J Korean Assoc Oral Maxillofac Surg.
2022 Apr;48(2):94-100. 10.5125/jkaoms.2022.48.2.94.
Comparative effects of systemic administration of levofloxacin and cephalexin on fracture healing in rats
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Dental School, Islamic Azad University, Isfahan (Khorasgan) Branch, Isfahan, Iran.
- 2Department of Oral Pathology, Dental School, Islamic Azad University, Isfahan (Khorasgan) Branch, Isfahan, Iran.
- KMID: 2529922
- DOI: http://doi.org/10.5125/jkaoms.2022.48.2.94
Abstract
Objectives
This study aimed to compare the effects of systemic administration of levofloxacin or cephalexin on fracture healing in rats.
Materials and Methods
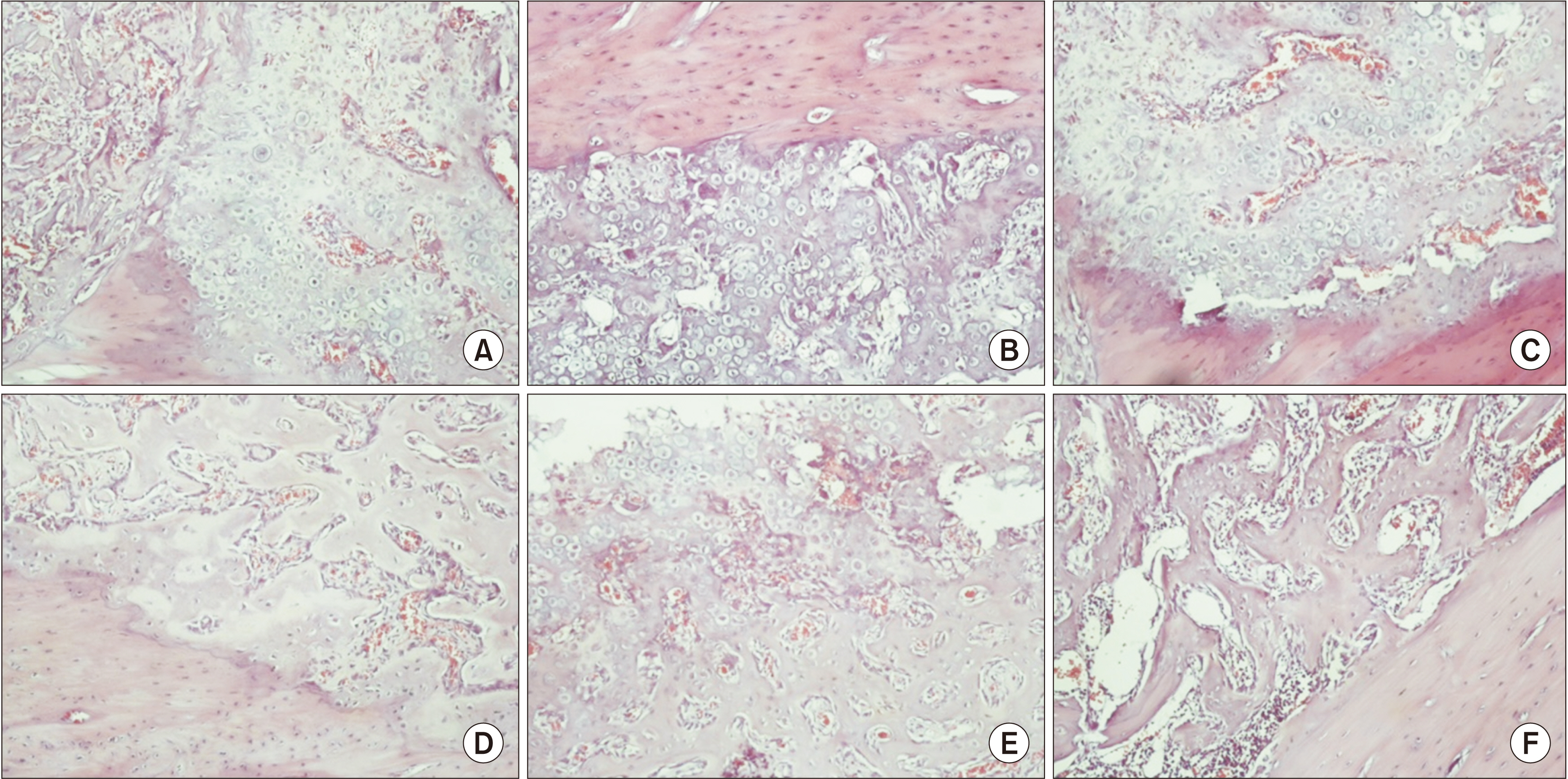
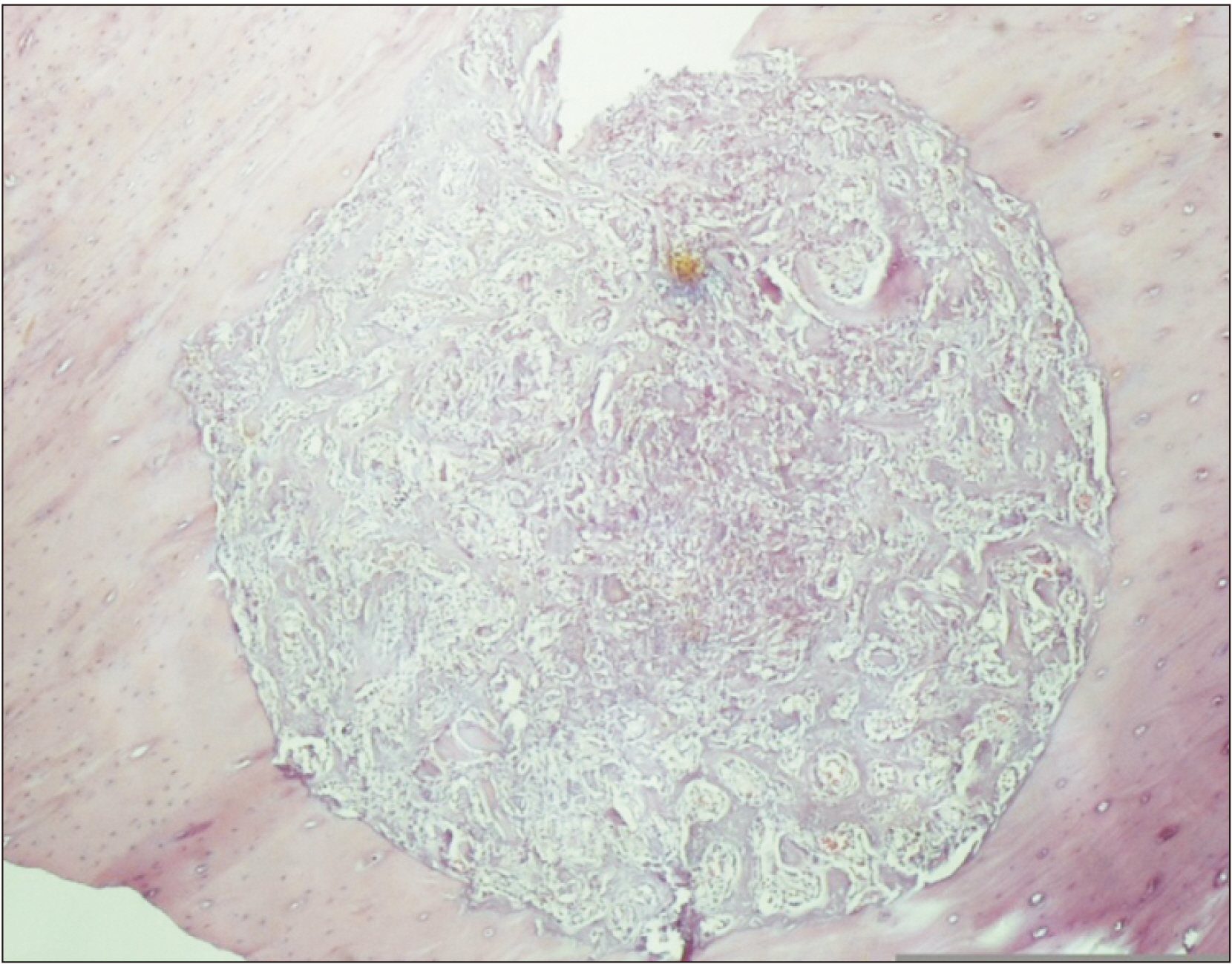
In this animal study, tibial fractures not requiring fixation were artificially induced in 30 male Wistar albino rats using a 1.1 mm surgical bur. The rats were randomly divided into 6 groups (n=5). Groups 1 and 2 received daily subcutaneous saline injections. Groups 3 and 4 received subcutaneous injections of 25 mg/kg levofloxacin twice daily. Groups 5 and 6 received daily subcutaneous injections of 20 mg/kg cephalexin. The rats in Groups 1, 3, and 5 were sacrificed after 1 week, while the rats in Groups 2, 4, and 6 were sacrificed after 4 weeks. The score of fracture healing was determined through histological assessment of sections from the fracture site according to Perry and colleagues. Data were analyzed by Kruskal–Wallis and Mann–Whitney tests.
Results
The mean score of fracture healing at 4 weeks was significantly higher than that at 1 week in the saline, levofloxacin, and cephalexin groups P<0.001). At 1 week, no significant difference was noted among the three groups of saline, levofloxacin, and cephalexin in the mean score of fracture healing (P=0.360). However, this difference was significant at 4 weeks (P=0.018), and the mean score in the saline group was significantly higher compared to that in the levofloxacin group (P=0.015).
Conclusion
It is recommended not to prescribe levofloxacin for more than 1 week after surgical management of bone fractures due to its possible adverse effects on fracture healing.
Keyword
Figure
Reference
-
References
1. Shokier H, Khalifa G, Fawzy A, Sallam MM. 2010; Experimental use of autogenous bone grafts as an alternative method for bone plates in treatment of mandibular fracture. Aust J Basic Appl Sci. 4:1466–72.2. Uçan MC, Koparal M, Ağaçayak S, Gunay A, Ozgoz M, Atilgan S, et al. 2013; Influence of caffeic acid phenethyl ester on bone healing in a rat model. J Int Med Res. 41:1648–54. https://doi.org/10.1177/0300060513490613. DOI: 10.1177/0300060513490613. PMID: 24065455.
Article3. Hausman MR, Schaffler MB, Majeska RJ. 2001; Prevention of fracture healing in rats by an inhibitor of angiogenesis. Bone. 29:560–4. https://doi.org/10.1016/s8756-3282(01)00608-1. DOI: 10.1016/S8756-3282(01)00608-1. PMID: 11728927.
Article4. Keramaris NC, Calori GM, Nikolaou VS, Schemitsch EH, Giannoudis PV. 2008; Fracture vascularity and bone healing: a systematic review of the role of VEGF. Injury. 39 Suppl 2:S45–57. https://doi.org/10.1016/S0020-1383(08)70015-9. DOI: 10.1016/S0020-1383(08)70015-9. PMID: 18804573.
Article5. Cook JJ, Summers NJ, Cook EA. 2015; Healing in the new millennium: bone stimulators: an overview of where we've been and where we may be heading. Clin Podiatr Med Surg. 32:45–59. https://doi.org/10.1016/j.cpm.2014.09.003. DOI: 10.1016/j.cpm.2014.09.003. PMID: 25440417.
Article6. MalekiGorji M, Golestaneh A, Razavi SM. 2020; The effect of two phosphodiesterase inhibitors on bone healing in mandibular fractures (animal study in rats). J Korean Assoc Oral Maxillofac Surg. 46:258–65. https://doi.org/10.5125/jkaoms.2020.46.4.258. DOI: 10.5125/jkaoms.2020.46.4.258. PMID: 32855373. PMCID: PMC7469969.
Article7. Massari L, Caruso G, Sollazzo V, Setti S. 2009; Pulsed electromagnetic fields and low intensity pulsed ultrasound in bone tissue. Clin Cases Miner Bone Metab. 6:149–54. PMID: 22461165. PMCID: PMC2781224.8. Perry AC, Prpa B, Rouse MS, Piper KE, Hanssen AD, Steckelberg JM, et al. 2003; Levofloxacin and trovafloxacin inhibition of experimental fracture-healing. Clin Orthop Relat Res. 414:95–100. https://doi.org/10.1097/01.blo.0000087322.60612.14. DOI: 10.1097/01.blo.0000087322.60612.14. PMID: 12966282.
Article9. Maxwell A. 1992; The molecular basis of quinolone action. J Antimicrob Chemother. 30:409–14. https://doi.org/10.1093/jac/30.4.409. DOI: 10.1093/jac/30.4.409. PMID: 1337067.
Article10. Rissing JP. 1997; Antimicrobial therapy for chronic osteomyelitis in adults: role of the quinolones. Clin Infect Dis. 25:1327–33. https://doi.org/10.1086/516150. DOI: 10.1086/516150. PMID: 9431371.
Article11. Davis R, Bryson HM. 1994; Levofloxacin. A review of its antibacterial activity, pharmacokinetics and therapeutic efficacy. Drugs. 47:677–700. https://doi.org/10.2165/00003495-199447040-00008. DOI: 10.2165/00003495-199447040-00008. PMID: 7516863.
Article12. Shahabadi N, Hashempour S. 2019; DNA binding studies of antibiotic drug cephalexin using spectroscopic and molecular docking techniques. Nucleosides Nucleotides Nucleic Acids. 38:428–47. https://doi.org/10.1080/15257770.2018.1562071. DOI: 10.1080/15257770.2018.1562071. PMID: 30931791.
Article13. Papich MG, Lindeman C. 2018; Cephalexin susceptibility breakpoint for veterinary isolates: Clinical Laboratory Standards Institute revision. J Vet Diagn Invest. 30:113–20. https://doi.org/10.1177/1040638717742434. DOI: 10.1177/1040638717742434. PMID: 29145786. PMCID: PMC6504153.
Article14. Huddleston PM, Steckelberg JM, Hanssen AD, Rouse MS, Bolander ME, Patel R. 2000; Ciprofloxacin inhibition of experimental fracture healing. J Bone Joint Surg Am. 82:161–73. https://doi.org/10.2106/00004623-200002000-00002. DOI: 10.2106/00004623-200002000-00002. PMID: 10682725.
Article15. Atalay Y, Gunes N, Guner MD, Akpolat V, Celik MS, Guner R. 2015; Pentoxifylline and electromagnetic field improved bone fracture healing in rats. Drug Des Devel Ther. 9:5195–201. https://doi.org/10.2147/DDDT.S89669. DOI: 10.2147/DDDT.S89669. PMID: 26388687. PMCID: PMC4571933.
Article16. Clark JD, Gebhart GF, Gonder JC, Keeling ME, Kohn DF. 1997; Special report: the 1996 guide for the care and use of laboratory animals. ILAR J. 38:41–8. https://doi.org/10.1093/ilar.38.1.41. DOI: 10.1093/ilar.38.1.41. PMID: 11528046.
Article17. Krischak GD, Augat P, Blakytny R, Claes L, Kinzl L, Beck A. 2007; The non-steroidal anti-inflammatory drug diclofenac reduces appearance of osteoblasts in bone defect healing in rats. Arch Orthop Trauma Surg. 127:453–8. https://doi.org/10.1007/s00402-007-0288-9. DOI: 10.1007/s00402-007-0288-9. PMID: 17245601.
Article18. Sitovs A, Voiko L, Kustovs D, Kovalcuka L, Bandere D, Purvina S, et al. 2020; Pharmacokinetic profiles of levofloxacin after intravenous, intramuscular and subcutaneous administration to rabbits (Oryctolagus cuniculus). J Vet Sci. 21:e32. https://doi.org/10.4142/jvs.2020.21.e32. DOI: 10.4142/jvs.2020.21.e32. PMID: 32233138. PMCID: PMC7113567.
Article19. Williams BH. 2000; Therapeutics in ferrets. Vet Clin North Am Exot Anim Pract. 3:131–53. vihttps://doi.org/10.1016/s1094-9194(17)30098-1. DOI: 10.1016/S1094-9194(17)30098-1. PMID: 11228824. PMCID: PMC7110454.
Article20. Hernandez RK, Do TP, Critchlow CW, Dent RE, Jick SS. 2012; Patient-related risk factors for fracture-healing complications in the United Kingdom General Practice Research Database. Acta Orthop. 83:653–60. https://doi.org/10.3109/17453674.2012.747054. DOI: 10.3109/17453674.2012.747054. PMID: 23140093. PMCID: PMC3555441.
Article21. Bratzler DW, Dellinger EP, Olsen KM, Perl TM, Auwaerter PG, Bolon MK, et al. 2013; ; American Society of Health-System Pharmacists (ASHP); Infectious Diseases Society of America (IDSA); Surgical Infection Society (SIS); Society for Healthcare Epidemiology of America (SHEA). Clinical practice guidelines for antimicrobial prophylaxis in surgery. Surg Infect (Larchmt). 14:73–156. https://doi.org/10.1089/sur.2013.9999. DOI: 10.1089/sur.2013.9999. PMID: 23461695.
Article22. Pountos I, Georgouli T, Bird H, Kontakis G, Giannoudis PV. 2011; The effect of antibiotics on bone healing: current evidence. Expert Opin Drug Saf. 10:935–45. https://doi.org/10.1517/14740338.2011.589833. DOI: 10.1517/14740338.2011.589833. PMID: 21824037.
Article23. Kallala R, Graham SM, Nikkhah D, Kyrkos M, Heliotis M, Mantalaris A, et al. 2012; In vitro and in vivo effects of antibiotics on bone cell metabolism and fracture healing. Expert Opin Drug Saf. 11:15–32. https://doi.org/10.1517/14740338.2012.643867. DOI: 10.1517/14740338.2012.643867. PMID: 22149454.
Article24. Holtom PD, Pavkovic SA, Bravos PD, Patzakis MJ, Shepherd LE, Frenkel B. 2000; Inhibitory effects of the quinolone antibiotics trovafloxacin, ciprofloxacin, and levofloxacin on osteoblastic cells in vitro. J Orthop Res. 18:721–7. https://doi.org/10.1002/jor.1100180507. DOI: 10.1002/jor.1100180507. PMID: 11117292.
Article25. Salzmann GM, Naal FD, von Knoch F, Tuebel J, Gradinger R, Imhoff AB, et al. 2007; Effects of cefuroxime on human osteoblasts in vitro. J Biomed Mater Res A. 82:462–8. https://doi.org/10.1002/jbm.a.31158. DOI: 10.1002/jbm.a.31158. PMID: 17295250.
Article26. Edin ML, Miclau T, Lester GE, Lindsey RW, Dahners LE. 1996; Effect of cefazolin and vancomycin on osteoblasts in vitro. Clin Orthop Relat Res. 333:245–51. DOI: 10.1097/00003086-199612000-00027. PMID: 8981903.
Article27. Brown SA. 1996; Fluoroquinolones in animal health. J Vet Pharmacol Ther. 19:1–14. https://doi.org/10.1111/j.1365-2885.1996.tb00001.x. DOI: 10.1111/j.1365-2885.1996.tb00001.x. PMID: 8992019.
Article28. Martinez M, McDermott P, Walker R. 2006; Pharmacology of the fluoroquinolones: a perspective for the use in domestic animals. Vet J. 172:10–28. https://doi.org/10.1016/j.tvjl.2005.07.010. DOI: 10.1016/j.tvjl.2005.07.010. PMID: 16154368.
Article29. Förster C, Kociok K, Shakibaei M, Merker HJ, Stahlmann R. 1996; Quinolone-induced cartilage lesions are not reversible in rats. Arch Toxicol. 70:474–81. https://doi.org/10.1007/s002040050301. DOI: 10.1007/s002040050301. PMID: 8783810.
Article30. Gough A, Johnson R, Campbell E, Hall L, Tylor J, Carpenter A, et al. 1996; Quinolone arthropathy in immature rabbits treated with the fluoroquinolone, PD 117596. Exp Toxicol Pathol. 48:225–32. https://doi.org/10.1016/S0940-2993(96)80003-0. DOI: 10.1016/S0940-2993(96)80003-0. PMID: 8811288.
Article31. Kato M, Takada S, Ogawara S, Takayama S. 1995; Effect of levofloxacin on glycosaminoglycan and DNA synthesis of cultured rabbit chondrocytes at concentrations inducing cartilage lesions in vivo. Antimicrob Agents Chemother. 39:1979–83. https://doi.org/10.1128/AAC.39.9.1979. DOI: 10.1128/AAC.39.9.1979. PMID: 8540702. PMCID: PMC162867.
Article32. Linseman DA, Hampton LA, Branstetter DG. 1995; Quinolone-induced arthropathy in the neonatal mouse. Morphological analysis of articular lesions produced by pipemidic acid and ciprofloxacin. Fundam Appl Toxicol. 28:59–64. https://doi.org/10.1006/faat.1995.1146. DOI: 10.1006/faat.1995.1146. PMID: 8566484.
Article33. Shakibaei M, Kociok K, Förster C, Vormann J, Günther T, Stahlmann R, et al. 1996; Comparative evaluation of ultrastructural changes in articular cartilage of ofloxacin-treated and magnesium-deficient immature rats. Toxicol Pathol. 24:580–7. https://doi.org/10.1177/019262339602400507. DOI: 10.1177/019262339602400507. PMID: 8923679.
Article34. Egerbacher M, Edinger J, Tschulenk W. 2001; Effects of enrofloxacin and ciprofloxacin hydrochloride on canine and equine chondrocytes in culture. Am J Vet Res. 62:704–8. https://doi.org/10.2460/ajvr.2001.62.704. DOI: 10.2460/ajvr.2001.62.704. PMID: 11341389.
Article35. Egerbacher M, Seiberl G, Wolfesberger B, Walter I. 2000; Ciprofloxacin causes cytoskeletal changes and detachment of human and rat chondrocytes in vitro. Arch Toxicol. 73:557–63. https://doi.org/10.1007/s002040050008. DOI: 10.1007/s002040050008. PMID: 10663387.
Article36. Stahlmann R, Schwabe R. 1997; Safety profile of grepafloxacin compared with other fluoroquinolones. J Antimicrob Chemother. 40 Suppl A:83–92. https://doi.org/10.1093/jac/40.suppl_1.83. DOI: 10.1093/jac/40.suppl_1.83. PMID: 9484877.
Article37. Förster C, Rücker M, Shakibaei M, Baumann-Wilschke I, Vormann J, Stahlmann R. 1998; Effects of fluoroquinolones and magnesium deficiency in murine limb bud cultures. Arch Toxicol. 72:411–9. https://doi.org/10.1007/s002040050521. DOI: 10.1007/s002040050521. PMID: 9708880.
Article38. Menschik M, Neumüller J, Steiner CW, Erlacher L, Köller M, Ullrich R, et al. 1997; Effects of ciprofloxacin and ofloxacin on adult human cartilage in vitro. Antimicrob Agents Chemother. 41:2562–5. https://doi.org/10.1128/AAC.41.11.2562. DOI: 10.1128/AAC.41.11.2562. PMID: 9371369. PMCID: PMC164164.
Article39. Long F, Ornitz DM. 2013; Development of the endochondral skeleton. Cold Spring Harb Perspect Biol. 5:a008334. https://doi.org/10.1101/cshperspect.a008334. DOI: 10.1101/cshperspect.a008334. PMID: 23284041. PMCID: PMC3579395.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clostridium difficile Colitis after Topical Ophthalmic Use of Levofloxacin
- The Effect of COX-2 Inhibitor on the Expression of MMP-13 during Early Fracture Healing Phase in Rats
- The Effect of Distraction - Compression on the Fracture Healing in Rats with Osteoporosis
- Studies on the Antivacterial Effect of Cephalosporin Derivatives
- Effect of Teriparatide on Healing of Atypical Femoral Fractures: A Systemic Review