J Korean Med Sci.
2021 Oct;36(38):e236. 10.3346/jkms.2021.36.e236.
Correlation between Exposure to Fine Particulate Matter (PM 2.5 ) during Pregnancy and Congenital Anomalies: Its Surgical Perspectives
- Affiliations
-
- 1Division of Pediatric Surgery, Department of Surgery, Keimyung University School of Medicine, Daegu, Korea
- 2Department of Obstetrics & Gynecology, Keimyung University School of Medicine, Daegu, Korea
- 3Department of Urban Planning, Keimyung University, Daegu, Korea
- 4Division of Pediatric Surgery, Department of Surgery, Pusan National University Yangsan Hospital, Gyeongnam, Korea
- KMID: 2520775
- DOI: http://doi.org/10.3346/jkms.2021.36.e236
Abstract
- Background
Fine particulate matter (PM2.5) can easily penetrate blood vessels and tissues through the human respiratory tract and cause various health problems. Some studies reported that particular matter (PM) exposure during pregnancy is associated with low birth weight or congenital cardiovascular anomalies. This study aimed to investigate the correlation between the degree of exposure to PM ≤ 2.5 μm (PM2.5) during pregnancy and congenital anomalies relevant to the field of pediatric surgery.
Methods
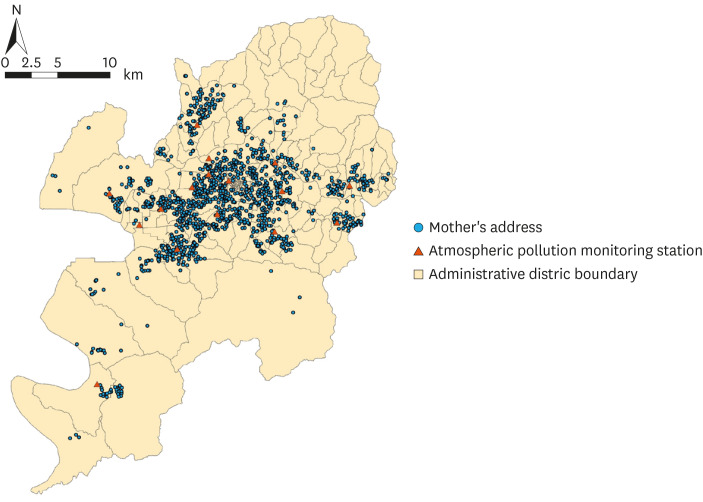
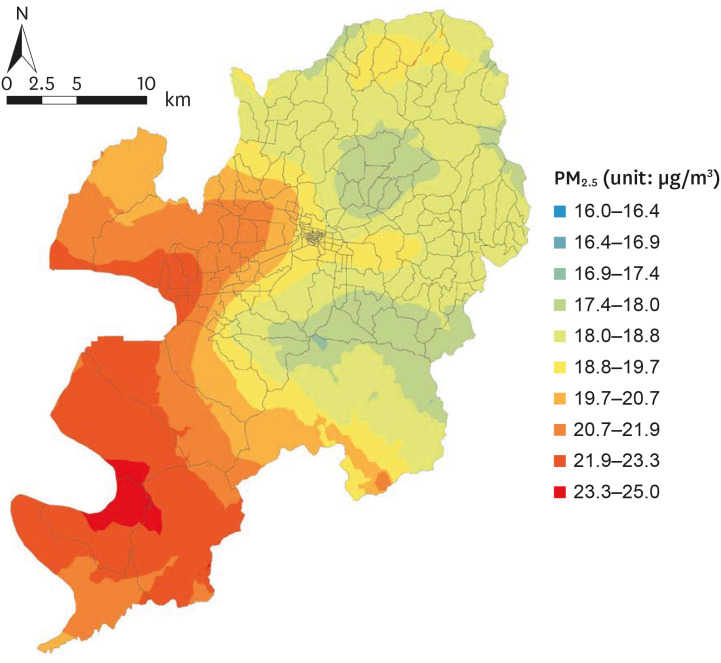
Mother-infant dyads with registered addresses in the Metropolitan City were selected during 3 years. The electronic medical records of mothers and neonates were retrospectively analyzed, with a focus on maternal age at delivery, date of delivery, gestation week, presence of diabetes mellitus (DM) or hypertension, parity, the residence of the mother and infant, infant sex, birth weight, Apgar score, and presence of congenital anomaly. The monthly PM2.5 concentration from the first month of pregnancy to the delivery was computed based on the mothers' residences.
Results
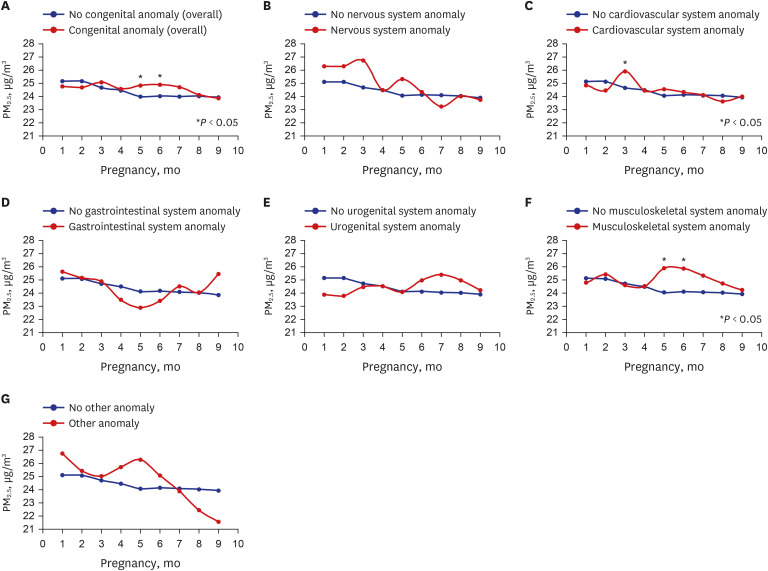
PM2.5 exposure concentration in the second trimester was higher in the congenital anomaly group than in the non-congenital anomaly group (24.82 ± 4.78 µg/m3, P = 0.023). PM2.5 exposure concentration did not affect the incidence of nervous, cardiovascular, and gastrointestinal anomalies. While statistically insignificant, the groups with nervous, cardiovascular, gastrointestinal, musculoskeletal, and other congenital anomalies were exposed to higher PM2.5 concentrations in the first trimester compared with their respective counterparts. The effect of PM2.5 concentration on the incidence of congenital anomalies was significant even after adjusting for the mother's age, presence of DM, hypertension, and parity. The incidence of congenital anomalies increased by 26.0% (95% confidence interval of 4.3% and 49.2%) per 7.23 µg/m3 elevation of PM2.5 interquartile range in the second trimester.
Conclusions
The congenital anomaly group was exposed to a higher PM2.5 concentration in the second trimester than the non-congenital anomaly group. The PM2.5 exposure concentration level in the first trimester tended to be higher in groups with anomalies than those without anomalies. This suggests that continuous exposure to a high PM2.5 concentration during pregnancy influences the incidence of neonatal anomalies in surgical respects.
Figure
Reference
-
1. Ministry of Environment. What if fine dust? Updated 2016. Accessed March 15, 2021. http://www.me.go.kr/home/web/board/read.do?menuId=10181&orgCd=&boardId=627350&boardMasterId=54.2. World Health Organization. Air pollution and cancer. Updated 2013. Accessed March 15, 2021. https://www.iarc.fr/wp-content/uploads/2018/07/AirPollutionandCancer161.pdf.3. Téllez-Rojo MM, Romieu I, Ruiz-Velasco S, Lezana MA, Hernández-Avila MM. Daily respiratory mortality and PM10 pollution in Mexico City: importance of considering place of death. Eur Respir J. 2000; 16(3):391–396. PMID: 11028649.4. Du Y, Xu X, Chu M, Guo Y, Wang J. Air particulate matter and cardiovascular disease: the epidemiological, biomedical and clinical evidence. J Thorac Dis. 2016; 8(1):E8–19. PMID: 26904258.5. Brook RD, Rajagopalan S, Pope CA 3rd, Brook JR, Bhatnagar A, Diez-Roux AV, et al. Particulate matter air pollution and cardiovascular disease: an update to the scientific statement from the American Heart Association. Circulation. 2010; 121(21):2331–2378. PMID: 20458016.6. Ailshire JA, Clarke P. Fine particulate matter air pollution and cognitive function among U.S. older adults. J Gerontol B Psychol Sci Soc Sci. 2015; 70(2):322–328. PMID: 24906394.
Article7. Lee JY, Kim JW, Kim EJ, Lee MY, Nam CW, Chung IS. Spatial analysis between particulate matter and emergency room visits for conjunctivitis and keratitis. Ann Occup Environ Med. 2018; 30(1):41–51. PMID: 29942521.
Article8. Ren S, Haynes E, Hall E, Hossain M, Chen A, Muglia L, et al. Periconception exposure to air pollution and risk of congenital malformations. J Pediatr. 2018; 193:76–84.e6. PMID: 29237538.
Article9. Wang X, Ding H, Ryan L, Xu X. Association between air pollution and low birth weight: a community-based study. Environ Health Perspect. 1997; 105(5):514–520. PMID: 9222137.
Article10. Seeni I, Ha S, Nobles C, Liu D, Sherman S, Mendola P. Air pollution exposure during pregnancy: maternal asthma and neonatal respiratory outcomes. Ann Epidemiol. 2018; 28(9):612–618.e4. PMID: 30153910.
Article11. Hwang BF, Lee YL, Jaakkola JJ. Air pollution and stillbirth: a population-based case-control study in Taiwan. Environ Health Perspect. 2011; 119(9):1345–1349. PMID: 21447454.
Article12. Huang CC, Chen BY, Pan SC, Ho YL, Guo YL. Prenatal exposure to PM2.5 and congenital heart diseases in Taiwan. Sci Total Environ. 2019; 655:880–886. PMID: 30481714.13. Lin HC, Guo JM, Ge P, Ou P. Association between prenatal exposure to ambient particulate matter and risk of hypospadias in offspring: a systematic review and meta-analysis. Environ Res. 2021; 192:110190. PMID: 32919959.
Article14. Kim YJ, Song IG, Kim KN, Kim MS, Chung SH, Choi YS, et al. Maternal exposure to particulate matter during pregnancy and adverse birth outcomes in the Republic of Korea. Int J Environ Res Public Health. 2019; 16(4):663–672.
Article15. Lee KS, Lim YH, Choi YJ, Kim S, Bae HJ, Han C, et al. Prenatal exposure to traffic-related air pollution and risk of congenital diseases in South Korea. Environ Res. 2020; 191:110060. PMID: 32805245.
Article16. Air Korea. Updated 2021. Accessed March 15, 2021. https://www.airkorea.or.kr/web.17. Al-Hamdan MZ, Crosson WL, Limaye AS, Rickman DL, Quattrochi DA, Estes MG Jr, et al. Methods for characterizing fine particulate matter using ground observations and remotely sensed data: potential use for environmental public health surveillance. J Air Waste Manag Assoc. 2009; 59(7):865–881. PMID: 19645271.
Article18. Zhang G, Rui X, Fan Y. Critical review of methods to estimate PM2.5 concentrations within specified research region. Inl J Geo-Inf. 2018; 7(9):368–382.19. Sadler TW. Langman's Medical Embryology. 14th ed. Philadelphia, PA, USA: Wolters Kluwer Health/Lippincott Williams & Wilkins;2018.20. Chun Y, Lee H. Understanding of human embryo development for teratogen counselling. J Korean Soc Matern Child Health. 2016; 20(2):112–118.21. Parkes B, Hansell AL, Ghosh RE, Douglas P, Fecht D, Wellesley D, et al. Risk of congenital anomalies near municipal waste incinerators in England and Scotland: Retrospective population-based cohort study. Environ Int. 2020; 134:104845. PMID: 31230843.
Article22. Jung EM, Kim KN, Park H, Shin HH, Kim HS, Cho SJ, et al. Association between prenatal exposure to PM2.5 and the increased risk of specified infant mortality in South Korea. Environ Int. 2020; 144:105997. PMID: 32768726.23. Chen G, Jin Z, Li S, Jin X, Tong S, Liu S, et al. Early life exposure to particulate matter air pollution (PM1, PM2.5 and PM10) and autism in Shanghai, China: a case-control study. Environ Int. 2018; 121(Pt 2):1121–1127. PMID: 30409451.24. Raz R, Roberts AL, Lyall K, Hart JE, Just AC, Laden F, et al. Autism spectrum disorder and particulate matter air pollution before, during, and after pregnancy: a nested case-control analysis within the Nurses' Health Study II Cohort. Environ Health Perspect. 2015; 123(3):264–270. PMID: 25522338.
Article25. Chen H, Chen X, Hong X, Liu C, Huang H, Wang Q, et al. Maternal exposure to ambient PM2.5 exaggerates fetal cardiovascular maldevelopment induced by homocysteine in rats. Environ Toxicol. 2017; 32(3):877–889. PMID: 27203204.26. Zhang B, Liang S, Zhao J, Qian Z, Bassig BA, Yang R, et al. Maternal exposure to air pollutant PM2.5 and PM10 during pregnancy and risk of congenital heart defects. J Expo Sci Environ Epidemiol. 2016; 26(4):422–427. PMID: 26883477.27. Christianson RE. The relationship between maternal smoking and the incidence of congenital anomalies. Am J Epidemiol. 1980; 112(5):684–695. PMID: 7435494.
Article28. Werler MM, Sheehan JE, Mitchell AA. Association of vasoconstrictive exposures with risks of gastroschisis and small intestinal atresia. Epidemiology. 2003; 14(3):349–354. PMID: 12859037.
Article