apoplexy. Turk Neurosurg. 22:785–790. 2012.2. Arita K, Kurisu K, Tominaga A, Sugiyama K, Ikawa F, Yoshioka H, et al. Thickening of sphenoid sinus mucosa during the acute stage of pituitary apoplexy. J Neurosurg. 95:897–901. 2001.3. Boellis A, di Napoli A, Romano A, Bozzao A. Pituitary apoplexy: an update on clinical and imaging features. Insights Imaging. 5:753–762. 2014.4. Chang CV, Felicio AC, Toscanini AC, Teixeira MJ, Cunha-Neto MB. Pituitary tumor apoplexy. Arq Neuropsiquiatr. 67:328–333. 2009.5. Falhammar H, Tornvall S, Höybye C. Pituitary apoplexy: a retrospective study of 33 cases from a single center. Front Endocrinol (Lausanne). 12:656950. 2021.6. Fernandez A, Karavitaki N, Wass JA. Prevalence of pituitary adenomas: a community-based, cross-sectional study in Banbury (Oxfordshire, UK). Clin Endocrinol (Oxf). 72:377–382. 2010.7. Gupta P, Dutta P. Landscape of molecular events in pituitary apoplexy. Front Endocrinol (Lausanne). 9:107. 2018.8. Jho DH, Biller BM, Agarwalla PK, Swearingen B. Pituitary apoplexy: large surgical series with grading system. World Neurosurg. 82:781–790. 2014.9. Liu JK, Couldwell WT. Pituitary apoplexy in the magnetic resonance imaging era: clinical significance of sphenoid sinus mucosal thickening. J Neurosurg. 104:892–898. 2006.10. Ly S, Naman A, Chaufour-Higel B, Patey M, Arndt C, Delemer B, et al. Pituitary apoplexy and rivaroxaban. Pituitary. 20:709–710. 2017.11. Ogawa Y, Niizuma K, Mugikura S, Tominaga T. Ischemic pituitary adenoma apoplexy-clinical appearance and prognosis after surgical intervention. Clin Neurol Neurosurg. 148:142–146. 2016.12. Oldfield EH, Merrill MJ. Apoplexy of pituitary adenomas: the perfect storm. J Neurosurg. 122:1444–1449. 2015.13. Pyrgelis ES, Mavridis I, Meliou M. Presenting symptoms of pituitary apoplexy. J Neurol Surg A Cent Eur Neurosurg. 79:52–59. 2018.14. Rajasekaran S, Vanderpump M, Baldeweg S, Drake W, Reddy N, Lanyon M, et al. UK guidelines for the management of pituitary apoplexy. Clin Endocrinol (Oxf). 74:9–20. 2011.15. Vaphiades MS. Pituitary ring sign plus sphenoid sinus mucosal thickening: neuroimaging signs of pituitary apoplexy. Neuroophthalmology. 41:306–309. 2017.16. Wang Z, Gao L, Wang W, Guo X, Feng C, Lian W, et al. Coagulative necrotic pituitary adenoma apoplexy: a retrospective study of 21 cases from a large pituitary center in China. Pituitary. 22:13–28. 2019.17. Waqar M, McCreary R, Kearney T, Karabatsou K, Gnanalingham KK. Sphenoid sinus mucosal thickening in the acute phase of pituitary apoplexy. Pituitary. 20:441–449. 2017.18. Wildemberg LE, Glezer A, Bronstein MD, Gadelha MR. Apoplexy in nonfunctioning pituitary adenomas. Pituitary. 21:138–144. 2018.19. Xiao D, Wang S, Huang Y, Zhao L, Wei L, Ding C. Clinical analysis of infarction in pituitary adenoma. Int J Clin Exp Med. 8:7477–7486. 2015.20. Zhan R, Zhao Y, Wiebe TM, Li X. Acute hemorrhagic apoplectic pituitary adenoma: endoscopic management, surgical outcomes, and complications. J Craniofac Surg. 26:e510–515. 2015.21. Zhu Q, Liang Y, Fan Z, Liu Y, Zhou C, Zhang H, et al. Ischemic infarction of pituitary apoplexy: a retrospective study of 46 cases from a single tertiary center. Front Neurosci. 15:808111. 2022.