J Korean Assoc Oral Maxillofac Surg.
2022 Oct;48(5):259-266. 10.5125/jkaoms.2022.48.5.259.
Associations between obstructive sleep apnea and painful temporomandibular disorder: a systematic review
- Affiliations
-
- 1Clinic of Oral Medicine and Orofacial Pain, Ajou University School of Medicine, Suwon, Korea
- 2Department of Oral and Maxillofacial Surgery, Institute of Oral Health Science, Ajou University School of Medicine, Suwon, Korea
- KMID: 2534805
- DOI: http://doi.org/10.5125/jkaoms.2022.48.5.259
Abstract
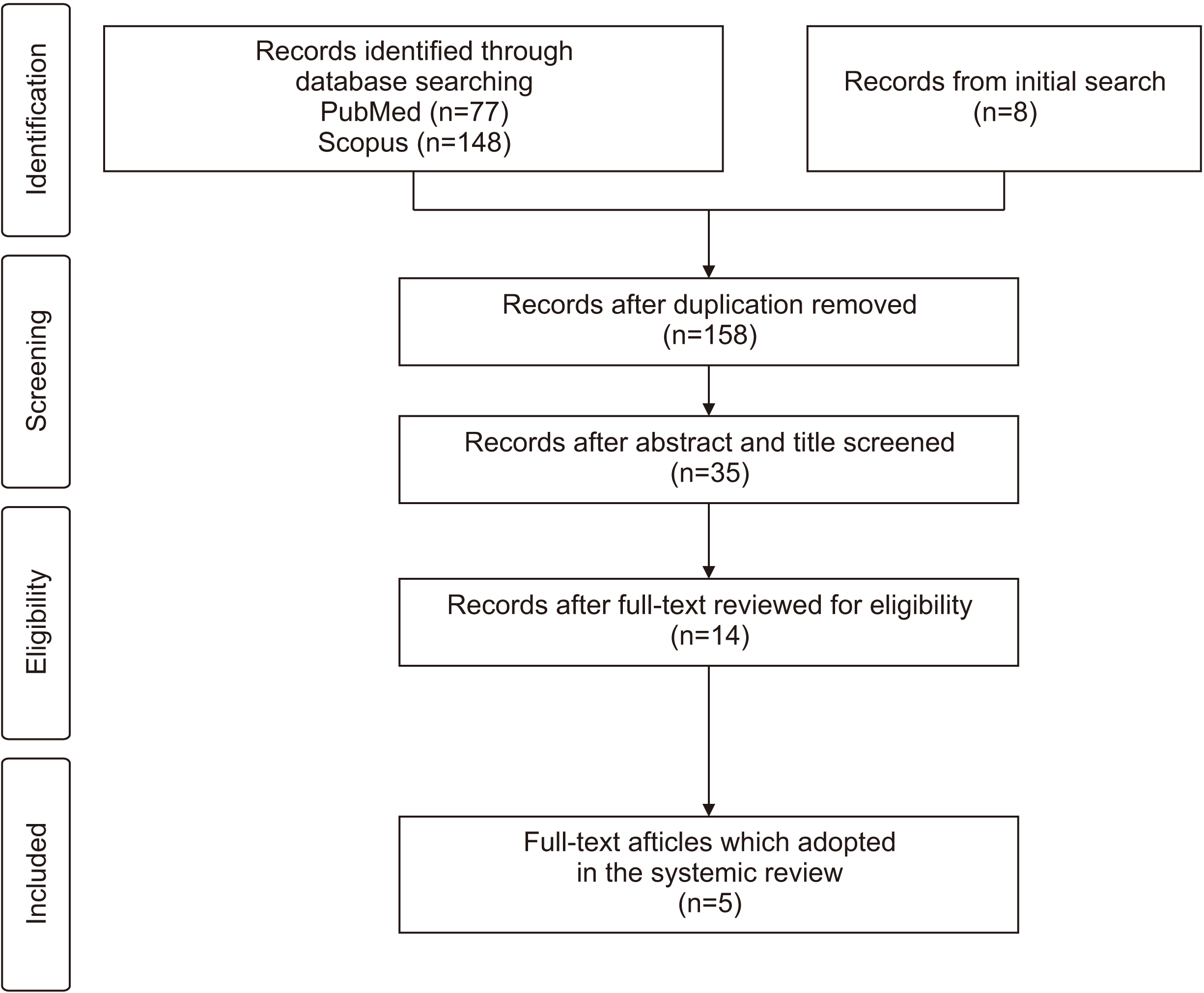
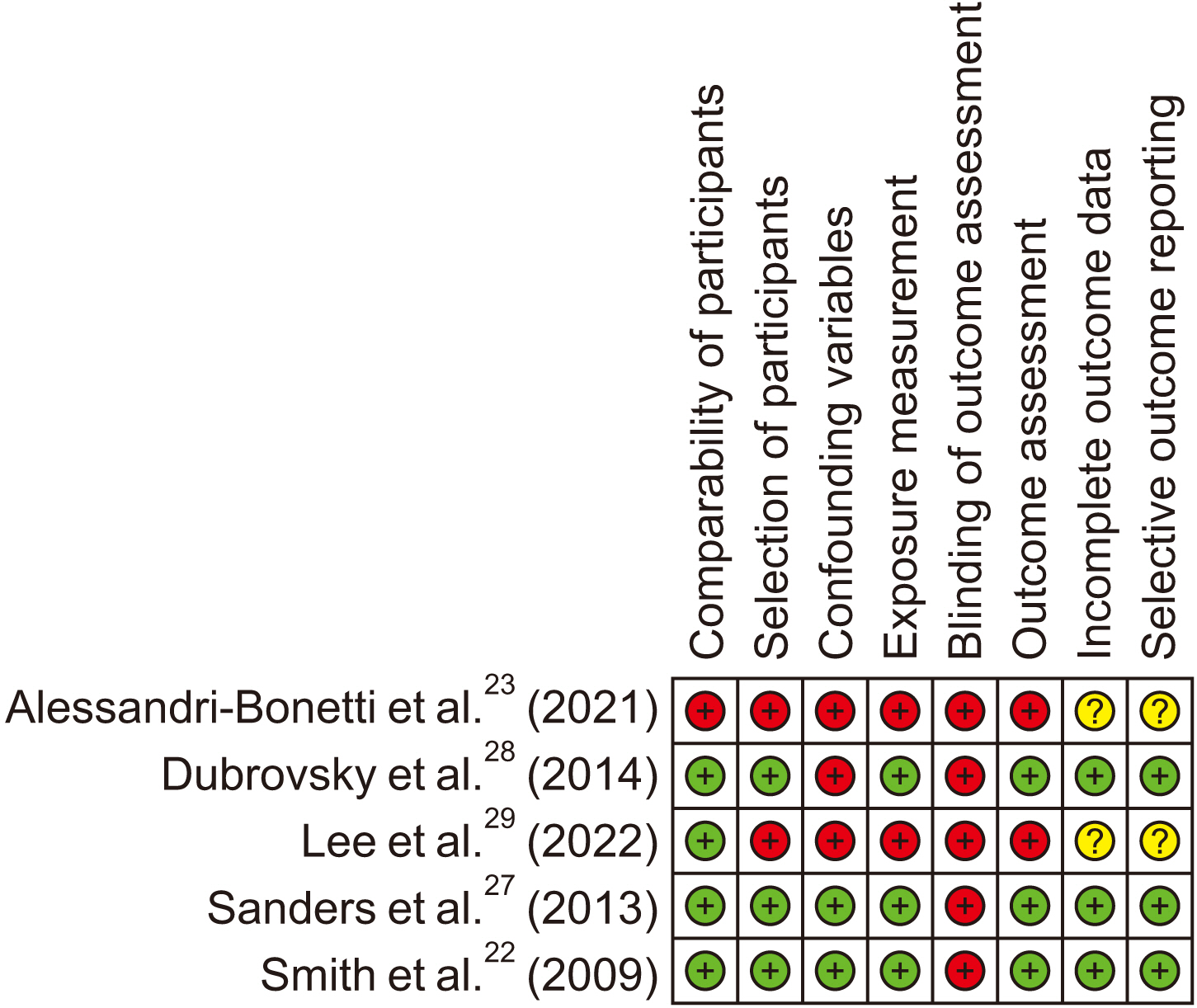
- The relationship between obstructive sleep apnea (OSA) and diverse types of pain conditions have been proposed. However, no consensus on the relationship between OSA and painful temporomandibular disorders (TMDs) has been established. Therefore, this systematic review has been conducted to review the existing literatures and provide comprehensive synthesis of such literatures about OSA and painful TMDs using the evidence-based methodology. A literature search was conducted using two electronic databases, Scopus, and PubMed. Risk of bias was assessed using the risk-ofbias assessment tool for non-randomized study version 2.0. A total of 158 articles were screened from the initial search and eventually, 5 articles were included in this systematic review. One study adopted both the longitudinal prospective cohort and case-control designs and other 4 articles adopted the cross-sectional design. Two studies employed polysomnography (PSG) for the diagnosis of OSA and mentioned the results from the PSG. All crosssectional studies demonstrated higher OSA prevalence among patients with TMD, and one cohort study suggested OSA as a risk factor for TMD. OSA appears to have potential influences on the development of TMD; however, the role of TMD in the development of OSA remains to be unknown owing to the lack of high-quality evidences.
Keyword
Figure
Reference
-
References
1. de Leeuw Reny, Klasser G. 2018. Orofacial pain: guidelines for assessment, diagnosis, and management. 6th ed. Quintessence;Batavia (IL):2. Dahan H, Shir Y, Velly A, Allison P. 2015; Specific and number of comorbidities are associated with increased levels of temporomandibular pain intensity and duration. J Headache Pain. 16:528. https://doi.org/10.1186/s10194-015-0528-2. DOI: 10.1186/s10194-015-0528-2. PMID: 26002637. PMCID: PMC4441879.
Article3. Hoffmann RG, Kotchen JM, Kotchen TA, Cowley T, Dasgupta M, Cowley AW Jr. 2011; Temporomandibular disorders and associated clinical comorbidities. Clin J Pain. 27:268–74. https://doi.org/10.1097/AJP.0b013e31820215f5. DOI: 10.1097/AJP.0b013e31820215f5. PMID: 21178593.
Article4. Al-Jewair T, Shibeika D, Ohrbach R. 2021; Temporomandibular disorders and their association with sleep disorders in adults: a systematic review. J Oral Facial Pain Headache. 35:41–53. https://doi.org/10.11607/ofph.2780. DOI: 10.11607/ofph.2780. PMID: 33730126.
Article5. Almoznino G, Benoliel R, Sharav Y, Haviv Y. 2017; Sleep disorders and chronic craniofacial pain: characteristics and management possibilities. Sleep Med Rev. 33:39–50. https://doi.org/10.1016/j.smrv.2016.04.005. DOI: 10.1016/j.smrv.2016.04.005. PMID: 27321865.
Article6. Burr MR, Naze GS, Shaffer SM, Emerson AJ. 2021; The role of sleep dysfunction in temporomandibular onset and progression: a systematic review and meta-analyses. J Oral Rehabil. 48:183–94. https://doi.org/10.1111/joor.13127. DOI: 10.1111/joor.13127. PMID: 33211331.
Article7. Dreweck FDS, Soares S, Duarte J, Conti PCR, De Luca Canto G, Luís Porporatti A. 2020; Association between painful temporomandibular disorders and sleep quality: a systematic review. J Oral Rehabil. 47:1041–51. https://doi.org/10.1111/joor.12993. DOI: 10.1111/joor.12993. PMID: 32395855.
Article8. Kim HK, Kim ME. 2021; Phenotyping 1488 patients with painful temporomandibular disorders and its relevance to subjective sleep quality: a key step for stratified medicine. Cranio. 39:491–501. https://doi.org/10.1080/08869634.2019.1682750. DOI: 10.1080/08869634.2019.1682750. PMID: 31662051.
Article9. Lerman SF, Mun CJ, Hunt CA, Kunatharaju S, Buenaver LF, Finan PH, et al. 2022; Insomnia with objective short sleep duration in women with temporomandibular joint disorder: quantitative sensory testing, inflammation and clinical pain profiles. Sleep Med. 90:26–35. https://doi.org/10.1016/j.sleep.2022.01.004. DOI: 10.1016/j.sleep.2022.01.004. PMID: 35091170. PMCID: PMC8923986.
Article10. Roithmann CC, Silva CAGD, Pattussi MP, Grossi ML. 2021; Subjective sleep quality and temporomandibular disorders: systematic literature review and meta-analysis. J Oral Rehabil. 48:1380–94. https://doi.org/10.1111/joor.13265. DOI: 10.1111/joor.13265. PMID: 34599524.
Article11. Schütz TC, Andersen ML, Tufik S. 2009; The influence of orofacial pain on sleep pattern: a review of theory, animal models and future directions. Sleep Med. 10:822–8. https://doi.org/10.1016/j.sleep.2008.09.018. DOI: 10.1016/j.sleep.2008.09.018. PMID: 19195929.
Article12. Sommer I, Lavigne G, Ettlin DA. 2015; Review of self-reported instruments that measure sleep dysfunction in patients suffering from temporomandibular disorders and/or orofacial pain. Sleep Med. 16:27–38. https://doi.org/10.1016/j.sleep.2014.07.023. DOI: 10.1016/j.sleep.2014.07.023. PMID: 25547038.
Article13. Rener-Sitar K, John MT, Pusalavidyasagar SS, Bandyopadhyay D, Schiffman EL. 2016; Sleep quality in temporomandibular disorder cases. Sleep Med. 25:105–12. https://doi.org/10.1016/j.sleep.2016.06.031. DOI: 10.1016/j.sleep.2016.06.031. PMID: 27823702. PMCID: PMC5376270.
Article14. Yatani H, Studts J, Cordova M, Carlson CR, Okeson JP. 2002; Comparison of sleep quality and clinical and psychologic characteristics in patients with temporomandibular disorders. J Orofac Pain. 16:221–8. PMID: 12221738.15. Kang J, Tian Z, Wei J, Mu Z, Liang J, Li M. 2022; Association between obstructive sleep apnea and Alzheimer's disease-related blood and cerebrospinal fluid biomarkers: a meta-analysis. J Clin Neurosci. 102:87–94. https://doi.org/10.1016/j.jocn.2022.06.004. DOI: 10.1016/j.jocn.2022.06.004. PMID: 35753156.
Article16. Marshall NS, Wong KK, Liu PY, Cullen SR, Knuiman MW, Grunstein RR. 2008; Sleep apnea as an independent risk factor for all-cause mortality: the Busselton health study. Sleep. 31:1079–85. DOI: 10.5665/sleep/31.8.1079. PMID: 18714779. PMCID: PMC2542953.17. Peker Y, Carlson J, Hedner J. 2006; Increased incidence of coronary artery disease in sleep apnoea: a long-term follow-up. Eur Respir J. 28:596–602. https://doi.org/10.1183/09031936.06.00107805. DOI: 10.1183/09031936.06.00107805. PMID: 16641120.
Article18. Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass LM, Mohsenin V. 2005; Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med. 353:2034–41. https://doi.org/10.1056/NEJMoa043104. DOI: 10.1056/NEJMoa043104. PMID: 16282178.
Article19. Young T, Finn L, Peppard PE, Szklo-Coxe M, Austin D, Nieto FJ, et al. 2008; Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin sleep cohort. Sleep. 31:1071–8. DOI: 10.5665/sleep/31.8.1071. PMID: 18714778. PMCID: PMC2542952.20. Roehrs T, Hyde M, Blaisdell B, Greenwald M, Roth T. 2006; Sleep loss and REM sleep loss are hyperalgesic. Sleep. 29:145–51. https://doi.org/10.1093/sleep/29.2.145. DOI: 10.1093/sleep/29.2.145. PMID: 16494081.
Article21. Kaczmarski P, Karuga FF, Szmyd B, Sochal M, Białasiewicz P, Strzelecki D, et al. 2022; The role of inflammation, hypoxia, and opioid receptor expression in pain modulation in patients suffering from obstructive sleep apnea. Int J Mol Sci. 23:9080. https://doi.org/10.3390/ijms23169080. DOI: 10.3390/ijms23169080. PMID: 36012341. PMCID: PMC9409023.
Article22. Smith MT, Wickwire EM, Grace EG, Edwards RR, Buenaver LF, Peterson S, et al. 2009; Sleep disorders and their association with laboratory pain sensitivity in temporomandibular joint disorder. Sleep. 32:779–90. https://doi.org/10.1093/sleep/32.6.779. DOI: 10.1093/sleep/32.6.779. PMID: 19544755. PMCID: PMC2690566.
Article23. Alessandri-Bonetti A, Scarano E, Fiorita A, Cordaro M, Gallenzi P. 2021; Prevalence of signs and symptoms of temporo-mandibular disorder in patients with sleep apnea. Sleep Breath. 25:2001–6. https://doi.org/10.1007/s11325-021-02337-9. DOI: 10.1007/s11325-021-02337-9. PMID: 33674964.
Article24. Maixner W, Greenspan JD, Dubner R, Bair E, Mulkey F, Miller V, et al. 2011; Potential autonomic risk factors for chronic TMD: descriptive data and empirically identified domains from the OPPERA case-control study. J Pain. 12(11 Suppl):T75–91. https://doi.org/10.1016/j.jpain.2011.09.002. DOI: 10.1016/j.jpain.2011.09.002. PMID: 22074754. PMCID: PMC3233841.
Article25. Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. 2015; ; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 4:1. https://doi.org/10.1186/2046-4053-4-1. DOI: 10.1186/2046-4053-4-1. PMID: 25554246. PMCID: PMC4320440.
Article26. Kim SY, Park JE, Lee YJ, Seo HJ, Sheen SS, Hahn S, Jang BH, et al. 2013; Testing a tool for assessing the risk of bias for nonrandomized studies showed moderate reliability and promising validity. J Clin Epidemiol. 66:408–14. https://doi.org/10.1016/j.jclinepi.2012.09.016. DOI: 10.1016/j.jclinepi.2012.09.016. PMID: 23337781.
Article27. Sanders AE, Essick GK, Fillingim R, Knott C, Ohrbach R, Greenspan JD, et al. 2013; Sleep apnea symptoms and risk of temporomandibular disorder: OPPERA cohort. J Dent Res. 92(7 Suppl):70S–77S. https://doi.org/10.1177/0022034513488140. DOI: 10.1177/0022034513488140. PMID: 23690360. PMCID: PMC3706181.
Article28. Dubrovsky B, Raphael KG, Lavigne GJ, Janal MN, Sirois DA, Wigren PE, et al. 2014; Polysomnographic investigation of sleep and respiratory parameters in women with temporomandibular pain disorders. J Clin Sleep Med. 10:195–201. https://doi.org/10.5664/jcsm.3452. DOI: 10.5664/jcsm.3452. PMID: 24533003. PMCID: PMC3899322.
Article29. Lee YH, Auh QS, An JS, Kim T. 2022; Poorer sleep quality in patients with chronic temporomandibular disorders compared to healthy controls. BMC Musculoskelet Disord. 23:246. https://doi.org/10.1186/s12891-022-05195-y. DOI: 10.1186/s12891-022-05195-y. PMID: 35287633. PMCID: PMC8922910.
Article30. Jennum P, Drewes AM, Andreasen A, Nielsen KD. 1993; Sleep and other symptoms in primary fibromyalgia and in healthy controls. J Rheumatol. 20:1756–9. PMID: 8295190.31. Olmos SR. 2016; Comorbidities of chronic facial pain and obstructive sleep apnea. Curr Opin Pulm Med. 22:570–5. DOI: 10.1097/MCP.0000000000000325. PMID: 27662470.
Article32. Doufas AG, Tian L, Davies MF, Warby SC. 2013; Nocturnal intermittent hypoxia is independently associated with pain in subjects suffering from sleep-disordered breathing. Anesthesiology. 119:1149–62. https://doi.org/10.1097/ALN.0b013e3182a951fc. DOI: 10.1097/ALN.0b013e3182a951fc. PMID: 24025612.
Article33. Lam KK, Kunder S, Wong J, Doufas AG, Chung F. 2016; Obstructive sleep apnea, pain, and opioids: is the riddle solved? Curr Opin Anaesthesiol. 29:134–40. https://doi.org/10.1097/ACO.0000000000000265. DOI: 10.1097/ACO.0000000000000265. PMID: 26545144. PMCID: PMC4927322.
Article34. Ratnavadivel R, Chau N, Stadler D, Yeo A, McEvoy RD, Catcheside PG. 2009; Marked reduction in obstructive sleep apnea severity in slow wave sleep. J Clin Sleep Med. 5:519–24. DOI: 10.5664/jcsm.27651. PMID: 20465017. PMCID: PMC2792966.
Article35. Bonnet MH, Arand DL. 2003; Clinical effects of sleep fragmentation versus sleep deprivation. Sleep Med Rev. 7:297–310. https://doi.org/10.1053/smrv.2001.0245. DOI: 10.1053/smrv.2001.0245. PMID: 14505597.
Article36. Choy EH. 2015; The role of sleep in pain and fibromyalgia. Nat Rev Rheumatol. 11:513–20. https://doi.org/10.1038/nrrheum.2015.56. DOI: 10.1038/nrrheum.2015.56. PMID: 25907704.
Article37. de Feijter M, Katimertzoglou A, Tiemensma J, Ikram MA, Luik AI. 2022; Polysomnography-estimated sleep and the negative feedback loop of the hypothalamic-pituitary-adrenal (HPA) axis. Psychoneuroendocrinology. 141:105749. https://doi.org/10.1016/j.psyneuen.2022.105749. DOI: 10.1016/j.psyneuen.2022.105749. PMID: 35427952.
Article38. Jo KB, Lee YJ, Lee IG, Lee SC, Park JY, Ahn RS. 2016; Association of pain intensity, pain-related disability, and depression with hypothalamus-pituitary-adrenal axis function in female patients with chronic temporomandibular disorders. Psychoneuroendocrinology. 69:106–15. https://doi.org/10.1016/j.psyneuen.2016.03.017. DOI: 10.1016/j.psyneuen.2016.03.017. PMID: 27082645.
Article39. Doufas AG, Tian L, Padrez KA, Suwanprathes P, Cardell JA, Maecker HT, et al. 2013; Experimental pain and opioid analgesia in volunteers at high risk for obstructive sleep apnea. PLoS One. 8:e54807. https://doi.org/10.1371/journal.pone.0054807. DOI: 10.1371/journal.pone.0054807. PMID: 23382975. PMCID: PMC3558510.
Article40. Fang D, Kong LY, Cai J, Li S, Liu XD, Han JS, et al. 2015; Interleukin-6-mediated functional upregulation of TRPV1 receptors in dorsal root ganglion neurons through the activation of JAK/PI3K signaling pathway: roles in the development of bone cancer pain in a rat model. Pain. 156:1124–44. https://doi.org/10.1097/j.pain.0000000000000158. DOI: 10.1097/j.pain.0000000000000158. PMID: 25775359.
Article41. Yokoe T, Minoguchi K, Matsuo H, Oda N, Minoguchi H, Yoshino G, et al. 2003; Elevated levels of C-reactive protein and interleukin-6 in patients with obstructive sleep apnea syndrome are decreased by nasal continuous positive airway pressure. Circulation. 107:1129–34. https://doi.org/10.1161/01.cir.0000052627.99976.18. DOI: 10.1161/01.CIR.0000052627.99976.18. PMID: 12615790.
Article42. Kawasaki Y, Zhang L, Cheng JK, Ji RR. 2008; Cytokine mechanisms of central sensitization: distinct and overlapping role of interleukin-1beta, interleukin-6, and tumor necrosis factor-alpha in regulating synaptic and neuronal activity in the superficial spinal cord. J Neurosci. 28:5189–94. https://doi.org/10.1523/JNEUROSCI.3338-07.2008. DOI: 10.1523/JNEUROSCI.3338-07.2008. PMID: 18480275. PMCID: PMC2408767.
Article43. Ji RR, Nackley A, Huh Y, Terrando N, Maixner W. 2018; Neuroinflammation and central sensitization in chronic and widespread pain. Anesthesiology. 129:343–66. https://doi.org/10.1097/ALN.0000000000002130. DOI: 10.1097/ALN.0000000000002130. PMID: 29462012. PMCID: PMC6051899.
Article44. Goksan B, Gunduz A, Karadeniz D, Ağan K, Tascilar FN, Tan F, et al. 2009; Morning headache in sleep apnoea: clinical and polysomnographic evaluation and response to nasal continuous positive airway pressure. Cephalalgia. 29:635–41. https://doi.org/10.1111/j.1468-2982.2008.01781.x. DOI: 10.1111/j.1468-2982.2008.01781.x. PMID: 19187338.
Article45. Kallweit U, Hidalgo H, Uhl V, Sándor PS. 2011; Continuous positive airway pressure therapy is effective for migraines in sleep apnea syndrome. Neurology. 76:1189–91. https://doi.org/10.1212/WNL.0b013e318212aad0. DOI: 10.1212/WNL.0b013e318212aad0. PMID: 21444907.
Article46. Charokopos A, Card ME, Gunderson C, Steffens C, Bastian LA. 2018; The association of obstructive sleep apnea and pain outcomes in adults: a systematic review. Pain Med. 19(Suppl 1):S69–75. https://doi.org/10.1093/pm/pny140. DOI: 10.1093/pm/pny140. PMID: 30203008.
Article47. Oh JT, Chung JW. 2016; Inflammatory cytokine level in patients with obstructive sleep apnea and treatment outcome of oral appliance therapy. J Oral Med Pain. 41:126–32. DOI: 10.14476/jomp.2016.41.3.126.
Article48. Doff MH, Veldhuis SK, Hoekema A, Slater JJ, Wijkstra PJ, de Bont LG, et al. 2012; Long-term oral appliance therapy in obstructive sleep apnea syndrome: a controlled study on temporomandibular side effects. Clin Oral Investig. 16:689–97. https://doi.org/10.1007/s00784-011-0555-6. DOI: 10.1007/s00784-011-0555-6. PMID: 21538074.
Article49. El-Solh AA, Homish GG, Ditursi G, Lazarus J, Rao N, Adamo D, et al. 2017; A randomized crossover trial evaluating continuous positive airway pressure versus mandibular advancement device on health outcomes in veterans with posttraumatic stress disorder. J Clin Sleep Med. 13:1327–35. https://doi.org/10.5664/jcsm.6808. DOI: 10.5664/jcsm.6808. PMID: 29065960. PMCID: PMC5656482.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Long-Term Side Effects of Mandibular Advancement Devices in Patients with Obstructive Sleep Apnea
- Upper airway myofunctional exercise: a systematic review
- Effects of Menopause on Obstructive Sleep Apnea
- Complications of Obstructive Sleep Apnea
- A Review on Sleep Disorders Similar to REM Sleep Behavior Disorder