Ann Pediatr Endocrinol Metab.
2020 Mar;25(1):10-14. 10.6065/apem.2020.25.1.10.
Updates on bone health in children with gastrointestinal diseases
- Affiliations
-
- 1Department of Pediatrics, Seoul National University Bundang Hospital, Seongnam, Korea
- 2Department of Pediatrics, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2501031
- DOI: http://doi.org/10.6065/apem.2020.25.1.10
Abstract
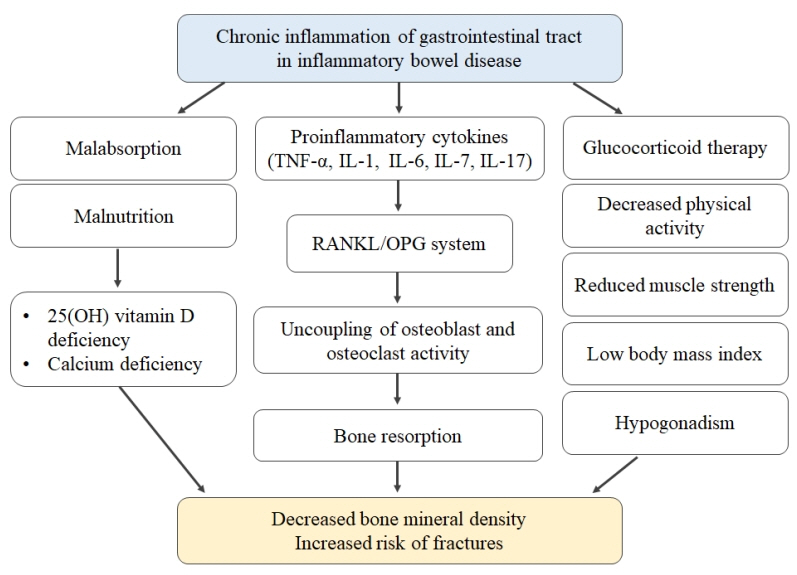
- Chronic gastrointestinal diseases such as inflammatory bowel disease, malabsorption syndromes (e.g., intestinal lymphangiectasia, celiac disease, congenital chloride diarrhea, cystic fibrosis), and postsubtotal gastrectomy state or short-bowel syndrome after extensive bowel resection are related to poor bone health in pediatric patients due to increased risks of low bone mineral density, osteoporosis, and fractures. The pathophysiology of abnormal bone health in pediatric gastrointestinal diseases may present from inflammation to malabsorption. In children with chronic gastrointestinal diseases at high risk of poor bone health, routine evaluation using dual-energy X-ray absorptiometry and appropriate prevention or treatment strategies are needed.
Keyword
Figure
Reference
-
References
1. Oh HJ, Ryu KH, Park BJ, Yoon BH. Osteoporosis and osteoporotic fractures in gastrointestinal disease. J Bone Metab. 2018; 25:213–7.
Article2. Katz S, Weinerman S. Osteoporosis and gastrointestinal disease. Gastroenterol Hepatol (N Y). 2010; 6:506–17.3. Sohn J, Chang EJ, Yang HR. Vitamin D status and bone mineral density in children with inflammatory bowel disease compared to those with functional abdominal pain. J Korean Med Sci. 2017; 32:961–7.
Article4. Szafors P, Che H, Barnetche T, Morel J, Gaujoux-Viala C, Combe B, et al. Risk of fracture and low bone mineral density in adults with inflammatory bowel diseases. A systematic literature review with meta-analysis. Osteoporos Int. 2018; 29:2389–97.
Article5. Sylvester FA, Wyzga N, Hyams JS, Davis PM, Lerer T, Vance K, et al. Natural history of bone metabolism and bone mineral density in children with inflammatory bowel disease. Inflamm Bowel Dis. 2007; 13:42–50.
Article6. Scott EM, Gaywood I, Scott BB. Guidelines for osteoporosis in coeliac disease and inflammatory bowel disease. British Society of Gastroenterology. Gut. 2000; 46 Suppl 1:i1–8.
Article7. Ghishan FK, Kiela PR. Advances in the understanding of mineral and bone metabolism in inflammatory bowel diseases. Am J Physiol Gastrointest Liver Physiol. 2011; 300:G191–201.
Article8. van Hogezand RA, Hamdy NA. Skeletal morbidity in inflammatory bowel disease. Scand J Gastroenterol Suppl. 2006; (243):59–64.
Article9. Tilg H, Moschen AR, Kaser A, Pines A, Dotan I. Gut, inflammation and osteoporosis: basic and clinical concepts. Gut. 2008; 57:684–94.
Article10. Schüle S, Rossel JB, Frey D, Biedermann L, Scharl M, Zeitz J, et al. Widely differing screening and treatment practice for osteoporosis in patients with inflammatory bowel diseases in the Swiss IBD cohort study. Medicine (Baltimore). 2017; 96:e6788.
Article11. Ward LM, Ma J, Rauch F, Benchimol EI, Hay J, Leonard MB, et al. Musculoskeletal health in newly diagnosed children with Crohn's disease. Osteoporos Int. 2017; 28:3169–77.
Article12. Guz-Mark A, Rinawi F, Egotubov O, Shimon I, Shamir R, Assa A. Pediatric-onset inflammatory bowel disease poses risk for low bone mineral density at early adulthood. Dig Liver Dis. 2017; 49:639–42.
Article13. Miele E, Shamir R, Aloi M, Assa A, Braegger C, Bronsky J, et al. Nutrition in Pediatric inflammatory bowel disease: a position paper on behalf of the porto inflammatory bowel disease group of the european society of pediatric gastroenterology, hepatology and nutrition. J Pediatr Gastroenterol Nutr. 2018; 66:687–708.14. Melek J, Sakuraba A. Efficacy and safety of medical therapy for low bone mineral density in patients with inflammatory bowel disease: a meta-analysis and systematic review. Clin Gastroenterol Hepatol. 2014; 12:32–44.
Article15. Li XP, Shen WB, Long MQ, Meng XW, Lian XL, Yu M. Osteomalacia and osteoporosis associated with primary intestinal lymphangiectasis. Chin Med J (Engl). 2012; 125:1836–8.16. Sahli H, Ben Mbarek R, Elleuch M, Azzouz D, Meddeb N, Chéour E, et al. Osteomalacia in a patient with primary intestinal lymphangiectasis (Waldmann's disease). Joint Bone Spine. 2008; 75:73–5.
Article17. Ludvigsson JF, Bai JC, Biagi F, Card TR, Ciacci C, Ciclitira PJ, et al. Diagnosis and management of adult coeliac disease: guidelines from the British Society of Gastroenterology. Gut. 2014; 63:1210–28.
Article18. Fouda MA, Khan AA, Sultan MS, Rios LP, McAssey K, Armstrong D. Evaluation and management of skeletal health in celiac disease: position statement. Can J Gastroenterol. 2012; 26:819–29.
Article19. Bernstein CN, Leslie WD, Leboff MS. AGA technical review on osteoporosis in gastrointestinal diseases. Gastroenterology. 2003; 124:795–841.
Article20. Turner J, Pellerin G, Mager D. Prevalence of metabolic bone disease in children with celiac disease is independent of symptoms at diagnosis. J Pediatr Gastroenterol Nutr. 2009; 49:589–93.
Article21. Johnson E, Vu L, Matarese LE. Bacteria, bones, and stones: managing complications of short bowel syndrome. Nutr Clin Pract. 2018; 33:454–66.
Article22. Demehri FR, Simha S, Stephens L, Harris MB, Arnold MA, Brown PI, et al. Pediatric intestinal failure: predictors of metabolic bone disease. J Pediatr Surg. 2015; 50:958–62.
Article23. Ubesie AC, Heubi JE, Kocoshis SA, Henderson CJ, Mezoff AG, Rao MB, et al. Vitamin D deficiency and low bone mineral density in pediatric and young adult intestinal failure. J Pediatr Gastroenterol Nutr. 2013; 57:372–6.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Recent Updates on Vitamin D and Pediatric Gastrointestinal Diseases
- Evaluation and Management of Bone Health in Patients with Thyroid Diseases: A Position Statement of the Korean Thyroid Association
- Bone modeling, remodeling, and skeletal health in children and adolescents: mineral accrual, assessment and treatment
- Upper gastrointestinal diseases diagnosed by upper gastrointestinal fiberoptic endoscopy in children
- Updates on ankylosing spondylitis: pathogenesis and therapeutic agents