Anesth Pain Med.
2020 Apr;15(2):157-166. 10.17085/apm.2020.15.2.157.
Effect of preoperative administration of systemic alpha-2 agonists on postoperative pain: a systematic review and meta-analysis
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea
- KMID: 2500966
- DOI: http://doi.org/10.17085/apm.2020.15.2.157
Abstract
- Background
Alpha-2 agonists have sedative, analgesic, and opioid-sparing effects. Moreover, intraoperative or postoperative systemic administration of alpha-2 adrenergic agonists is known to reduce postoperative pain and opioid consumption. This meta-analysis investigated whether preoperative administration of alpha-2 agonists can affect postoperative pain and opioid consumption.
Methods
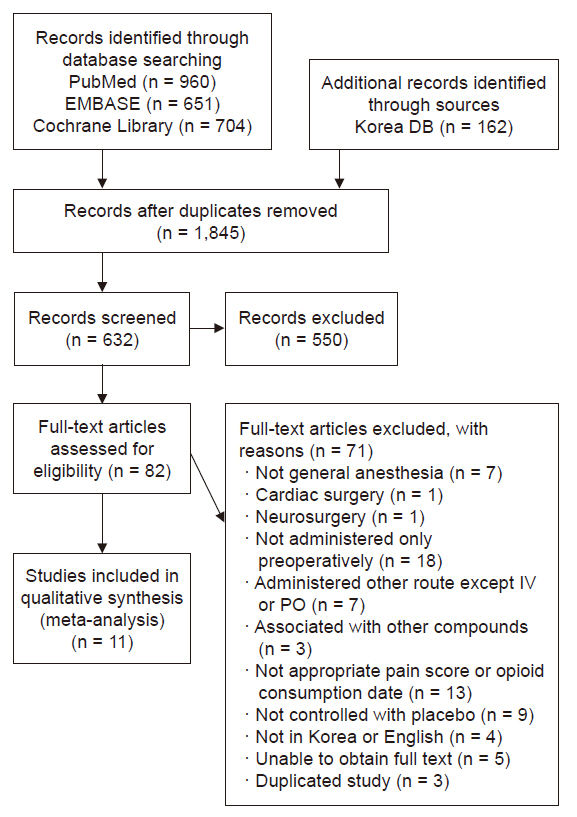
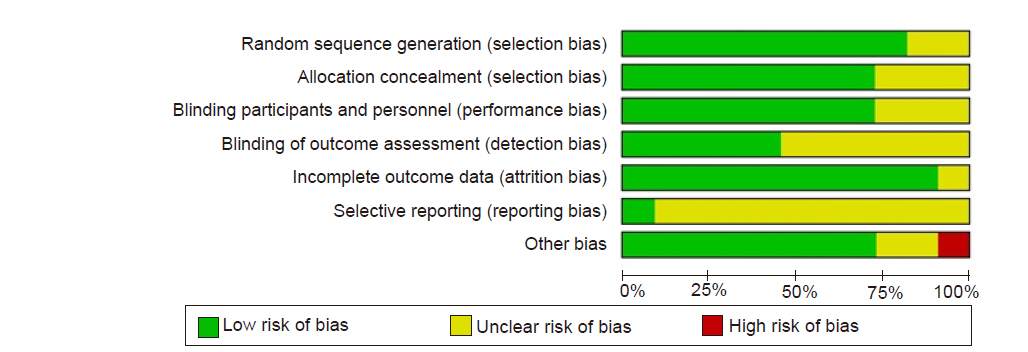
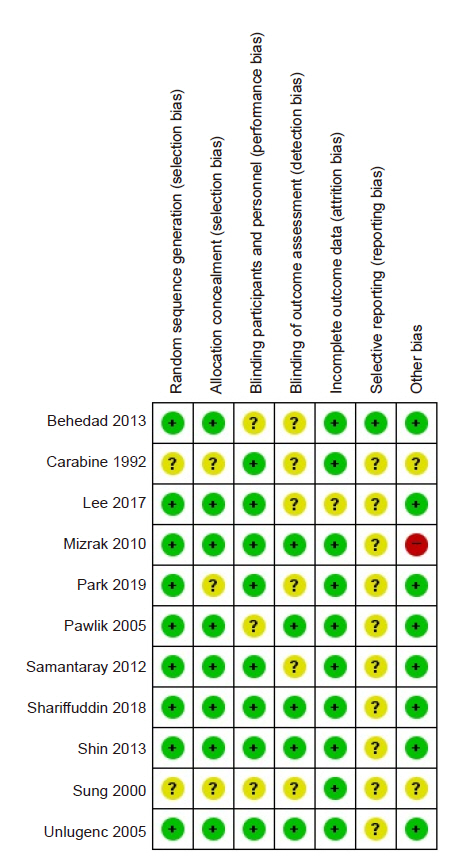
We searched the MEDLINE, EMBASE, Cochrane Library (CENTRAL), KoreaMed, and KMbase databases through March 2019 to identify relevant randomized controlled trials (RCTs) on the effect of preoperative systemic administration of alpha-2 agonists on postoperative pain and opioid consumption. We conducted a meta-analysis according to the Cochrane Collaboration guidelines. Standardized mean differences (SMDs) of postoperative pain intensity or dose of opioid consumption in the alpha-2 agonist group were extracted and combined using a random-effect model and were compared to those of the control group.
Results
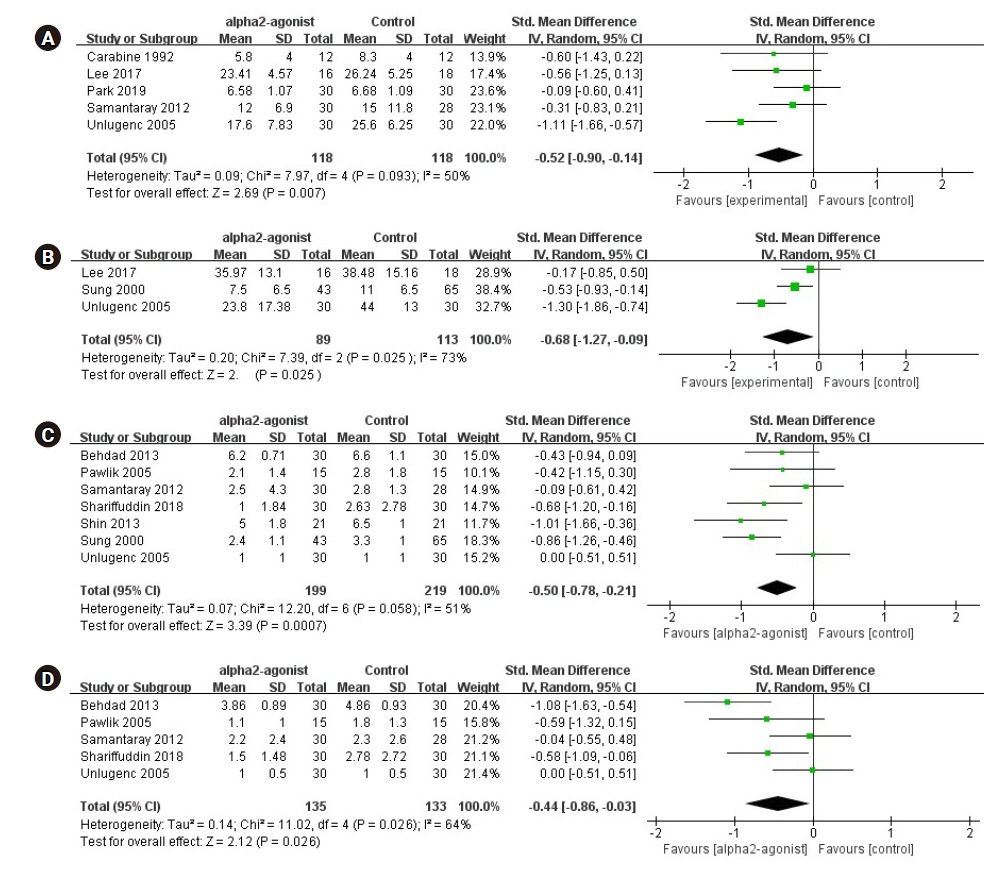
Eleven RCTs involving 748 participants were included in this meta-analysis. Preoperative administration of systemic alpha-2 agonists significantly reduced cumulative opioid consumption up to 6 h (SMD, –0.52; 95% confidence interval [–0.90 to –0.14]) and 24 h (SMD, –0.68 [–1.27 to –0.09]) after surgery. Moreover, preoperative administration of alpha-2 agonists significantly reduced postoperative pain intensity at 6 h (SMD, –0.50 [–0.78 to –0.21]) and 24 h (SMD, –0.44 [–0.86 to –0.03]).
Conclusions
In this meta-analysis, high degree of heterogeneity limits the preoperative administration of alpha-2 agonists in reducing postoperative opioid consumption and pain intensity. Future powered large RCTs are required to increase the certainty of evidence on the effect in reducing postoperative opioid consumption and pain intensity.
Keyword
Figure
Reference
-
1. Rasmussen ML, Mathiesen O, Dierking G, Christensen BV, Hilsted KL, Larsen TK, et al. Multimodal analgesia with gabapentin, ketamine and dexamethasone in combination with paracetamol and ketorolac after hip arthroplasty: a preliminary study. Eur J Anaesthesiol. 2010; 27:324–30.2. Khan ZP, Ferguson CN, Jones RM. Alpha-2 and imidazoline receptor agonists. Their pharmacology and therapeutic role. Anaesthesia. 1999; 54:146–65.3. Kamibayashi T, Maze M. Clinical uses of alpha2 -adrenergic agonists. Anesthesiology. 2000; 93:1345–9.4. Blaudszun G, Lysakowski C, Elia N, Tramèr MR. Effect of perioperative systemic α2 agonists on postoperative morphine consumption and pain intensity: systematic review and meta-analysis of randomized controlled trials. Anesthesiology. 2012; 116:1312–22.5. Shariffuddin II, Teoh WH, Wahab S, Wang CY. Effect of single-dose dexmedetomidine on postoperative recovery after ambulatory ureteroscopy and ureteric stenting: a double blind randomized controlled study. BMC Anesthesiol. 2018; 18:3.6. Sung CS, Lin SH, Chan KH, Chang WK, Chow LH, Lee TY. Effect of oral clonidine premedication on perioperative hemodynamic response and postoperative analgesic requirement for patients undergoing laparoscopic cholecystectomy. Acta Anaesthesiol Sin. 2000; 38:23–9.7. Lee KY, Lee WY, Kim KM, Yoo BH, Lee S, Lim YH, et al. The effect of pre-anesthetic administration of dexmedetomidine on the consumption of opioids in postoperative gynecologic patients. Anesth Pain Med. 2017; 12:37–41.8. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009; 339:b2535.9. Viera AJ, Garrett JM. Understanding interobserver agreement: the kappa statistic. Fam Med. 2005; 37:360–3.10. Carabine UA, Allen RW, Moore J. Partial attenuation of the pressor response to endotracheal intubation. A comparison of the effects of intravenous clonidine and fentanyl. Eur J Anaesthesiol. 1992; 9:325–9.11. Park H, Kim HS, Kim JW, Lee GG, Park DH, Jeong CY, et al. Effects of preanesthetic single administration of dexmedetomidine on the remifentanil and propofol requirement during laparoscopic cholecystectomy. Anesth Pain Med. 2019; 14:29–34.12. Shin HW, Yoo HN, Kim DH, Lee H, Shin HJ, Lee HW. Preanesthetic dexmedetomidine 1 µg/kg single infusion is a simple, easy, and economic adjuvant for general anesthesia. Korean J Anesthesiol. 2013; 65:114–20.13. Pawlik MT, Hansen E, Waldhauser D, Selig C, Kuehnel TS. Clonidine premedication in patients with sleep apnea syndrome: a randomized, double-blind, placebo-controlled study. Anesth Analg. 2005; 101:1374–80.14. Mizrak A, Koruk S, Bilgi M, Kocamer B, Erkutlu I, Ganidagli S, et al. Pretreatment with dexmedetomidine or thiopental decreases myoclonus after etomidate: a randomized, double-blind controlled trial. J Surg Res. 2010; 159:e11–6.15. Samantaray A, Rao MH, Chandra A. The effect on post-operative pain of intravenous clonidine given before induction of anaesthesia. Indian J Anaesth. 2012; 56:359–64.16. Behdad S, Ayatollahi V, Yazdi AG, Mortazavizadeh A, Niknam F. Effect of oral low dose clonidine premedication on postoperative pain in patients undergoing abdominal hysterectomy: a randomized placebo controlled clinical trial. Rev Med Chir Soc Med Nat Iasi. 2013; 117:934–41.17. Unlugenc H, Gunduz M, Guler T, Yagmur O, Isik G. The effect of pre-anaesthetic administration of intravenous dexmedetomidine on postoperative pain in patients receiving patient-controlled morphine. Eur J Anaesthesiol. 2005; 22:386–91.18. Schnabel A, Meyer-Frießem CH, Reichl SU, Zahn PK, Pogatzki-Zahn EM. Is intraoperative dexmedetomidine a new option for postoperative pain treatment? A meta-analysis of randomized controlled trials. Pain. 2013; 154:1140–9.19. Kalkman CJ, Visser K, Moen J, Bonsel GJ, Grobbee DE, Moons KG. Preoperative prediction of severe postoperative pain. Pain. 2003; 105:415–23.20. Kelly DJ, Ahmad M, Brull SJ. Preemptive analgesia I: physiological pathways and pharmacological modalities. Can J Anaesth. 2001; 48:1000–10.21. Roberts GW, Bekker TB, Carlsen HH, Moffatt CH, Slattery PJ, McClure AF. Postoperative nausea and vomiting are strongly influenced by postoperative opioid use in a dose-related manner. Anesth Analg. 2005; 101:1343–8.22. Liu SS, Strodtbeck WM, Richman JM, Wu CL. A comparison of regional versus general anesthesia for ambulatory anesthesia: a meta-analysis of randomized controlled trials. Anesth Analg. 2005; 101:1634–42.23. Marret E, Kurdi O, Zufferey P, Bonnet F. Effects of nonsteroidal antiinflammatory drugs on patient-controlled analgesia morphine side effects: meta-analysis of randomized controlled trials. Anesthesiology. 2005; 102:1249–60.24. Gurbet A, Basagan-Mogol E, Turker G, Ugun F, Kaya FN, Ozcan B. Intraoperative infusion of dexmedetomidine reduces perioperative analgesic requirements. Can J Anaesth. 2006; 53:646–52.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Factors Related to Persistent Postoperative Pain after Cardiac Surgery: A Systematic Review and Meta-Analysis
- An Introduction of the Systematic Review and Meta-Analysis
- Effect of premedication on postoperative pain after root canal therapy in patients with irreversible pulpitis: a systematic review and meta-analysis
- Effect of single dose preoperative intravenous ibuprofen on postoperative pain and opioid consumption: a systematic review and meta-analysis
- Introduction to systematic review and meta-analysis