Clin Endosc.
2021 Nov;54(6):888-898. 10.5946/ce.2020.271.
Endoscopic Interventions for the Early and Remission Phases of Acute Biliary Pancreatitis: What are the More Concrete and Practical Situations for Performing Them?
- Affiliations
-
- 1Department of Gastroenterology, Sendai City Medical Center, Sendai, Japan
- 2Department of Gastroenterology and Hepatology, Yokohama City University School of Medicine, Yokohama, Japan
- KMID: 2522710
- DOI: http://doi.org/10.5946/ce.2020.271
Abstract
- Background/Aims
The use of endoscopic intervention (EI) for acute biliary pancreatitis (ABP) remains controversial because the severity of biliary obstruction/cholangitis/pancreatitis is not reflected in the indications for early EI (EEI).
Methods
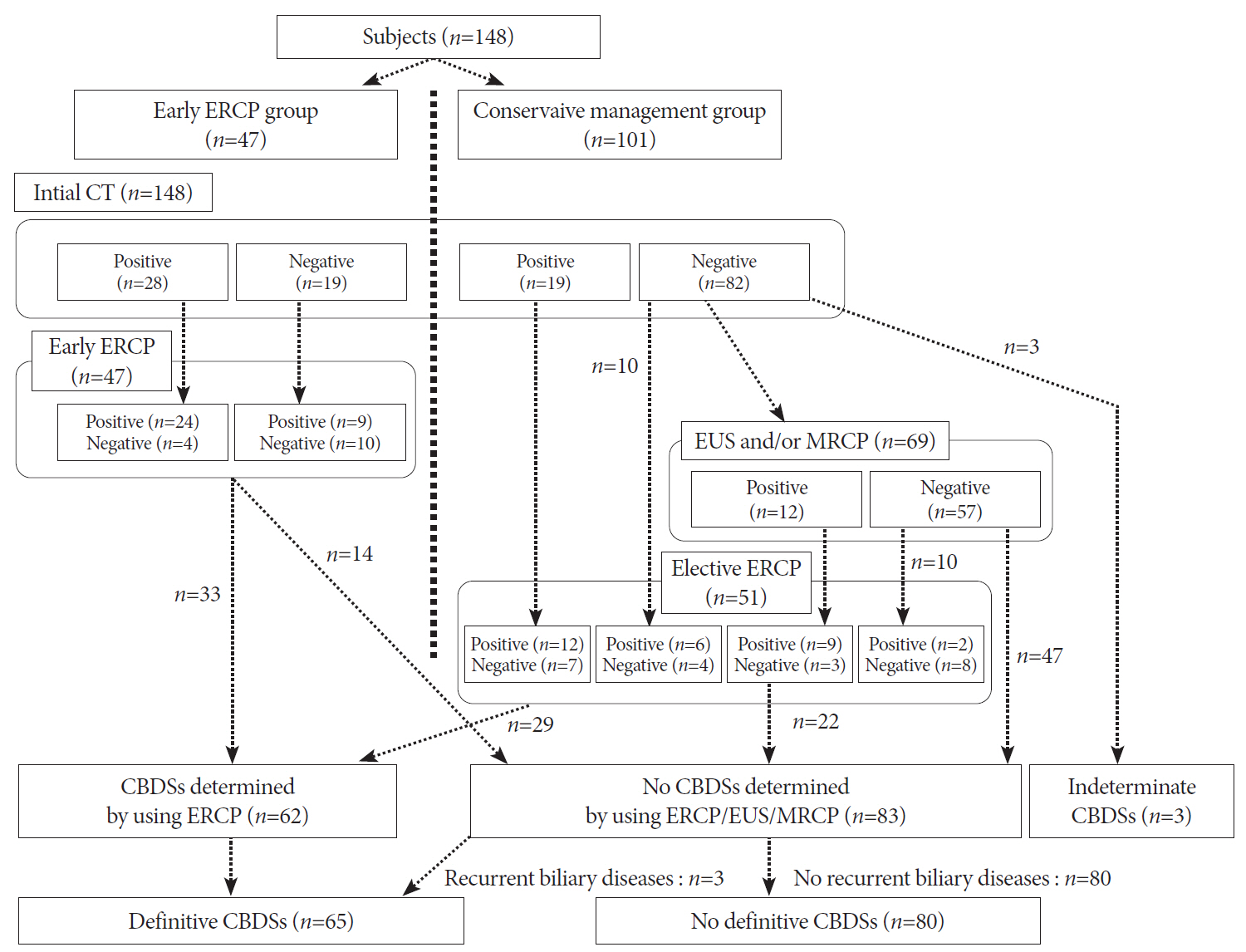
A total of 148 patients with ABP were included to investigate 1) the differences in the rate of worsening cholangitis/pancreatitis between the EEI group and the early conservative management (ECM) group, especially for each severity of cholangitis/pancreatitis, and 2) the diagnostic ability of imaging studies, including endoscopic ultrasound (EUS), to detect common bile duct stones (CBDSs) in the ECM group.
Results
No differences were observed in the rate of worsening cholangitis between the EEI and ECM groups, regardless of the severity of cholangitis and/or the existence of impacted CBDSs. Among patients without impacted CBDSs and moderate/severe cholangitis, worsening pancreatitis was significantly more frequent in the EEI group (18% vs. 4%, p=0.048). In patients in the ECM group, the sensitivity and specificity for detecting CBDSs were 73% and 98%, respectively, for EUS, whereas the values were 13% and 92%, respectively, for magnetic resonance cholangiopancreatography.
Conclusions
EEI should be avoided in the absence of moderate/severe cholangitis and/or impacted CBDSs because of the high rate of worsening pancreatitis. EUS can contribute to the accurate detection of residual CBDSs, for the determination of the need for elective EI.
Keyword
Figure
Reference
-
1. Maple JT, Ben-Menachem T, Anderson MA, et al. The role of endoscopy in the evaluation of suspected choledocholithiasis. Gastrointest Endosc. 2010; 71:1–9.
Article2. Anderloni A, Galeazzi M, Ballare M, et al. Early endoscopic ultrasonography in acute biliary pancreatitis: a prospective pilot study. World J Gastroenterol. 2015; 21:10427–10434.
Article3. Yokoe M, Takada T, Mayumi T, et al. Japanese guidelines for the management of acute pancreatitis: Japanese guidelines 2015. J Hepatobiliary Pancreat Sci. 2015; 22:405–432.
Article4. ASGE Standards of Practice committee, Buxbaum JL, Abbas Fehmi SM, et al. ASGE guideline on the role of endoscopy in the evaluation and management of choledocholithiasis. Gastrointest Endosc. 2019; 89:1075–1105.
Article5. Williams E, Beckingham I, El Sayed G, Gurusamy K, Webster G, Young T. Updated guideline on the management of common bile duct stones (CBDS). Gut. 2017; 66:765–782.
Article6. Tse F, Yuan Y. Early routine endoscopic retrograde cholangiopancreatography strategy versus early conservative management strategy in acute gallstone pancreatitis. Cochrane Database Syst Rev. 2012; (5):CD009779.
Article7. Kimura Y, Arata S, Takada T, et al. Gallstone-induced acute pancreatitis. J Hepatobiliary Pancreat Sci. 2010; 17:60–69.
Article8. Kiriyama S, Takada T, Strasberg SM, et al. TG13 guidelines for diagnosis and severity grading of acute cholangitis. J Hepatobiliary Pancreat Sci. 2013; 20:24–34.9. Kiriyama S, Kozaka K, Takada T, et al. Tokyo guidelines 2018: diagnostic criteria and severity grading of acute cholangitis. J Hepatobiliary Pancreat Sci. 2018; 25:17–30.10. Acosta JM, Katkhouda N, Debian KA, Groshen SG, Tsao-Wei DD, Berne TV. Early ductal decompression versus conservative management for gallstone pancreatitis with ampullary obstruction: a prospective randomized clinical trial. Ann Surg. 2006; 243:33–40.11. Schepers NJ, Hallensleben NDL, Besselink MG, et al. Urgent endoscopic retrograde cholangiopancreatography with sphincterotomy versus conservative treatment in predicted severe acute gallstone pancreatitis (APEC): a multicentre randomised controlled trial. Lancet. 2020; 396:167–176.12. Verma D, Kapadia A, Eisen GM, Adler DG. EUS vs MRCP for detection of choledocholithiasis. Gastrointest Endosc. 2006; 64:248–254.
Article13. Kondo S, Isayama H, Akahane M, et al. Detection of common bile duct stones: comparison between endoscopic ultrasonography, magnetic resonance cholangiography, and helical-computed-tomographic cholangiography. Eur J Radiol. 2005; 54:271–275.
Article14. Sugiyama M, Atomi Y. Endoscopic ultrasonography for diagnosing choledocholithiasis: a prospective comparative study with ultrasonography and computed tomography. Gastrointest Endosc. 1997; 45:143–146.
Article15. Meeralam Y, Al-Shammari K, Yaghoobi M. Diagnostic accuracy of EUS compared with MRCP in detecting choledocholithiasis: a meta-analysis of diagnostic test accuracy in head-to-head studies. Gastrointest Endosc. 2017; 86:986–993.
Article16. Liu CL, Fan ST, Lo CM, et al. Comparison of early endoscopic ultrasonography and endoscopic retrograde cholangiopancreatography in the management of acute biliary pancreatitis: a prospective randomized study. Clin Gastroenterol Hepatol. 2005; 3:1238–1244.
Article17. Lee SL, Kim HK, Choi HH, et al. Diagnostic value of magnetic resonance cholangiopancreatography to detect bile duct stones in acute biliary pancreatitis. Pancreatology. 2018; 18:22–28.
Article18. Cavdar F, Yildar M, Tellioğlu G, Kara M, Tilki M, Titiz Mİ. Controversial issues in biliary pancreatitis: when should we perform MRCP and ERCP? Pancreatology. 2014; 14:411–414.
Article19. Endo T, Ito K, Fujita N, et al. Intraductal ultrasonography in the diagnosis of bile duct stones: when and whom? Dig Endosc. 2011; 23:173–175.
Article20. Moon JH, Cho YD, Cha SW, et al. The detection of bile duct stones in suspected biliary pancreatitis: comparison of MRCP, ERCP, and intraductal US. Am J Gastroenterol. 2005; 100:1051–1057.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Indications and Timing of ERCP and Cholecystectomy for Biliary Pancreatitis
- Assessment of Severity and Fluid Administration in Acute Pancreatitis
- Medical Management of Acute Pancreatitis and Complications
- Utility of Early CT in Patients with Suspected Acute Biliary Pancreatitis
- Evaluation of Recurrent or Idiopathic Pancreatitis