J Yeungnam Med Sci.
2022 Jan;39(1):39-45. 10.12701/yujm.2021.01207.
Clinical investigation on acute pyelonephritis without pyuria: a retrospective observational study
- Affiliations
-
- 1Department of Emergency Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2525026
- DOI: http://doi.org/10.12701/yujm.2021.01207
Abstract
- Background
The current guidelines for the diagnosis of acute pyelonephritis (APN) recommend that APN be diagnosed based on the clinical features and the presence of pyuria. However, we observed that some of the patients who are diagnosed with APN do not have characteristic clinical features or pyuria at the initial examination. We performed this study to investigate the characteristics of APN without pyuria.
Methods
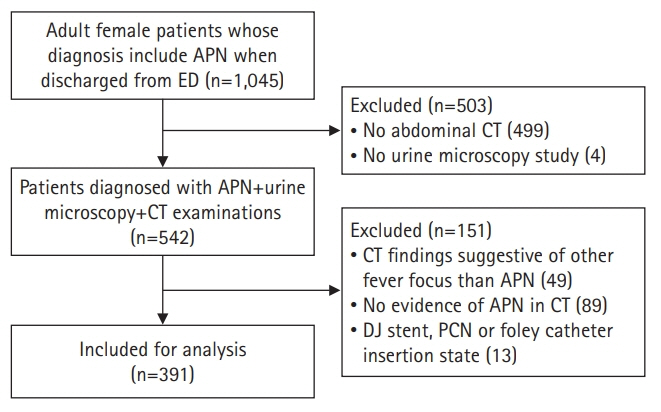
A retrospective, cross-sectional study was conducted on 391 patients diagnosed with APN based on clinical and radiologic findings, between 2015 and 2019. The clinical features, laboratory results, and computed tomography (CT) findings were compared between patients with normal white blood cell (WBC) counts and those with abnormal WBC counts (WBC of 0–5/high power field [HPF] vs. >5/HPF) in urine.
Results
More than 50% of patients with APN had no typical urinary tract symptoms and one-third of them had no costovertebral angle (CVA) tenderness. Eighty-eight patients (22.5%) had normal WBC counts (0–5/HPF) on urine microscopy. There was a negative correlation between pyuria (WBC of >5/HPF) and previous antibiotic use (odds ratio, 0.249; 95% confidence interval, 0.140–0.441; p<0.001), and the probability of pyuria was reduced by 75.1% in patients who took antibiotics before visiting the emergency room.
Conclusion
The diagnosis of APN should not be overlooked even if there are no typical clinical features, or urine microscopic examination is normal. If a patient has already taken antibiotics at the time of diagnosis, imaging studies such as CT should be performed more actively, regardless of the urinalysis results.
Figure
Reference
-
References
1. Gupta K, Hooton TM, Naber KG, Wullt B, Colgan R, Miller LG, et al. International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: a 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clin Infect Dis. 2011; 52:e103–20.2. Kang CI, Kim J, Park DW, Kim BN, Ha US, Lee SJ, et al. Clinical practice guidelines for the antibiotic treatment of community: acquired urinary tract infections. Infect Chemother. 2018; 50:67–100.3. Matthews SJ, Lancaster JW. Urinary tract infections in the elderly population. Am J Geriatr Pharmacother. 2011; 9:286–309.4. Woodford HJ, George J. Diagnosis and management of urinary infections in older people. Clin Med (Lond). 2011; 11:80–3.5. Stamm WE. Measurement of pyuria and its relation to bacteriuria. Am J Med. 1983; 75(1B):53–8.6. Colgan R, Williams M, Johnson JR. Diagnosis and treatment of acute pyelonephritis in women. Am Fam Physician. 2011; 84:519–26.7. Pietrucha-Dilanchian P, Hooton TM. Diagnosis, treatment, and prevention of urinary tract infection. Microbiol Spectr. 2016; 4(6):10.1128/microbiolspec.UTI-0021-2015.8. Rollino C, Beltrame G, Ferro M, Quattrocchio G, Sandrone M, Quarello F. Acute pyelonephritis in adults: a case series of 223 patients. Nephrol Dial Transplant. 2012; 27:3488–93.9. Ifergan J, Pommier R, Brion MC, Glas L, Rocher L, Bellin MF. Imaging in upper urinary tract infections. Diagn Interv Imaging. 2012; 93:509–19.10. Lee A, Kim HC, Hwang SI, Chin HJ, Na KY, Chae DW, et al. Clinical usefulness of unenhanced computed tomography in patients with acute pyelonephritis. J Korean Med Sci. 2018; 33:e236.11. Flores-Mireles AL, Walker JN, Caparon M, Hultgren SJ. Urinary tract infections: epidemiology, mechanisms of infection and treatment options. Nat Rev Microbiol. 2015; 13:269–84.12. McLellan LK, Hunstad DA. Urinary tract infection: pathogenesis and outlook. Trends Mol Med. 2016; 22:946–57.13. Expert Panel on Urologic Imaging; Nikolaidis P, Dogra VS, Goldfarb S, Gore JL, Harvin HJ, et al. ACR Appropriateness Criteria® acute pyelonephritis. J Am Coll Radiol. 2018; 15(11 Suppl):S232–9.14. Meng MV, Mario LA, McAninch JW. Current treatment and outcomes of perinephric abscesses. J Urol. 2002; 168(4 Pt 1):1337–40.15. Aboumarzouk OM, Hughes O, Narahari K, Coulthard R, Kynaston H, Chlosta P, et al. Emphysematous pyelonephritis: time for a management plan with an evidence-based approach. Arab J Urol. 2014; 12:106–15.16. Ramsey S, Robertson A, Ablett MJ, Meddings RN, Hollins GW, Little B. Evidence-based drainage of infected hydronephrosis secondary to ureteric calculi. J Endourol. 2010; 24:185–9.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Urinary Transforming Growth Factor-beta1 (TGF-beta1)/Creatinine Ratio and Its Clinical Implications in Childhood Acute Pyelonephritis
- The Nitroblue-tetrazlium dye Reduction Test in Urinary Tract Infections
- Clinical Characteristics of Acute Pyelonephritis in Spinal Cord Injury Patient
- A Case of Xanthogranulomatous Pyelonephritis
- A Clinical Study on the Patients with Pyuria