J Stroke.
2021 May;23(2):263-272. 10.5853/jos.2020.04637.
Long-Term Changes in Post-Stroke Depression, Emotional Incontinence, and Anger
- Affiliations
-
- 1Department of Neurology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Department of Neurology, Inje University Haeundae Paik Hospital, Busan, Korea
- 3Clinical Research Center, Asan Medical Center, Seoul, Korea
- 4Department of Neurology, Veterans Health Service Medical Center, Seoul, Korea
- 5Department of Neurology, Gachon University Gil Medical Center, Incheon, Korea
- 6Department of Neurology, Hanyang University Guri Hospital, Hanyang University College of Medicine, Guri, Korea
- 7Department of Neurology, Kyung Hee University Hospital, Seoul, Korea
- 8Department of Neurology, Myongji Hospital, Hanyang University College of Medicine, Goyang, Korea
- 9Department of Neurology, Dong-A University Hospital, Busan, Korea
- 10Department of Neurology, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 11Department of Neurology, Keimyung University Dongsan Medical Center, Daegu, Korea
- 12Department of Neurology, Dongguk University Ilsan Hospital, Goyang, Korea
- 13College of Nursing, Seoul National University, Seoul, Korea
- KMID: 2516415
- DOI: http://doi.org/10.5853/jos.2020.04637
Abstract
- Background and Purpose
Long-term changes in post-stroke depression (PSD), post-stroke emotional incontinence (PSEI), and post-stroke anger (PSA) have rarely been studied.
Methods
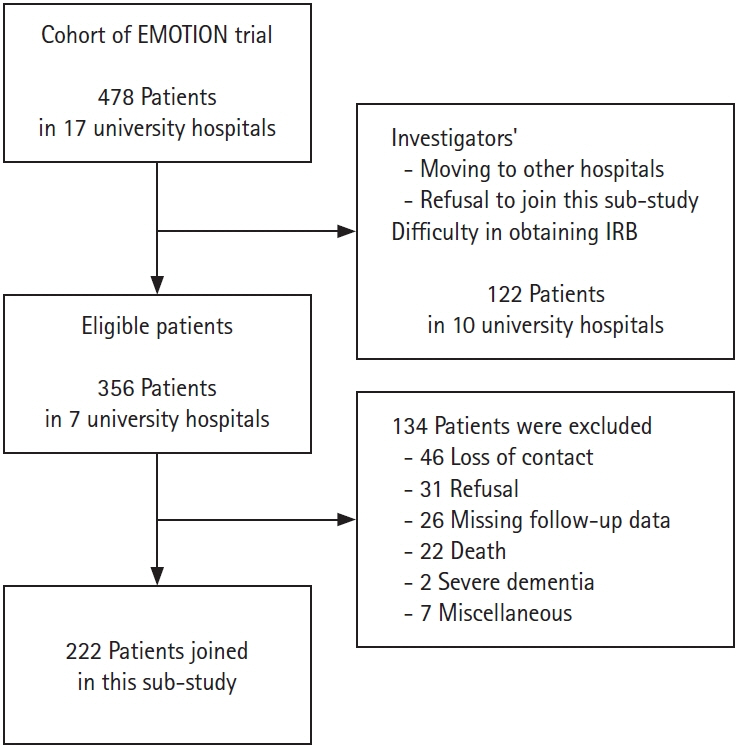
This is a sub-study of EMOTION, a randomized, placebo-controlled trial, that examined the efficacy of escitalopram on PSD, PSEI, and PSA in patients with stroke. We interviewed patients at the long-term period (LTP) using predefined questionnaires: Montgomery-Åsberg depression rating scale (MADRS) for PSD, modified Kim’s criteria for PSEI, and Spielberger trait anger scale for PSA. Additionally, the ENRICHD Social Support Instrument (ESSI) for the social support state and the modified Rankin Scale (mRS) were measured. We investigated the changes in and factors behind PSD, PSEI, and PSA at LTP.
Results
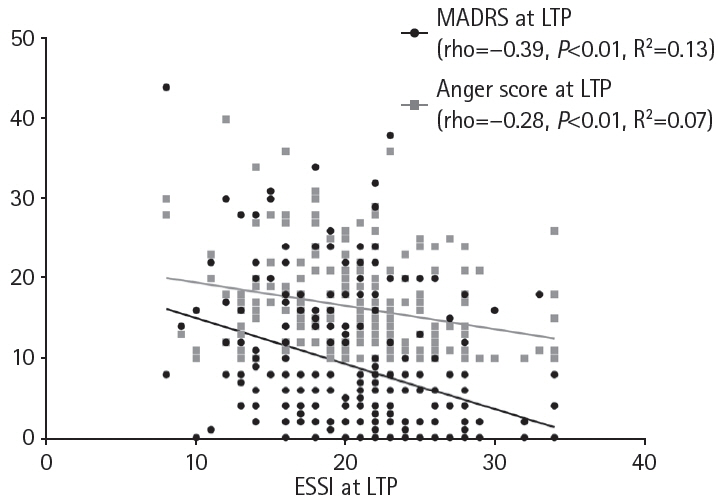
A total of 222 patients were included, and the median follow-up duration was 59.5 months (interquartile range, 50 to 70). Compared to the data at 6 months post-stroke, the prevalence of PSEI (11.7% at 6 months, 6.3% at LTP; P=0.05) and mean anger score (21.62, 16.24; P<0.01) decreased, while the prevalence of PSD (35.6%, 44.6%; P=0.03) and mean MADRS (6.16, 8.67; P<0.01) increased at LTP. ESSI was associated with PSD and PSA, but not with PSEI. The effect of the baseline National Institutes of Health Stroke Scale score on PSD decreased over time. The effect of low social support on PSD was greater than that of mRS at LTP.
Conclusions
The prevalence and degree of PSD significantly increased, while those of PSEI and PSA decreased at LTP. PSD in this stage appeared to be more closely associated with a lack of social support than patients' physical disabilities.
Keyword
Figure
Reference
-
References
1. Kim JS, Choi S, Kwon SU, Seo YS. Inability to control anger or aggression after stroke. Neurology. 2002; 58:1106–1108.
Article2. Kim JS, Choi-Kwon S. Poststroke depression and emotional incontinence: correlation with lesion location. Neurology. 2000; 54:1805–1810.
Article3. Kim JS. Post-stroke mood and emotional disturbances: pharmacological therapy based on mechanisms. J Stroke. 2016; 18:244–255.
Article4. Hackett ML, Pickles K. Part I: frequency of depression after stroke: an updated systematic review and meta-analysis of observational studies. Int J Stroke. 2014; 9:1017–1025.
Article5. Towfighi A, Ovbiagele B, El Husseini N, Hackett ML, Jorge RE, Kissela BM, et al. Poststroke depression: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2017; 48:e30–e43.
Article6. Werheid K. A two-phase pathogenetic model of depression after stroke. Gerontology. 2015; 62:33–39.
Article7. Kim JS, Lee EJ, Chang DI, Park JH, Ahn SH, Cha JK, et al. Efficacy of early administration of escitalopram on depressive and emotional symptoms and neurological dysfunction after stroke: a multicentre, double-blind, randomised, placebo- controlled study. Lancet Psychiatry. 2017; 4:33–41.8. Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979; 134:382–389.
Article9. Kearns NP, Cruickshank CA, McGuigan KJ, Riley SA, Shaw SP, Snaith RP. A comparison of depression rating scales. Br J Psychiatry. 1982; 141:45–49.10. Kang HJ, Stewart R, Kim JM, Jang JE, Kim SY, Bae KY, et al. Comparative validity of depression assessment scales for screening poststroke depression. J Affect Disord. 2013; 147:186–191.
Article11. Lee EJ, Kim JS, Chang DI, Park JH, Ahn SH, Cha JK, et al. Differences in therapeutic responses and factors affecting poststroke depression at a later stage according to baseline depression. J Stroke. 2018; 20:258–267.
Article12. Brott T, Adams HP Jr, Olinger CP, Marler JR, Barsan WG, Biller J, et al. Measurements of acute cerebral infarction: a clinical examination scale. Stroke. 1989; 20:864–870.
Article13. Farrell B, Godwin J, Richards S, Warlow C. The United Kingdom transient ischaemic attack (UK-TIA) aspirin trial: final results. J Neurol Neurosurg Psychiatry. 1991; 54:1044–1054.
Article14. Rao N. The clinical pharmacokinetics of escitalopram. Clin Pharmacokinet. 2007; 46:281–290.
Article15. Mitchell PH, Powell L, Blumenthal J, Norten J, Ironson G, Pitula CR, et al. A short social support measure for patients recovering from myocardial infarction: the ENRICHD Social Support Inventory. J Cardiopulm Rehabil. 2003; 23:398–403.16. ENRICHD Investigators. Enhancing recovery in coronary heart disease (ENRICHD): baseline characteristics. Am J Cardiol. 2001; 88:316–322.17. Ayerbe L, Ayis S, Rudd AG, Heuschmann PU, Wolfe CD. Natural history, predictors, and associations of depression 5 years after stroke: the South London Stroke Register. Stroke. 2011; 42:1907–1911.18. Ayerbe L, Ayis S, Crichton S, Wolfe CD, Rudd AG. The longterm outcomes of depression up to 10 years after stroke: the South London Stroke Register. J Neurol Neurosurg Psychiatry. 2014; 85:514–521.
Article19. Ki M, Paik JW, Choi KS, Ryu SH, Han C, Lee K, et al. Delays in depression treatment among Korean population. Asia Pac Psychiatry. 2014; 6:414–424.
Article20. Turvey CL, Jogerst G, Kim MY, Frolova E. Cultural differences in depression-related stigma in late-life: a comparison between the USA, Russia, and South Korea. Int Psychogeriatr. 2012; 24:1642–1647.
Article21. Organization for Economic Cooperation. Health at a glance 2015: OECD indicators. Paris: OECD;2015.22. Chuang CS, Yang TY, Muo CH, Su HL, Sung FC, Kao CH. Hyperlipidemia, statin use and the risk of developing depression: a nationwide retrospective cohort study. Gen Hosp Psychiatry. 2014; 36:497–501.
Article23. Valkanova V, Ebmeier KP. Vascular risk factors and depression in later life: a systematic review and meta-analysis. Biol Psychiatry. 2013; 73:406–413.
Article24. House A, Dennis M, Molyneux A, Warlow C, Hawton K. Emotionalism after stroke. BMJ. 1989; 298:991–994.
Article25. Andersen G, Ingeman-Nielsen M, Vestergaard K, Riis JO. Pathoanatomic correlation between poststroke pathological crying and damage to brain areas involved in serotonergic neurotransmission. Stroke. 1994; 25:1050–1052.
Article26. Kim JM, Stewart R, Kang HJ, Bae KY, Kim SW, Shin IS, et al. Associations of serotonergic genes with poststroke emotional incontinence. Int J Geriatr Psychiatry. 2012; 27:799–806.
Article27. Kim JS. Post-stroke emotional incontinence after small lenticulocapsular stroke: correlation with lesion location. J Neurol. 2002; 249:805–810.
Article28. Murai T, Barthel H, Berrouschot J, Sorger D, von Cramon DY, Müller U. Neuroimaging of serotonin transporters in poststroke pathological crying. Psychiatry Res. 2003; 123:207–211.
Article29. Leykin Y, Dunn LB, Muñoz RF. The effect of depression on the decision to join a clinical trial. J Consult Clin Psychol. 2017; 85:751–756.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Post-stroke Mood and Emotional Disturbances: Pharmacological Therapy Based on Mechanisms
- Post-stroke Depression, Anxiety, Emotional incontinence, Anger-proneness and Fatigue
- Anger, a Result and Cause of Stroke: A Narrative Review
- A Subjectivity Study on Type of Emotional Response of Stroke Patient
- A Study on Perceived Entrapment, Anger and Depression in Adolescent Women