Korean J Orthod.
2021 Jul;51(4):231-240. 10.4041/kjod.2021.51.4.231.
Root proximity of the anchoring miniscrews of orthodontic miniplates in the mandibular incisal area: Cone-beam computed tomographic analysis
- Affiliations
-
- 1Department of Oral and Maxillofacial Radiology, Graduate School, Kyung Hee University, Seoul, Korea
- 2Department of Surgery, Division of Plastic and Reconstructive Surgery, Craniofacial and Airway Orthodontic Clinic, Stanford University School of Medicine, Lucile Packard Children’s Hospital, Palo Alto, CA, USA
- 3Department of Orthodontics, Graduate School, Kyung Hee University, Seoul, Korea
- 4Department of Dental Education, Graduate School, Kyung Hee University, Seoul, Korea
- KMID: 2518516
- DOI: http://doi.org/10.4041/kjod.2021.51.4.231
Abstract
Objective
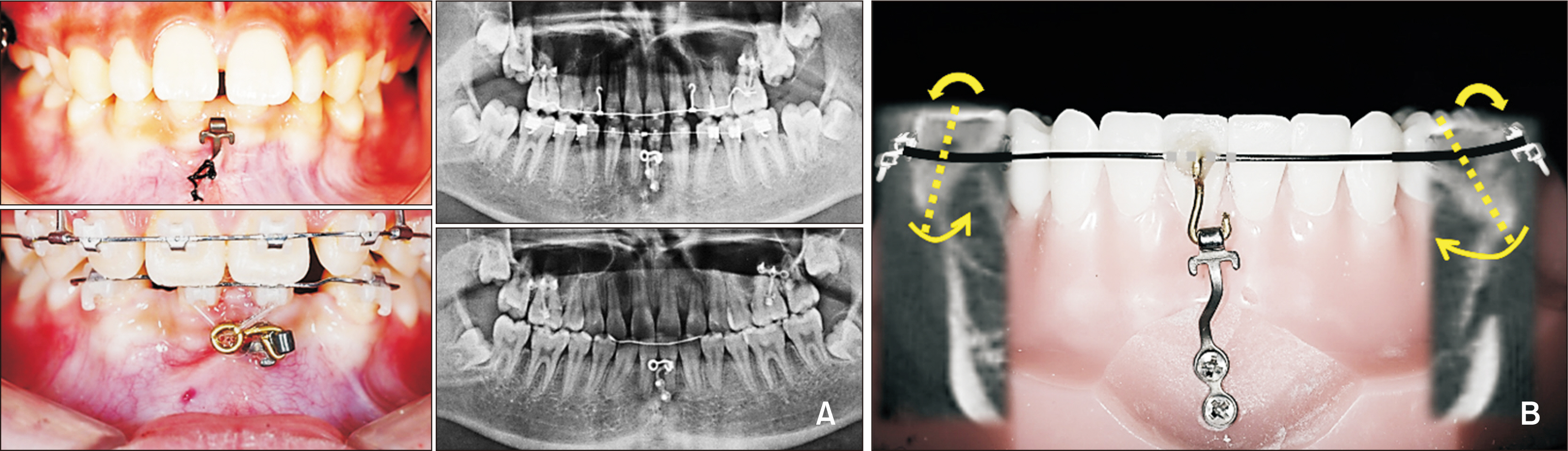
This outcome analysis study evaluated the actual positions of the orthodontic miniplate and miniplate anchoring screws (MPASs) and the risk factors affecting adjacent anatomic structures after miniplate placement in the mandibular incisal area.
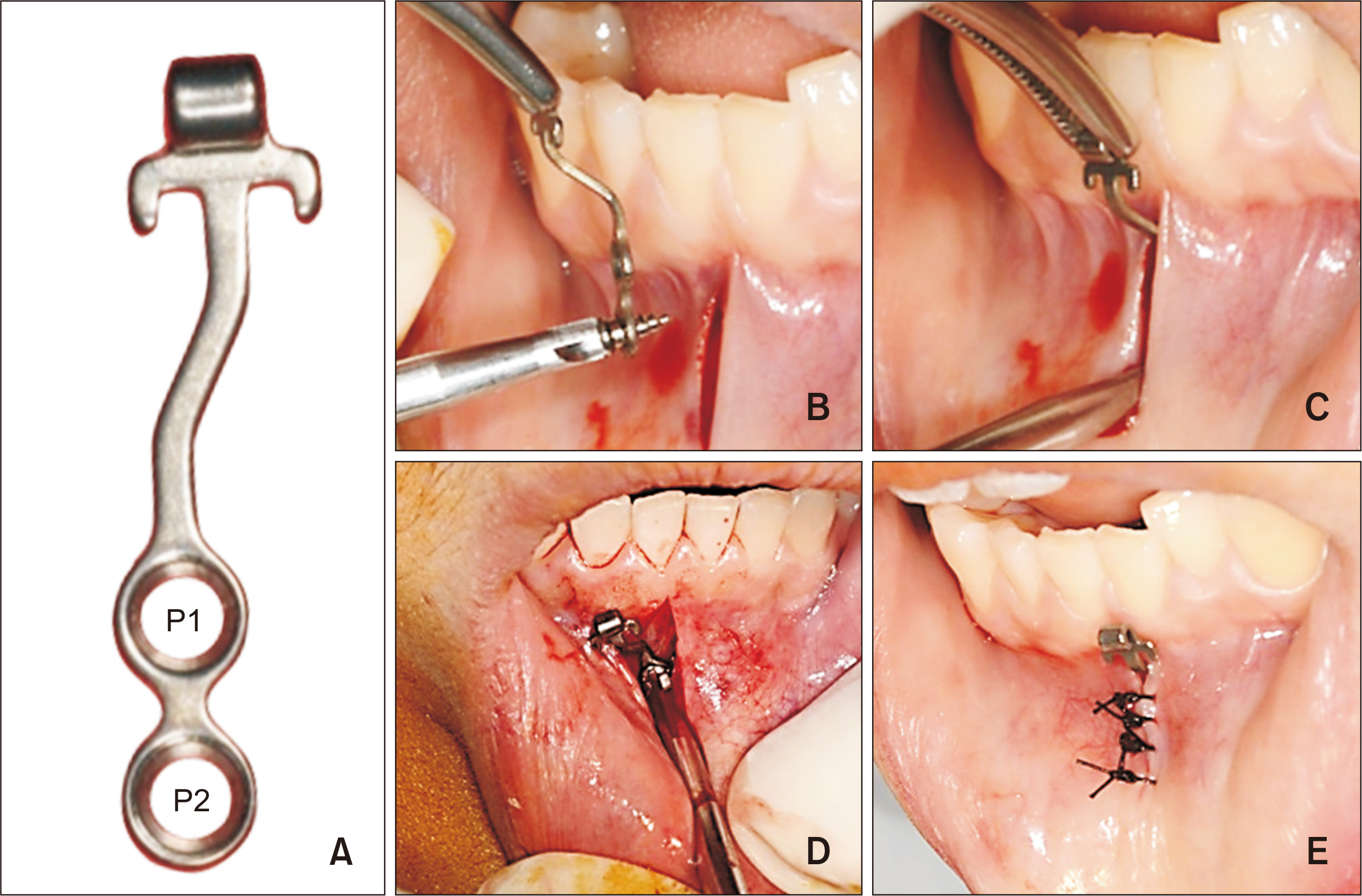
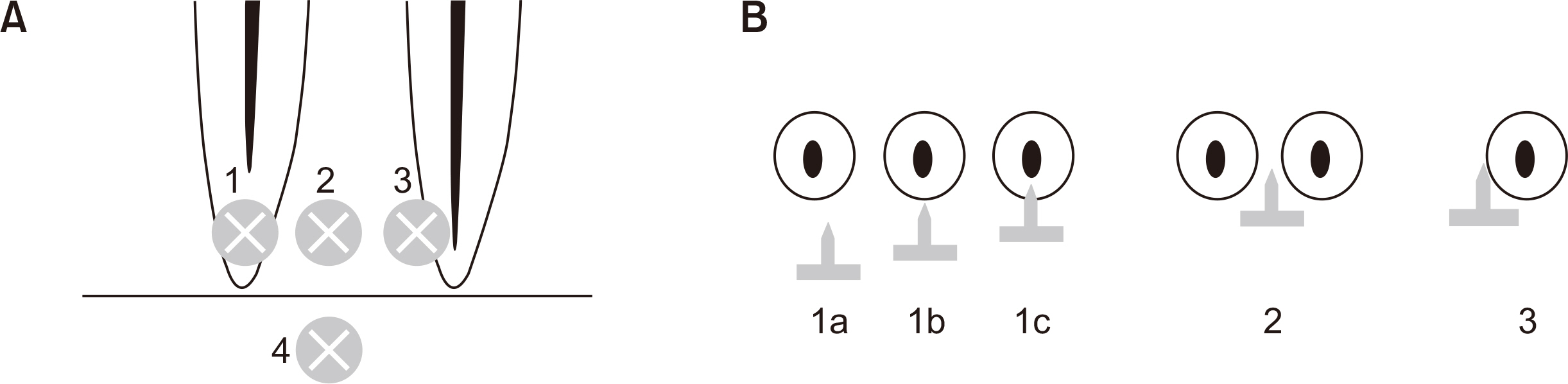
Methods
Cone-beam computed tomographic images of 97 orthodontic miniplates and their 194 MPASs (diameter, 1.5 mm; length, 4 mm) in patients whose miniplates provided sufficient clinical stability for orthodontic treatment were retrospectively reviewed. For evaluating the actual positions of the miniplates and analyzing the risk factors, including the effects on adjacent roots, MPAS placement height (PH), placement depth (PD), plate angle (PA), mental fossa angle (MA), and root proximity were assessed using the paired t-test, analysis of variance, and generalized linear model and regression analyses.
Results
The mean PDs of MPASs at positions 1 (P1) and 2 (P2) were 2.01 mm and 2.23 mm, respectively. PA was significantly higher in the Class III malocclusion group than in the other groups. PH was positively correlated with MA and PD at P1. Of the 97 MPASs at P1, 49 were in the no-root area and 48 in the dentulous area; moreover, 19 showed a degree of root contact (19.6%) without root perforation. All MPASs at P2 were in the no-root area.
Conclusions
Positioning the miniplate head approximately 1 mm lower than the mucogingival junction is highly likely to provide sufficient PH for the P1-MPASs to be placed in the no-root area.
Figure
Reference
-
1. Odman J, Lekholm U, Jemt T, Brånemark PI, Thilander B. 1988; Osseointegrated titanium implants--a new approach in orthodontic treatment. Eur J Orthod. 10:98–105. DOI: 10.1093/ejo/10.2.98. PMID: 3164683.
Article2. Roberts WE, Helm FR, Marshall KJ, Gongloff RK. 1989; Rigid endosseous implants for orthodontic and orthopedic anchorage. Angle Orthod. 59:247–56. DOI: 10.1043/0003-3219(1989)059<0247:REIFOA>2.0.CO;2. PMID: 2688486.3. Sadek MM, Sabet NE, Hassan IT. 2019; Type of tooth movement during en masse retraction of the maxillary anterior teeth using labial versus lingual biocreative therapy in adults: a randomized clinical trial. Korean J Orthod. 49:381–92. DOI: 10.4041/kjod.2019.49.6.381. PMID: 31815106. PMCID: PMC6883212.
Article4. Poggio PM, Incorvati C, Velo S, Carano A. 2006; "Safe zones": a guide for miniscrew positioning in the maxillary and mandibular arch. Angle Orthod. 76:191–7.5. Chen YJ, Chang HH, Huang CY, Hung HC, Lai EH, Yao CC. 2007; A retrospective analysis of the failure rate of three different orthodontic skeletal anchorage systems. Clin Oral Implants Res. 18:768–75. DOI: 10.1111/j.1600-0501.2007.01405.x. PMID: 17868386.
Article6. Ahn HW, Noh MK, Chung KR, Kim SH, Nelson G. 2020; Strategic molar uprighting using the biocreative reverse-curve technique. J Clin Orthod. 54:486–94. PMID: 32966268.7. Sugawara J, Kanzaki R, Takahashi I, Nagasaka H, Nanda R. 2006; Distal movement of maxillary molars in nongrowing patients with the skeletal anchorage system. Am J Orthod Dentofacial Orthop. 129:723–33. DOI: 10.1016/j.ajodo.2005.08.036. PMID: 16769490.
Article8. Chung KR, Kim YS, Linton JL, Lee YJ. 2002; The miniplate with tube for skeletal anchorage. J Clin Orthod. 36:407–12. PMID: 12165982.9. Lee SJ, Lin L, Kim SH, Chung KR, Donatelli RE. 2013; Survival analysis of a miniplate and tube device designed to provide skeletal anchorage. Am J Orthod Dentofacial Orthop. 144:349–56. DOI: 10.1016/j.ajodo.2013.03.026. PMID: 23992807.
Article10. Ahn HW, Chung KR, Kang SM, Lin L, Nelson G, Kim SH. 2012; Correction of dental Class III with posterior open bite by simple biomechanics using an anterior C-tube miniplate. Korean J Orthod. 42:270–8. DOI: 10.4041/kjod.2012.42.5.270. PMID: 23173121. PMCID: PMC3495259.
Article11. Chung KR, Kim SH, Kang YG, Nelson G. 2011; Orthodontic miniplate with tube as an efficient tool for borderline cases. Am J Orthod Dentofacial Orthop. 139:551–62. DOI: 10.1016/j.ajodo.2008.08.041. PMID: 21457867.
Article12. Kim GT, Kim SH, Choi YS, Park YJ, Chung KR, Suk KE, et al. 2009; Cone-beam computed tomography evaluation of orthodontic miniplate anchoring screws in the posterior maxilla. Am J Orthod Dentofacial Orthop. 136:628.e1–10. discussion 628–9. DOI: 10.1016/j.ajodo.2009.02.023. PMID: 19892272.
Article13. Kuroda S, Yamada K, Deguchi T, Hashimoto T, Kyung HM, Takano-Yamamoto T. 2007; Root proximity is a major factor for screw failure in orthodontic anchorage. Am J Orthod Dentofacial Orthop. 131(4 Suppl):S68–73. DOI: 10.1016/j.ajodo.2006.06.017. PMID: 17448389.
Article14. Kim SH, Kang SM, Choi YS, Kook YA, Chung KR, Huang JC. 2010; Cone-beam computed tomography evaluation of mini-implants after placement: is root proximity a major risk factor for failure? Am J Orthod Dentofacial Orthop. 138:264–76. DOI: 10.1016/j.ajodo.2008.07.026. PMID: 20816295.
Article15. Kadioglu O, Büyükyilmaz T, Zachrisson BU, Maino BG. 2008; Contact damage to root surfaces of premolars touching miniscrews during orthodontic treatment. Am J Orthod Dentofacial Orthop. 134:353–60. DOI: 10.1016/j.ajodo.2006.09.069. PMID: 18774081.
Article16. Tronstad L. 1988; Root resorption--etiology, terminology and clinical manifestations. Endod Dent Traumatol. 4:241–52. DOI: 10.1111/j.1600-9657.1988.tb00642.x. PMID: 3078294.17. Lee KJ, Joo E, Kim KD, Lee JS, Park YC, Yu HS. 2009; Computed tomographic analysis of tooth-bearing alveolar bone for orthodontic miniscrew placement. Am J Orthod Dentofacial Orthop. 135:486–94. DOI: 10.1016/j.ajodo.2007.05.019. PMID: 19361735.
Article18. Kim SY, Lim SH, Gang SN, Kim HJ. 2013; Crown and root lengths of incisors, canines, and premolars measured by cone-beam computed tomography in patients with malocclusions. Korean J Orthod. 43:271–8. DOI: 10.4041/kjod.2013.43.6.271. PMID: 24396736. PMCID: PMC3879283.
Article19. Kaya Y, Alkan Ö, Keskin S. 2017; An evaluation of the gingival biotype and the width of keratinized gingiva in the mandibular anterior region of individuals with different dental malocclusion groups and levels of crowding. Korean J Orthod. 47:176–85. DOI: 10.4041/kjod.2017.47.3.176. PMID: 28523244. PMCID: PMC5432439.
Article20. Kim MS, Lim SH, Jeong SR, Park JH. 2020; Maxillary molar intrusion and transverse decompensation to enable mandibular single-jaw surgery with rotational setback and transverse shift for a patient with mandibular prognathism and asymmetry. Am J Orthod Dentofacial Orthop. 157:818–31. DOI: 10.1016/j.ajodo.2019.02.022. PMID: 32487312.
Article21. Park JH, Choo H, Choi JY, Chung KR, Kim SH. 2021; Evaluation of strategic uprighting of the mandibular molars using an orthodontic miniplate and a nickel-titanium reverse curve arch wire: preliminary cephalometric study. Korean J Orthod. 51:179–88. DOI: 10.4041/kjod.2021.51.3.179. PMID: 33984225. PMCID: PMC8133900.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Reliability of panoramic radiography in predicting proximity of third molars to the mandibular canal: A comparison using cone-beam computed tomography
- Proximity of the mandibular molar root apex from the buccal bone surface: a cone-beam computed tomographic study
- Histomorphometric evaluation of the bone surrounding orthodontic miniscrews according to their adjacent root proximity
- Prevalence and features of distolingual roots in mandibular molars analyzed by cone-beam computed tomography
- Comparison between anterior segmental osteotomy versus conventional orthodontic treatment in root resorption: a radiographic study using cone-beam computed tomography