J Korean Soc Radiol.
2019 Jul;80(4):704-716. 10.3348/jksr.2019.80.4.704.
Utility of Early CT in Patients with Suspected Acute Biliary Pancreatitis
- Affiliations
-
- 1Department of Radiology, Gil Medical Center, Gachon University College of Medicine, Incheon, Korea. nnoleeter@naver.com
- 2Department of Internal Medicine, Gil Medical Center, Gachon University College of Medicine, Incheon, Korea.
- KMID: 2457448
- DOI: http://doi.org/10.3348/jksr.2019.80.4.704
Abstract
- PURPOSE
The purpose of this study was to investigate whether early CT scans are useful for improving the clinical management of acute biliary pancreatitis.
MATERIALS AND METHODS
We retrospectively reviewed 56 consecutive patients who experienced first attack of acute pancreatitis and underwent CT scans within 48 hours of symptom onset in the emergency department, between March 2015 and March 2016. CT images were retrospectively evaluated for absence or presence, and etiology of acute pancreatitis, and probability of biliary pancreatitis. Urgent procedures for acute pancreatitis were analyzed.
RESULTS
Of 56 patients, 54 (96.4%) showed acute pancreatitis and 23 (41.1%) had biliary pancreatitis on CT. The diagnostic accuracy, sensitivity, and specificity of CT-diagnosed biliary pancreatitis were 94.6% (53/56), 91.7% (22/24), and 96.9% (31/32), respectively. Of the 56 patients, 17 (30.4%) patients with biliary pancreatitis underwent urgent endoscopic retrograde cholangiopancreatography (ERCP) within 72 hours (mean time interval between CT and ERCP: 25.5 ± 19.8 hours; range: 2-67 hours). There was a significant difference in the urgent procedures between non-biliary and biliary pancreatitis groups (0 of 32 vs. 17 of 24, p < 0.001).
CONCLUSION
Early CT may be used in patients visiting hospital with suspected acute biliary pancreatitis to facilitate urgent treatment.
MeSH Terms
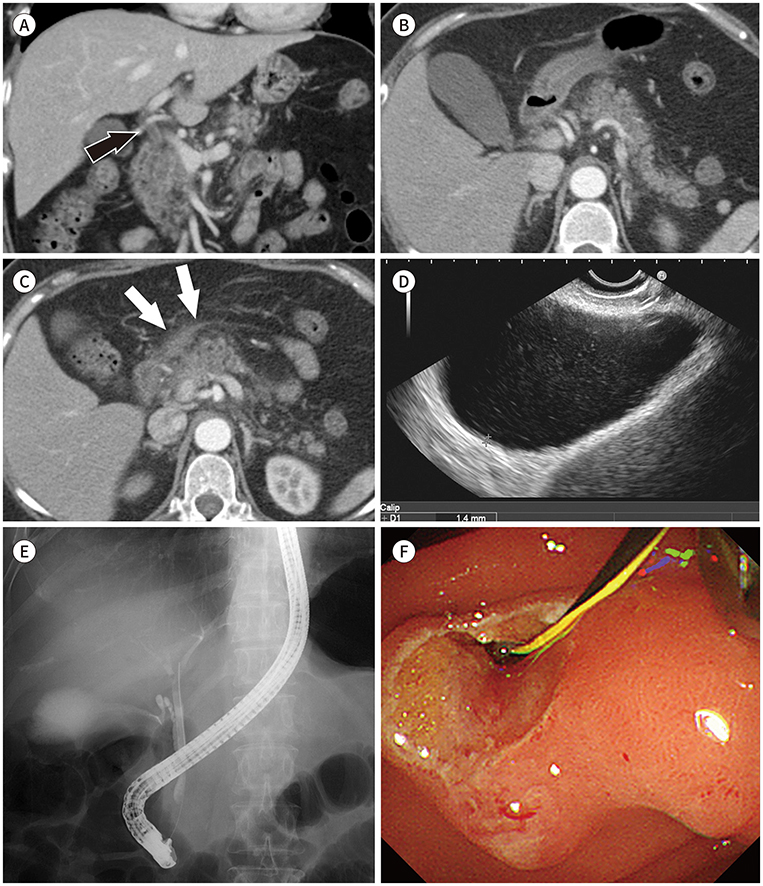
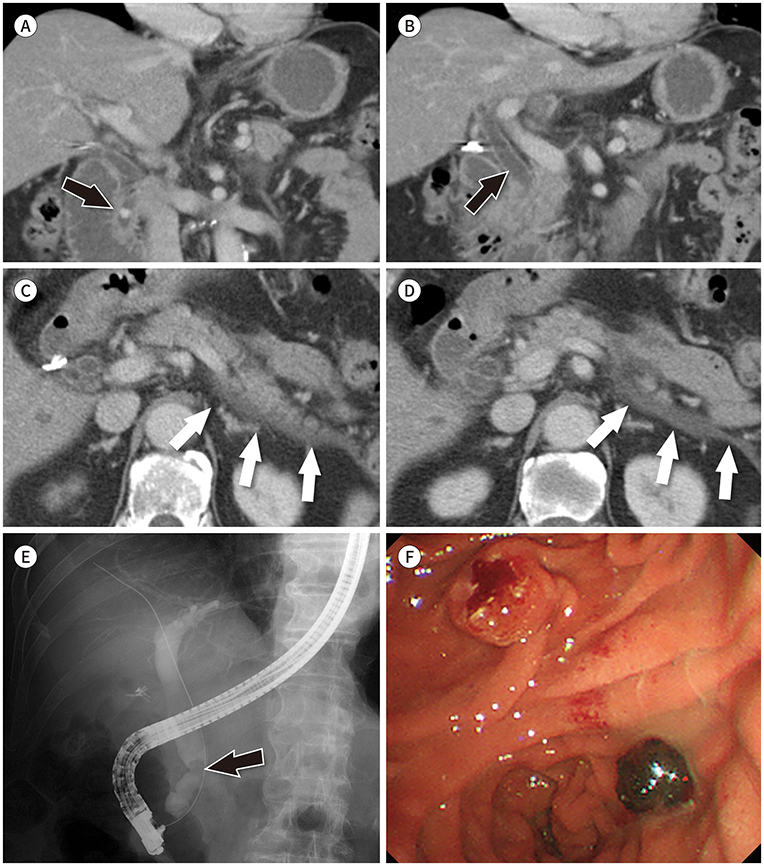
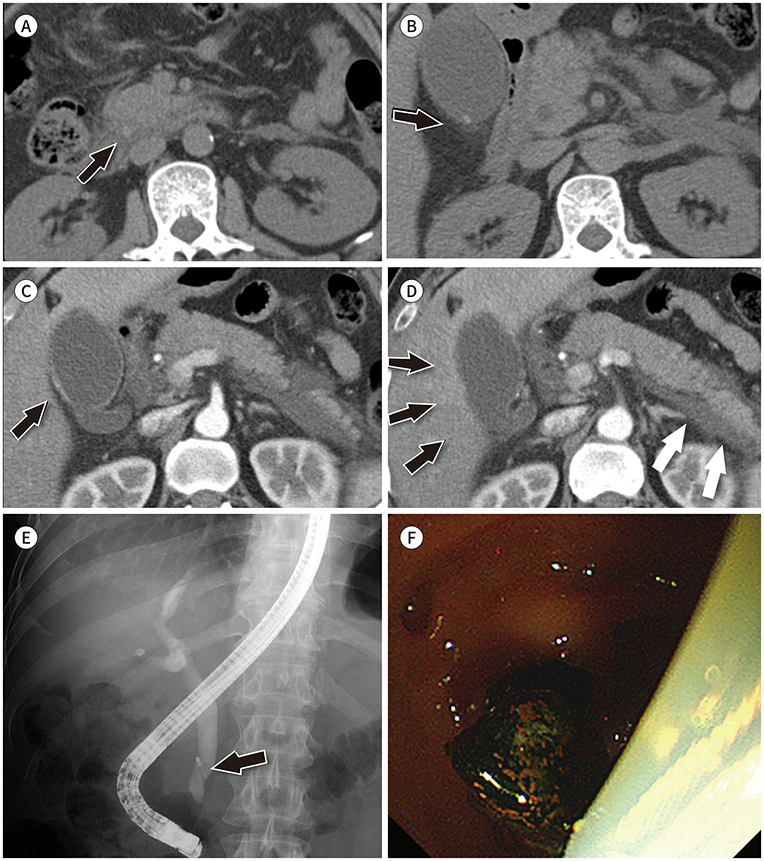
Figure
Reference
-
1. Peery AF, Dellon ES, Lund J, Crockett SD, McGowan CE, Bulsiewicz WJ, et al. Burden of gastrointestinal disease in the United States: 2012 update. Gastroenterology. 2012; 143:1179–1187.e3.
Article2. Fagenholz PJ, Fernández-del Castillo C, Harris NS, Pelletier AJ, Camargo CA Jr. National study of United States emergency department visits for acute pancreatitis, 1993-2003. BMC Emerg Med. 2007; 7:1.
Article3. Yadav D, Lowenfels AB. Trends in the epidemiology of the first attack of acute pancreatitis: a systematic review. Pancreas. 2006; 33:323–330.4. Yadav D, Lowenfels AB. The epidemiology of pancreatitis and pancreatic cancer. Gastroenterology. 2013; 144:1252–1261.
Article5. Cervellin G, Mora R, Ticinesi A, Meschi T, Comelli I, Catena F, et al. Epidemiology and outcomes of acute abdominal pain in a large urban Emergency Department: retrospective analysis of 5340 cases. Ann Transl Med. 2016; 4:362.
Article6. Caporale N, Morselli-Labate AM, Nardi E, Cogliandro R, Cavazza M, Stanghellini V. Acute abdominal pain in the emergency department of a university hospital in Italy. United European Gastroenterol J. 2016; 4:297–304.
Article7. Kocher KE, Meurer WJ, Fazel R, Scott PA, Krumholz HM, Nallamothu BK. National trends in use of computed tomography in the emergency department. Ann Emerg Med. 2011; 58:452–462.e3.
Article8. Banks PA, Bollen TL, Dervenis C, Gooszen HG, Johnson CD, Sarr MG, et al. Classification of acute pancreatitis--2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2013; 62:102–111.
Article9. Tenner S, Baillie J, DeWitt J, Vege SS. American College of Gastroenterology guideline: management of acute pancreatitis. Am J Gastroenterol. 2013; 108:1400–1415.
Article10. Balthazar EJ. Acute pancreatitis: assessment of severity with clinical and CT evaluation. Radiology. 2002; 223:603–613.
Article11. Balthazar EJ, Robinson DL, Megibow AJ, Ranson JH. Acute pancreatitis: value of CT in establishing prognosis. Radiology. 1990; 174:331–336.
Article12. Dachs RJ, Sullivan L, Shanmugathasan P. Does early ED CT scanning of afebrile patients with first episodes of acute pancreatitis ever change management? Emerg Radiol. 2015; 22:239–243.
Article13. Mortele KJ, Ip IK, Wu BU, Conwell DL, Banks PA, Khorasani R. Acute pancreatitis: imaging utilization practices in an urban teaching hospital--analysis of trends with assessment of independent predictors in correlation with patient outcomes. Radiology. 2011; 258:174–181.
Article14. Koo BC, Chinogureyi A, Shaw AS. Imaging acute pancreatitis. Br J Radiol. 2010; 83:104–112.
Article15. Casas JD, Díaz R, Valderas G, Mariscal A, Cuadras P. Prognostic value of CT in the early assessment of patients with acute pancreatitis. AJR Am J Roentgenol. 2004; 182:569–574.
Article16. Whitcomb DC. Clinical practice. Acute Pancreatitis. N Engl J Med. 2006; 354:2142–2150.17. Attasaranya S, Fogel EL, Lehman GA. Choledocholithiasis, ascending cholangitis, and gallstone pancreatitis. Med Clin North Am. 2008; 92:925–960.
Article18. Hazem ZM. Acute biliary pancreatitis: diagnosis and treatment. Saudi J Gastroenterol. 2009; 15:147–155.
Article19. O'Connor OJ, McWilliams S, Maher MM. Imaging of acute pancreatitis. AJR Am J Roentgenol. 2011; 197:W221–W225.20. Kim CD. Current status of acute pancreatitis in Korea. Korean J Gastroenterol. 2003; 42:1–11.21. Roberts SE, Akbari A, Thorne K, Atkinson M, Evans PA. The incidence of acute pancreatitis: impact of social deprivation, alcohol consumption, seasonal and demographic factors. Aliment Pharmacol Ther. 2013; 38:539–548.
Article22. Chang L, Lo SK, Stabile BE, Lewis RJ, De Virgilio C. Gallstone pancreatitis: a prospective study on the incidence of cholangitis and clinical predictors of retained common bile duct stones. Am J Gastroenterol. 1998; 93:527–531.
Article23. Chan T, Yaghoubian A, Rosing D, Lee E, Lewis RJ, Stabile BE, et al. Total bilirubin is a useful predictor of persisting common bile duct stone in gallstone pancreatitis. Am Surg. 2008; 74:977–980.
Article24. Roston AD, Jacobson IM. Evaluation of the pattern of liver tests and yield of cholangiography in symptomatic choledocholithiasis: a prospective study. Gastrointest Endosc. 1997; 45:394–399.
Article25. Cabada Giadás T, Sarría Octavio de Toledo L, Martínez-Berganza Asensio MT, Cozcolluela Cabrejas R, Alberdi Ibáñez I, Alvarez López A, et al. Helical CT cholangiography in the evaluation of the biliary tract: application to the diagnosis of choledocholithiasis. Abdom Imaging. 2002; 27:61–70.
Article26. Jiménez Cuenca I, Del Olmo Martínez L, Pérez Homs M. Helical CT without contrast in choledocholithiasis diagnosis. Eur Radiol. 2001; 11:197–201.
Article27. Takahashi M, Saida Y, Itai Y, Gunji N, Orii K, Watanabe Y. Reevaluation of spiral CT cholangiography: basic considerations and reliability for detecting choledocholithiasis in 80 patients. J Comput Assist Tomogr. 2000; 24:859–865.
Article28. Frakes JT. Biliary pancreatitis: a review. Emphasizing appropriate endoscopic intervention. J Clin Gastroenterol. 1999; 28:97–109.29. Carr-Locke DL. Biliary pancreatitis. Can J Gastroenterol. 2003; 17:205–208.
Article30. Neoptolemos JP, Carr-Locke DL, London NJ, Bailey IA, James D, Fossard DP. Controlled trial of urgent endoscopic retrograde cholangiopancreatography and endoscopic sphincterotomy versus conservative treatment for acute pancreatitis due to gallstones. Lancet. 1988; 2:979–983.
Article31. Forsmark CE, Baillie J; AGA Institute Clinical Practice and Economics Committee; AGA Institute Governing Board. AGA Institute technical review on acute pancreatitis. Gastroenterology. 2007; 132:2022–2044.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Revised Clinical Practice Guideline of Korean Pancreatobiliary Association for Acute Pancreatitis: Diagnosis
- Indications and Timing of ERCP and Cholecystectomy for Biliary Pancreatitis
- Assessment of Severity and Fluid Administration in Acute Pancreatitis
- Ceftriaxone-Induced Acute Pancreatitis in Patient with Liver Abscess
- Necrotizing Pancreatitis with Gas Gangrene