Diabetes Metab J.
2020 Feb;44(1):103-112. 10.4093/dmj.2018.0160.
Combined Aerobic and Resistance Exercise Training Reduces Circulating Apolipoprotein J Levels and Improves Insulin Resistance in Postmenopausal Diabetic Women
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Department of Internal Medicine, Pusan National University Hospital, Pusan National University School of Medicine, Busan, Korea. drsskim7@gmail.com
- 2Biomedical Research Institute, Pusan National University Hospital, Busan, Korea.
- 3Division of Endocrinology, Diabetes, and Metabolism, Department of Medicine, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA, USA. ykim2@bidmc.harvard.edu
- 4Department of Physical Education, Kyungnam University College of Education, Changwon, Korea.
- 5Department of Marine Sports, Pukyong National University, Busan, Korea.
- 6Nutrition Service Team, Pusan National University Hospital, Busan, Korea.
- 7Kim Yong Ki Internal Medicine Clinic, Busan, Korea.
- 8Division of Nephrology, Department of Internal Medicine, Pusan National University Hospital, Pusan National University School of Medicine, Busan, Korea.
- KMID: 2470959
- DOI: http://doi.org/10.4093/dmj.2018.0160
Abstract
- BACKGROUND
Circulating apolipoprotein J (ApoJ) is closely associated with insulin resistance; however, the effect of exercise on circulating ApoJ levels and the association of ApoJ with metabolic indices remain unknown. Here, we investigated whether a combined exercise can alter the circulating ApoJ level, and whether these changes are associated with metabolic indices in patients with type 2 diabetes mellitus.
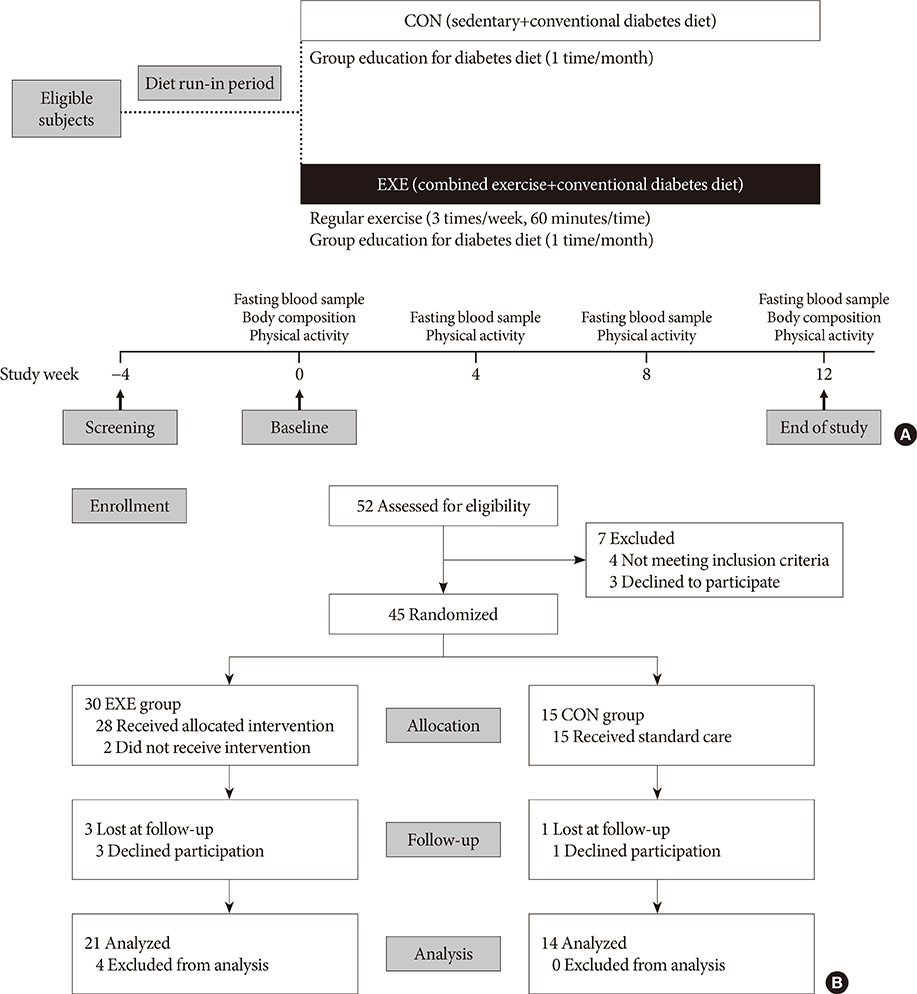
METHODS
Postmenopausal women with type 2 diabetes mellitus were randomly assigned into either an exercise (EXE, n=30) or control (CON, n=15) group. Participants in the EXE group were enrolled in a 12-week program consisting of a combination of aerobic and resistance exercises. At baseline, 4, 8, and 12 weeks, body composition and metabolic parameters including homeostatic model assessment of insulin resistance (HOMA-IR) and serum ApoJ levels were assessed.
RESULTS
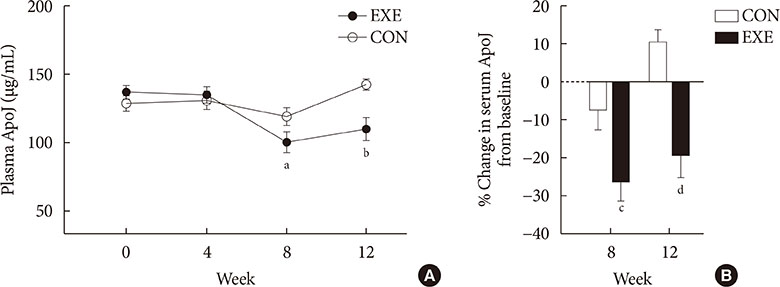
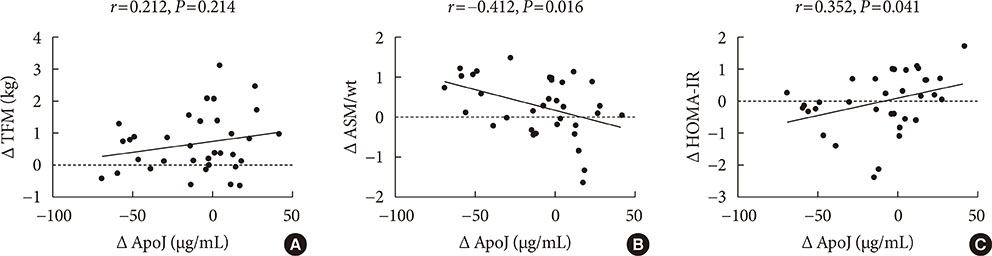
In the EXE group, ApoJ levels decreased 26.3% and 19.4%, relative to baseline, at 8 and 12 weeks, respectively. Between-group differences were significant at 8 and 12 weeks (P<0.05 and P<0.001, respectively). In the EXE group, 12 weeks of exercise resulted in significant decreases in body weight, percent body fat, and HOMA-IR indices. Concurrently, weight-adjusted appendicular skeletal muscle mass (ASM/wt) was increased in the EXE group compared with the CON group. Importantly, changes in the ApoJ level were significantly correlated with changes in ASM/wt.
CONCLUSION
Exercise training resulted in a significant decrease in the circulating ApoJ level, with changes in ApoJ associated with an improvement in some insulin resistance indices. These data suggest that circulating ApoJ may be a useful metabolic marker for assessing the effects of exercise on insulin resistance.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Impact of Skeletal Muscle Mass on Metabolic Health
Gyuri Kim, Jae Hyeon Kim
Endocrinol Metab. 2020;35(1):1-6. doi: 10.3803/EnM.2020.35.1.1.
Reference
-
1. Danaei G, Finucane MM, Lu Y, Singh GM, Cowan MJ, Paciorek CJ, Lin JK, Farzadfar F, Khang YH, Stevens GA, Rao M, Ali MK, Riley LM, Robinson CA, Ezzati M. Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group (Blood Glucose). National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2·7 million participants. Lancet. 2011; 378:31–40.
Article2. Miller BR, Nguyen H, Hu CJ, Lin C, Nguyen QT. New and emerging drugs and targets for type 2 diabetes: reviewing the evidence. Am Health Drug Benefits. 2014; 7:452–463.3. Wilcox G. Insulin and insulin resistance. Clin Biochem Rev. 2005; 26:19–39.4. Kim YB, Nikoulina SE, Ciaraldi TP, Henry RR, Kahn BB. Normal insulin-dependent activation of Akt/protein kinase B, with diminished activation of phosphoinositide 3-kinase, in muscle in type 2 diabetes. J Clin Invest. 1999; 104:733–741.
Article5. Trougakos IP, Gonos ES. Clusterin/apolipoprotein J in human aging and cancer. Int J Biochem Cell Biol. 2002; 34:1430–1448.
Article6. Miwa Y, Takiuchi S, Kamide K, Yoshii M, Horio T, Tanaka C, Banno M, Miyata T, Sasaguri T, Kawano Y. Insertion/deletion polymorphism in clusterin gene influences serum lipid levels and carotid intima-media thickness in hypertensive Japanese females. Biochem Biophys Res Commun. 2005; 331:1587–1593.
Article7. Thambisetty M, Simmons A, Velayudhan L, Hye A, Campbell J, Zhang Y, Wahlund LO, Westman E, Kinsey A, Guntert A, Proitsi P, Powell J, Causevic M, Killick R, Lunnon K, Lynham S, Broadstock M, Choudhry F, Howlett DR, Williams RJ, Sharp SI, Mitchelmore C, Tunnard C, Leung R, Foy C, O'Brien D, Breen G, Furney SJ, Ward M, Kloszewska I, Mecocci P, Soininen H, Tsolaki M, Vellas B, Hodges A, Murphy DG, Parkins S, Richardson JC, Resnick SM, Ferrucci L, Wong DF, Zhou Y, Muehlboeck S, Evans A, Francis PT, Spenger C, Lovestone S. Association of plasma clusterin concentration with severity, pathology, and progression in Alzheimer disease. Arch Gen Psychiatry. 2010; 67:739–748.
Article8. Bi J, Guo AL, Lai YR, Li B, Zhong JM, Wu HQ, Xie Z, He YL, Lv ZL, Lau SH, Wang Q, Huang XH, Zhang LJ, Wen JM, Guan XY. Overexpression of clusterin correlates with tumor progression, metastasis in gastric cancer: a study on tissue microarrays. Neoplasma. 2010; 57:191–197.
Article9. Won JC, Park CY, Oh SW, Lee ES, Youn BS, Kim MS. Plasma clusterin (ApoJ) levels are associated with adiposity and systemic inflammation. PLoS One. 2014; 9:e103351.
Article10. Baralla A, Sotgiu E, Deiana M, Pasella S, Pinna S, Mannu A, Canu E, Sotgiu G, Ganau A, Zinellu A, Sotgia S, Carru C, Deiana L. Plasma clusterin and lipid profile: a link with aging and cardiovascular diseases in a population with a consistent number of centenarians. PLoS One. 2015; 10:e0128029.
Article11. Hoofnagle AN, Wu M, Gosmanova AK, Becker JO, Wijsman EM, Brunzell JD, Kahn SE, Knopp RH, Lyons TJ, Heinecke JW. Low clusterin levels in high-density lipoprotein associate with insulin resistance, obesity, and dyslipoproteinemia. Arterioscler Thromb Vasc Biol. 2010; 30:2528–2534.
Article12. Seo JA, Kang MC, Ciaraldi TP, Kim SS, Park KS, Choe C, Hwang WM, Lim DM, Farr O, Mantzoros C, Henry RR, Kim YB. Circulating ApoJ is closely associated with insulin resistance in human subjects. Metabolism. 2018; 78:155–166.
Article13. Zanuso S, Jimenez A, Pugliese G, Corigliano G, Balducci S. Exercise for the management of type 2 diabetes: a review of the evidence. Acta Diabetol. 2010; 47:15–22.
Article14. Oliveira C, Simoes M, Carvalho J, Ribeiro J. Combined exercise for people with type 2 diabetes mellitus: a systematic review. Diabetes Res Clin Pract. 2012; 98:187–198.
Article15. Colberg SR, Sigal RJ, Fernhall B, Regensteiner JG, Blissmer BJ, Rubin RR, Chasan-Taber L, Albright AL, Braun B. American College of Sports Medicine. American Diabetes Association. Exercise and type 2 diabetes: the American College of Sports Medicine and the American Diabetes Association: joint position statement executive summary. Diabetes Care. 2010; 33:2692–2696.
Article16. Way KL, Hackett DA, Baker MK, Johnson NA. The effect of regular exercise on insulin sensitivity in type 2 diabetes mellitus: a systematic review and meta-analysis. Diabetes Metab J. 2016; 40:253–271.
Article17. Kim HJ, Lee S, Kim TW, Kim HH, Jeon TY, Yoon YS, Oh SW, Kwak H, Lee JG. Effects of exercise-induced weight loss on acylated and unacylated ghrelin in overweight children. Clin Endocrinol (Oxf). 2008; 68:416–422.
Article18. Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985; 28:412–419.19. Trougakos IP, Poulakou M, Stathatos M, Chalikia A, Melidonis A, Gonos ES. Serum levels of the senescence biomarker clusterin/apolipoprotein J increase significantly in diabetes type II and during development of coronary heart disease or at myocardial infarction. Exp Gerontol. 2002; 37:1175–1187.
Article20. Arnold T, Brandlhofer S, Vrtikapa K, Stangl H, Hermann M, Zwiauer K, Mangge H, Karwautz A, Huemer J, Koller D, Schneider WJ, Strobl W. Effect of obesity on plasma clusterin, [corrected] a proposed modulator of leptin action. Pediatr Res. 2011; 69:237–242.21. Navab M, Anantharamaiah GM, Reddy ST, Van Lenten BJ, Wagner AC, Hama S, Hough G, Bachini E, Garber DW, Mishra VK, Palgunachari MN, Fogelman AM. An oral apoJ peptide renders HDL antiinflammatory in mice and monkeys and dramatically reduces atherosclerosis in apolipoprotein E-null mice. Arterioscler Thromb Vasc Biol. 2005; 25:1932–1937.
Article22. Choi KM. Sarcopenia and sarcopenic obesity. Korean J Intern Med. 2016; 31:1054–1060.
Article23. Jang HC. Sarcopenia, frailty, and diabetes in older adults. Diabetes Metab J. 2016; 40:182–189.
Article24. Kang ES, Yun YS, Park SW, Kim HJ, Ahn CW, Song YD, Cha BS, Lim SK, Kim KR, Lee HC. Limitation of the validity of the homeostasis model assessment as an index of insulin resistance in Korea. Metabolism. 2005; 54:206–211.
Article25. DeFronzo RA, Tobin JD, Andres R. Glucose clamp technique: a method for quantifying insulin secretion and resistance. Am J Physiol. 1979; 237:E214–E223.
Article26. Rull A, Martinez-Bujidos M, Perez-Cuellar M, Perez A, Ordonez-Llanos J, Sanchez-Quesada JL. Increased concentration of clusterin/apolipoprotein J (apoJ) in hyperlipemic serum is paradoxically associated with decreased apoJ content in lipoproteins. Atherosclerosis. 2015; 241:463–470.
Article27. Aronis KN, Vamvini MT, Chamberland JP, Mantzoros CS. Circulating clusterin (apolipoprotein J) levels do not have any day/night variability and are positively associated with total and LDL cholesterol levels in young healthy individuals. J Clin Endocrinol Metab. 2011; 96:E1871–E1875.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Exercise on Glucose Metabolism
- Exercise therapy for diabetes mellitus
- Letter: The Effect of 12 Weeks Aerobic, Resistance, and Combined Exercises on Omentin-1 Levels and Insulin Resistance among Type 2 Diabetic Middle-Aged Women (Diabetes Metab J 2017;41:205-12)
- Effect of Exercise on Cardiovascular Disease in Patients with Diabetes Mellitus (Aerobic vs. Resistance)
- Exercise in the Elderly with Diabetes