Korean J Schizophr Res.
2021 Oct;24(2):60-67. 10.16946/kjsr.2021.24.2.60.
Association of the First Antipsychotic Treatment Duration With the Re-Initiation of Treatment in Schizophrenia: A National Health Insurance Data-Based Study
- Affiliations
-
- 1Department of Psychiatry, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2522032
- DOI: http://doi.org/10.16946/kjsr.2021.24.2.60
Abstract
Objectives
The optimal duration of maintenance treatment for patients with first-episode schizophrenia (FES) remains unclear. We examined the first antipsychotic treatment duration and its association with re-initiation of treatment using a nationwide claim database.
Methods
Data from the Health Insurance Review and Assessment Service database in South Korea for 2007–2016 were used. Linear regression analysis and Cox proportional hazard models were used to evaluate the associations between the duration of the first antipsychotic treatment, time to re-initiation of treatment, and occurrence of treatment re-initiation.
Results
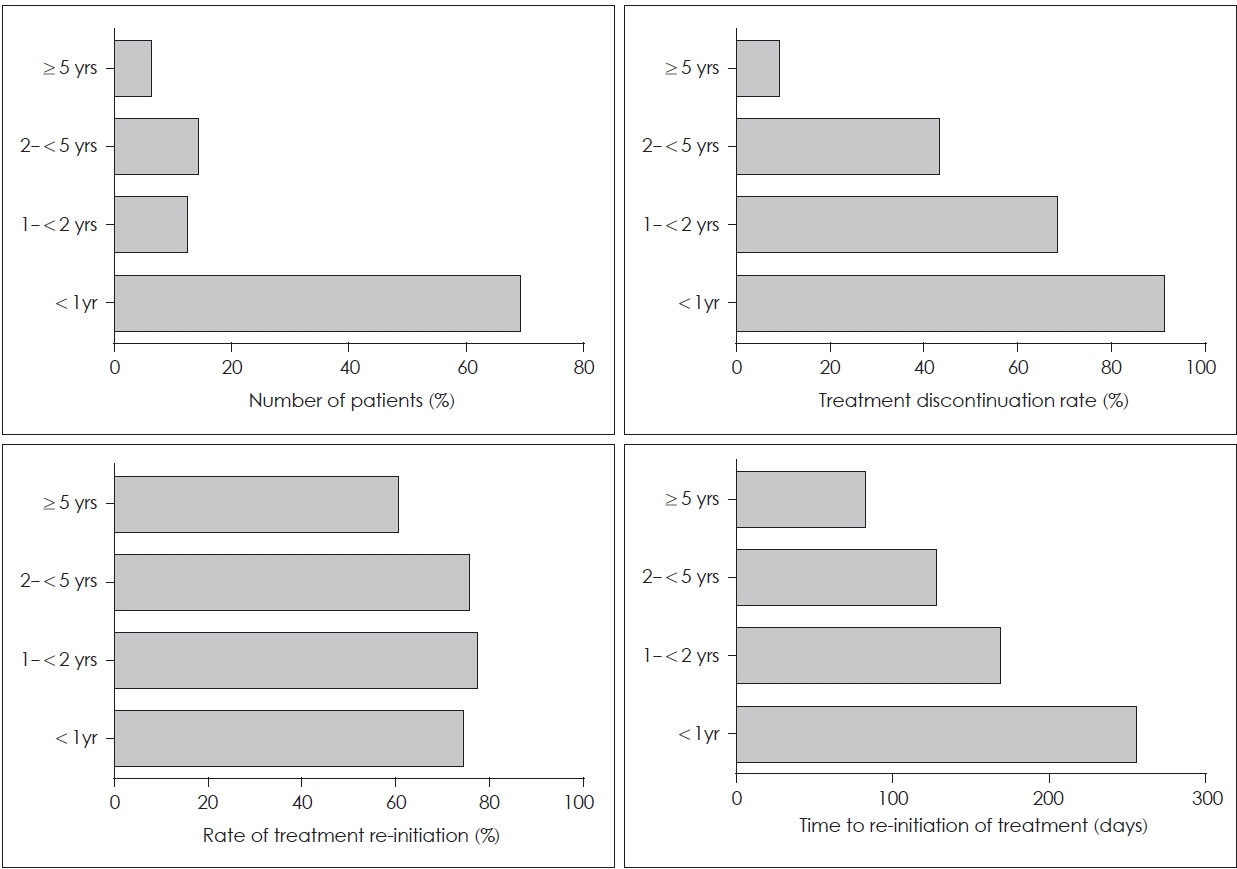
Of 30,143 patients with FES, 80.4% (n=24,231) received <2 years of the first antipsychotic treatment. In patients who discontinued treatment (n=23,030), the rate of treatment re-initiation was 74.2% (n=17,086). As the duration of the first antipsychotic treatment increased, the time to re-initiation of treatment decreased (β=-0.146, p<0.001); however, the rate of treatment re-initiation was relatively constant (hazard ratio=1.001, p<0.001).
Conclusion
Long-term antipsychotic treatment was not significantly associated with the rate of treatment re-initiation but showed a negative association with the time to re-initiation of treatment. Further research is needed to better understand the optimal treatment duration for FES.
Figure
Reference
-
1. McGrath J, Saha S, Chant D, Welham J. Schizophrenia: a concise overview of incidence, prevalence, and mortality. Epidemiol Rev. 2008; 30:67–76.
Article2. Robinson D, Woerner MG, Alvir JM, Bilder R, Goldman R, Geisler S, et al. Predictors of relapse following response from a first episode of schizophrenia or schizoaffective disorder. Arch Gen Psychiatry. 1999; 56:241–247.
Article3. Gitlin M, Nuechterlein K, Subotnik KL, Ventura J, Mintz J, Fogelson DL, et al. Clinical outcome following neuroleptic discontinuation in patients with remitted recent-onset schizophrenia. Am J Psychiatry. 2001; 158:1835–1842.
Article4. Boonstra G, Burger H, Grobbee DE, Kahn RS. Antipsychotic prophylaxis is needed after remission from a first psychotic episode in schizophrenia patients: results from an aborted randomised trial. Int J Psychiatry Clin Pract. 2011; 15:128–134.
Article5. Gaebel W, Riesbeck M, Wolwer W, Klimke A, Eickhoff M, von Wilmsdorff M, et al. Relapse prevention in first-episode schizophrenia: maintenance vs intermittent drug treatment with prodromebased early intervention: results of a randomized controlled trial within the German Research Network on Schizophrenia. J Clin Psychiatry. 2011; 72:205–218.6. Emsley R, Oosthuizen PP, Koen L, Niehaus DJ, Martinez G. Symptom recurrence following intermittent treatment in first-episode schizophrenia successfully treated for 2 years: a 3-year open-label clinical study. J Clin Psychiatry. 2012; 73:e541–547.7. McCreadie RG, Wiles D, Grant S, Crockett GT, Mahmood Z, Livingston MG, et al. The Scottish first episode schizophrenia study: VII. two-year follow-up. Acta Psychiatr Scand. 1989; 80:597–602.8. Kane JM. Treatment strategies to prevent relapse and encourage remission. J Clin Psychiatry. 2007; 68 Suppl 14:27–30.9. Wyatt RJ. Research in schizophrenia and the discontinuation of antipsychotic medications. Schizophr Bull. 1997; 23:3–9.
Article10. Lieberman JA, Alvir JM, Koreen A, Geisler S, Chakos M, Sheitman B, et al. Psychobiologic correlates of treatment response in schizophrenia. Neuropsychopharmacology. 1996; 14:13S–21S.11. Alvarez-Jimenez M, Priede A, Hetrick SE, Bendall S, Killackey E, Parker AG, et al. Risk factors for relapse following treatment for first episode psychosis: a systematic review and meta-analysis of longitudinal studies. Schizophr Res. 2012; 139:116–128.
Article12. De Hert M, Sermon J, Geerts P, Vansteelandt K, Peuskens J, Detraux J. The use of continuous treatment versus placebo or intermittent treatment strategies in stabilized patients with schizophrenia: a systematic review and meta-analysis of randomized controlled trials with first- and second-generation antipsychotics. CNS Drugs. 2015; 29:637–658.
Article13. Leucht S, Tardy M, Komossa K, Heres S, Kissling W, Salanti G, et al. Antipsychotic drugs versus placebo for relapse prevention in schizophrenia: a systematic review and meta-analysis. Lancet. 2012; 379:2063–2071.
Article14. Takeuchi H, Kantor N, Sanches M, Fervaha G, Agid O, Remington G. One-year symptom trajectories in patients with stable schizophrenia maintained on antipsychotics versus placebo: meta-analysis. Br J Psychiatry. 2017; 211:137–143.
Article15. Hui CLM, Honer WG, Lee EHM, Chang WC, Chan SKW, Chen ESM, et al. Long-term effects of discontinuation from antipsychotic maintenance following first-episode schizophrenia and related disorders: a 10 year follow-up of a randomised, double-blind trial. Lancet Psychiatry. 2018; 5:432–442.
Article16. Sampson S, Mansour M, Maayan N, Soares-Weiser K, Adams CE. Intermittent drug techniques for schizophrenia. Cochrane Database Syst Rev. 2013; CD006196.
Article17. Newcomer JW. Metabolic considerations in the use of antipsychotic medications: a review of recent evidence. J Clin Psychiatry. 2007; 68 Suppl 1:20–27.18. Bostwick JR, Guthrie SK, Ellingrod VL. Antipsychotic-induced hyperprolactinemia. Pharmacotherapy. 2009; 29:64–73.
Article19. Emsley R, Chiliza B, Asmal L, Harvey BH. The nature of relapse in schizophrenia. BMC Psychiatry. 2013; 13:50.
Article20. Shimomura Y, Kikuchi Y, Suzuki T, Uchida H, Mimura M, Takeuchi H. Antipsychotic treatment in the maintenance phase of schizophrenia: an updated systematic review of the guidelines and algorithms. Schizophr Res. 2020; 215:8–16.
Article21. Dans AL, Dans LF, Guyatt GH, Richardson S. Users’ guides to the medical literature: XIV. how to decide on the applicability of clinical trial results to your patient. JAMA. 1998; 279:545–549.22. Kim JA, Yoon S, Kim LY, Kim DS. Towards actualizing the value potential of Korea health insurance review and assessment (HIRA) data as a resource for health research: strengths, limitations, applications, and strategies for optimal use of HIRA data. J Korean Med Sci. 2017; 32:718–728.
Article23. Gardner DM, Murphy AL, O’Donnell H, Centorrino F, Baldessarini RJ. International consensus study of antipsychotic dosing. Am J Psychiatry. 2010; 167:686–693.
Article24. Sadock BJ, Sadock VA, Ruiz P. Kaplan & Sadock’s synopsis of psychiatry: behavioral sciences/clinical psychiatry. 11th ed. Philadelphia: Wolters Kluwer;2015.25. Barkhof E, Meijer CJ, de Sonneville LM, Linszen DH, de Haan L. Interventions to improve adherence to antipsychotic medication in patients with schizophrenia: a review of the past decade. Eur Psychiatry. 2012; 27:9–18.26. Haddad PM, Brain C, Scott J. Nonadherence with antipsychotic medication in schizophrenia: challenges and management strategies. Patient Relat Outcome Meas. 2014; 5:43–62.
Article27. Lieberman JA, Stroup TS, McEvoy JP, Swartz MS, Rosenheck RA, Perkins DO, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med. 2005; 353:1209–1223.
Article28. Tiihonen J, Tanskanen A, Taipale H. 20-year nationwide follow-up study on discontinuation of antipsychotic treatment in first-episode schizophrenia. Am J Psychiatry. 2018; 175:765–773.
Article29. Murray RM, Quattrone D, Natesan S, van Os J, Nordentoft M, Howes O, et al. Should psychiatrists be more cautious about the longterm prophylactic use of antipsychotics? Br J Psychiatry. 2016; 209:361–365.
Article30. Fenton WS, Blyler CR, Heinssen RK. Determinants of medication compliance in schizophrenia: empirical and clinical findings. Schizophr Bull. 1997; 23:637–651.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Cumulative Effect of Antipsychotic Usage on Mortality in Schizophrenia: A Nationwide Population-based Cohort Study in Korea
- Treatment-Resistant Schizophrenia : Pathophysiology and Treatment
- Drug Prescribing Patterns of Outpatients with Schizophrenia in a University Hospital
- Benzodiazepine Use among Patients with Schizophrenia in Korea: Analysis of Database of Health Insurance Review Agency
- Attitude Toward Antipsychotic Treatment According to Patients' Awareness of the Name of Their Illness in Patients with Schizophrenia