Ann Surg Treat Res.
2022 Aug;103(2):72-80. 10.4174/astr.2022.103.2.72.
Preoperative lymphocyte-to-C-reactive protein ratio predicts hepatocellular carcinoma recurrence after surgery
- Affiliations
-
- 1Department of Surgery, National Hospital Organization Fukuyama Medical Center, Fukuyama, Japan
- KMID: 2532361
- DOI: http://doi.org/10.4174/astr.2022.103.2.72
Abstract
- Purpose
This study was performed to determine the prognostic value of lymphocyte-to-CRP ratio after curative resection for hepatocellular carcinoma.
Methods
Between July 2010 and October 2021, 173 consecutive patients (144 male, 29 female) who underwent surgical resection for pathologically confirmed hepatocellular carcinoma were included in this retrospective study. Cox regression analysis was used to evaluate the relationship between clinicopathological characteristics and recurrence-free survival (RFS) and overall survival (OS). A P-value of <0.05 was considered statistically significant.
Results
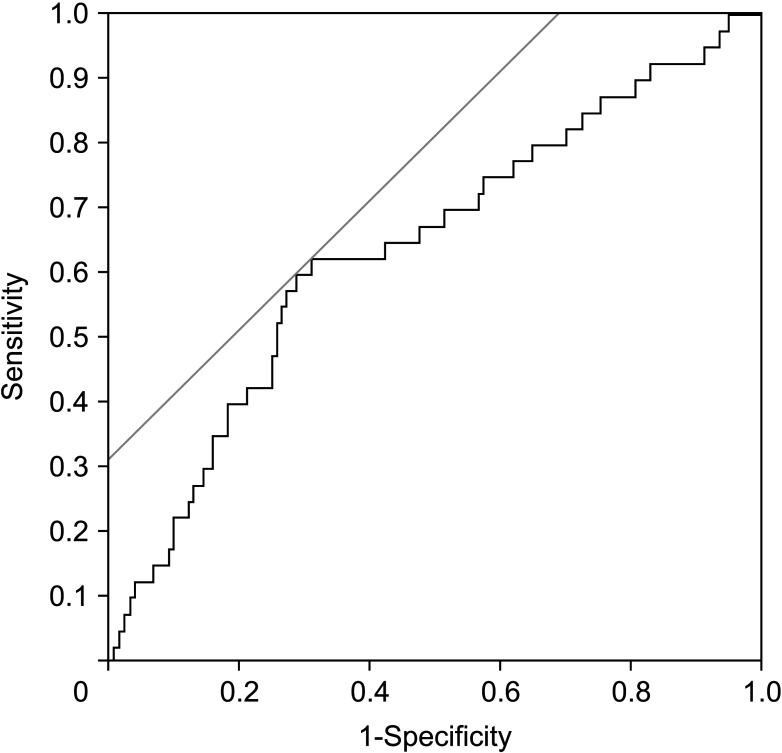
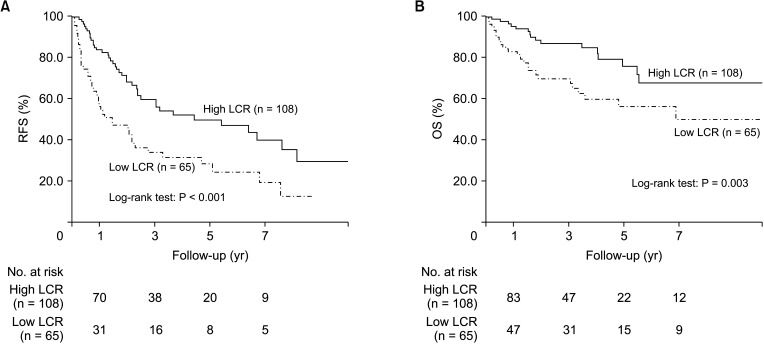
The patients (mean age, 71 years) were stratified into high (≥9,500, n = 108) and low (<9,500, n = 65) lymphocyteto-CRP ratio groups. The low lymphocyte-to-CRP ratio group had significantly worse RFS and OS. Low lymphocyte-toCRP ratio (hazard ratio [HR], 1.865; 95% confidence interval [CI], 1.176–2.960; P = 0.008), multiple tumors (HR, 3.333; 95% CI, 2.042–5.343; P < 0.001), and microvascular invasion (HR, 1.934; 95% CI, 1.178–3.184; P = 0.009) were independently associated with RFS, whereas low albumin-to-globulin ratio (HR, 2.270; 95% CI, 1.074–4.868; P = 0.032), α-FP of ≥25 ng/mL (HR, 2.187; 95% CI, 1.115–4.259; P = 0.023), and poor tumor differentiation (HR, 2.781; 95% CI, 1.041–6.692; P = 0.042) were independently associated with OS. Lymphocyte-to-CRP ratio had a higher area under the curve (0.635) than other inflammation-based markers (0.51–0.63).
Conclusion
Lymphocyte-to-CRP ratio is superior to other inflammation-based markers as a predictor of RFS in patients with surgically resected hepatocellular carcinoma.
Figure
Reference
-
1. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021; 71:209–249. PMID: 33538338.
Article2. You DD, Kim DG, Seo CH, Choi HJ, Yoo YK, Park YG. Prognostic factors after curative resection hepatocellular carcinoma and the surgeon’s role. Ann Surg Treat Res. 2017; 93:252–259. PMID: 29184878.
Article3. Huang J, Yan L, Cheng Z, Wu H, Du L, Wang J, et al. A randomized trial comparing radiofrequency ablation and surgical resection for HCC conforming to the Milan criteria. Ann Surg. 2010; 252:903–912. PMID: 21107100.
Article4. Kabbach G, Assi HA, Bolotin G, Schuster M, Lee HJ, Tadros M. Hepatobiliary tumors: update on diagnosis and management. J Clin Transl Hepatol. 2015; 3:169–181. PMID: 26623263.
Article5. Maida M, Orlando E, Cammà C, Cabibbo G. Staging systems of hepatocellular carcinoma: a review of literature. World J Gastroenterol. 2014; 20:4141–4150. PMID: 24764652.
Article6. Crusz SM, Balkwill FR. Inflammation and cancer: advances and new agents. Nat Rev Clin Oncol. 2015; 12:584–596. PMID: 26122183.
Article7. Diakos CI, Charles KA, McMillan DC, Clarke SJ. Cancer-related inflammation and treatment effectiveness. Lancet Oncol. 2014; 15:e493–e503. PMID: 25281468.
Article8. Utsumi M, Kitada K, Tokunaga N, Narusaka T, Hamano R, Miyasou H, et al. Preoperative albumin-to-globulin ratio predicts prognosis in hepatocellular carcinoma: a cohort study including non-hepatitis virus-infected patients. Dig Surg. 2021; 38:307–315. PMID: 34515102.
Article9. Chan SL, Chan AW, Chan AK, Jian P, Mo F, Chan CM, et al. Systematic evaluation of circulating inflammatory markers for hepatocellular carcinoma. Liver Int. 2017; 37:280–289. PMID: 27501075.
Article10. Mano Y, Shirabe K, Yamashita Y, Harimoto N, Tsujita E, Takeishi K, et al. Preoperative neutrophil-to-lymphocyte ratio is a predictor of survival after hepatectomy for hepatocellular carcinoma: a retrospective analysis. Ann Surg. 2013; 258:301–305. PMID: 23774313.
Article11. Chan AW, Chan SL, Wong GL, Wong VW, Chong CC, Lai PB, et al. Prognostic Nutritional Index (PNI) predicts tumor recurrence of very early/early stage hepatocellular carcinoma after surgical resection. Ann Surg Oncol. 2015; 22:4138–4148. PMID: 25801356.
Article12. Wang Y, Attar BM, Fuentes HE, Jaiswal P, Tafur AJ. Evaluation of the prognostic value of platelet to lymphocyte ratio in patients with hepatocellular carcinoma. J Gastrointest Oncol. 2017; 8:1065–1071. PMID: 29299368.
Article13. Okugawa Y, Toiyama Y, Yamamoto A, Shigemori T, Ichikawa T, Yin C, et al. Lymphocyte-to-C-reactive protein ratio and score are clinically feasible nutrition-inflammation markers of outcome in patients with gastric cancer. Clin Nutr. 2020; 39:1209–1217. PMID: 31155370.
Article14. Okugawa Y, Toiyama Y, Yamamoto A, Shigemori T, Ide S, Kitajima T, et al. Lymphocyte-C-reactive protein ratio as promising new marker for predicting surgical and oncological outcomes in colorectal cancer. Ann Surg. 2020; 272:342–351. PMID: 32675548.
Article15. Iseda N, Itoh S, Yoshizumi T, Tomiyama T, Morinaga A, Shimagaki T, et al. Lymphocyte-to-C-reactive protein ratio as a prognostic factor for hepatocellular carcinoma. Int J Clin Oncol. 2021; 26:1890–1900. PMID: 34251555.
Article16. Yugawa K, Maeda T, Kinjo N, Kawata K, Ikeda S, Edahiro K, et al. Prognostic impact of lymphocyte-C-reactive protein ratio in patients who underwent surgical resection for hepatocellular carcinoma. J Gastrointest Surg. 2022; 26:104–112. PMID: 34258673.
Article17. Zhang YF, Lu LH, Zhong C, Chen MS, Guo RP, Wang L. Prognostic value of the preoperative lymphocyte-C-reactive protein ratio in hepatocellular carcinoma patients treated with curative intent: a large-scale multicentre study. J Inflamm Res. 2021; 14:2483–2495. PMID: 34140796.
Article18. Brierley JD, Gospodarowicz MK, Wittekind C, editors. TNM classification of malignant tumours. Chichester, West Sussex, UK; Hoboken, NJ: John Wiley & Sons;2017.19. Fairclough E, Cairns E, Hamilton J, Kelly C. Evaluation of a modified early warning system for acute medical admissions and comparison with C-reactive protein/albumin ratio as a predictor of patient outcome. Clin Med (Lond). 2009; 9:30–33. PMID: 19271597.
Article20. Walsh SR, Cook EJ, Goulder F, Justin TA, Keeling NJ. Neutrophil-lymphocyte ratio as a prognostic factor in colorectal cancer. J Surg Oncol. 2005; 91:181–184. PMID: 16118772.
Article21. Templeton AJ, McNamara MG, Šeruga B, Vera-Badillo FE, Aneja P, Ocaña A, et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. J Natl Cancer Inst. 2014; 106:dju124. PMID: 24875653.
Article22. Onodera T, Goseki N, Kosaki G. Prognostic nutritional index in gastrointestinal surgery of malnourished cancer patients. Nihon Geka Gakkai Zasshi. 1984; 85:1001–1005. PMID: 6438478.23. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009; 250:187–196. PMID: 19638912.25. Cheng CB, Zhang QX, Zhuang LP, Sun JW. Prognostic value of lymphocyte-to-C-reactive protein ratio in patients with gastric cancer after surgery: a multicentre study. Jpn J Clin Oncol. 2020; 50:1141–1149. PMID: 32564084.
Article26. Kurebayashi Y, Kubota N, Sakamoto M. Immune microenvironment of hepatocellular carcinoma, intrahepatic cholangiocarcinoma and liver metastasis of colorectal adenocarcinoma: relationship with histopathological and molecular classifications. Hepatol Res. 2021; 51:5–18. PMID: 32573056.
Article27. Itoh S, Yoshizumi T, Yugawa K, Imai D, Yoshiya S, Takeishi K, et al. Impact of immune response on outcomes in hepatocellular carcinoma: association with vascular formation. Hepatology. 2020; 72:1987–1999. PMID: 32112577.
Article28. Väyrynen JP, Tuomisto A, Klintrup K, Mäkelä J, Karttunen TJ, Mäkinen MJ. Detailed analysis of inflammatory cell infiltration in colorectal cancer. Br J Cancer. 2013; 109:1839–1847. PMID: 24008661.
Article29. Nagaoka S, Yoshida T, Akiyoshi J, Akiba J, Torimura T, Adachi H, et al. Serum C-reactive protein levels predict survival in hepatocellular carcinoma. Liver Int. 2007; 27:1091–1097. PMID: 17845537.
Article30. Canna K, McArdle PA, McMillan DC, McNicol AM, Smith GW, McKee RF, et al. The relationship between tumour T-lymphocyte infiltration, the systemic inflammatory response and survival in patients undergoing curative resection for colorectal cancer. Br J Cancer. 2005; 92:651–654. PMID: 15700032.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Lymphopenia predicts reduced survival in canine hepatocellular carcinoma
- Blood Neutrophil-to-Lymphocyte Ratio Predicts Tumor Recurrence in Patients with Hepatocellular Carcinoma within Milan Criteria after Hepatectomy
- Significance of Erythrocyte Sedimentation Rate and C-reactive Protein as Predictive Factors for Prognosis in Non-metastatic Renal Cell Carcinoma
- C-reactive protein/albumin ratio as prognostic score in oral squamous cell carcinoma
- Surgical Experience for Recurrence of Hepatocellular Carcinoma