J Korean Orthop Assoc.
2020 Feb;55(1):54-61. 10.4055/jkoa.2020.55.1.54.
Diagnosis and Treatment of Brown Tumor
- Affiliations
-
- 1Department of Orthopedic Surgery, Chosun University College of Medicine, Gwangju, Korea.
- 2Department of Orthopedic Surgery, Chonnam National University College of Medicine, Gwangju, Korea. stjung@chonnam.ac.kr
- KMID: 2470769
- DOI: http://doi.org/10.4055/jkoa.2020.55.1.54
Abstract
- PURPOSE
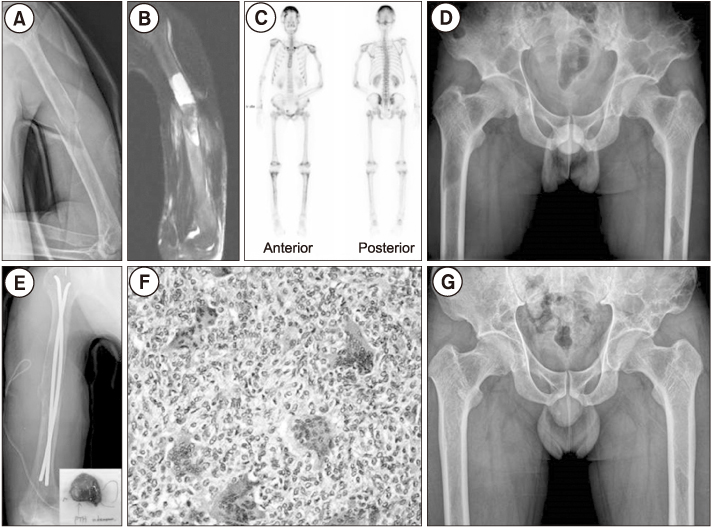
Brown tumor is a tumor-like disease that can occur as a linked disease of hyperparathyroidism which can causes osteoporosis, osteitis fibrosa cystica, pathologic fractures. Brown tumor has been reported as a case report, but there is no comprehensive report on the exact diagnosis and principle of management for osseous lesion. The purpose of this study is to report the treatment and results of osseous lesions through 5 cases.
MATERIALS AND METHODS
From February 2004 to May 2015, five cases of Brown tumor were diagnosed in Chosun University Hospital and Chonnam National University Hospital orthopedic department. Medical records and radiographs were reviewed retrospectively. Parathyroid tumors were surgically removed, and surgical treatment and observation were performed for orthopedic osseous lesions.
RESULTS
The mean length of the long axis of the symptomatic osseous lesion was 6.2 cm (4.5-9.0 cm). An average of 7.6 (range, 3 to 14) of high uptake osseous lesion showed in whole body bone scan. The absolute value, T-score and Z-score of the vertebrae and proximal femur were adequate for diagnosis of osteoporosis using dual energy X-ray absorptiometry bone mineral density at diagnosis and recovered to normal at the last follow-up. In laboratory tests, serum concentrations of total calcium, ionized calcium, inorganic phosphorus, serum alkaline phosphatase, and parathyroid hormone were helpful to diagnosis and normalized upon successful removal of parathyroid adenoma or cancer.
CONCLUSION
For accurate diagnosis of Brown tumor, it should be accompanied by systemic examination as well as clinical symptoms, laboratory tests and radiologic examination for osseous lesions. And a good prognosis can be expected if the hyperparathyroidism is treated together with the comprehensive treatment of osseous lesions.
MeSH Terms
-
Absorptiometry, Photon
Alkaline Phosphatase
Bone Density
Calcium
Diagnosis*
Femur
Follow-Up Studies
Fractures, Spontaneous
Hyperparathyroidism
Jeollanam-do
Medical Records
Orthopedics
Osteitis Fibrosa Cystica
Osteoporosis
Parathyroid Hormone
Parathyroid Neoplasms
Phosphorus
Prognosis
Retrospective Studies
Spine
Alkaline Phosphatase
Calcium
Parathyroid Hormone
Phosphorus
Figure
Reference
-
1. Khan AA, Hanley DA, Rizzoli R, et al. Primary hyperparathyroidism: review and recommendations on evaluation, diagnosis, and management. A Canadian and international consensus. Osteoporos Int. 2017; 28:1–19.
Article2. Bandeira F, Cusano NE, Silva BC, et al. Bone disease in primary hyperparathyroidism. Arq Bras Endocrinol Metabol. 2014; 58:553–561.
Article3. Zou H, Song L, Jia M, Wang L, Sun Y. Brown tumor of multiple facial bones associated with primary hyperparathyroidism: a clinical case report. Medicine (Baltimore). 2018; 97:e11877.4. Ruggeri RM, Calamoneri E, Russo A, et al. Supra-acetabular brown tumor due to primary hyperparathyroidism associated with chronic renal failure. ScientificWorldJournal. 2010; 10:799–805.
Article5. Qaisi M, Loeb M, Montague L, Caloss R. Mandibular brown tumor of secondary hyperparathyroidism requiring extensive resection: a forgotten entity in the developed world? Case Rep Med. 2015; 2015:567543.
Article6. Panagopoulos A, Tatani I, Kourea HP, Kokkalis ZT, Panagopoulos K, Megas P. Osteolytic lesions (brown tumors) of primary hyperparathyroidism misdiagnosed as multifocal giant cell tumor of the distal ulna and radius: a case report. J Med Case Rep. 2018; 12:176.
Article7. Carvalho R, Kurochka S, Rocha J, Fernandes JS. Brown tumor of the mandible: magnetic susceptibility demonstrated by MRI. Radiol Case Rep. 2015; 7:662.
Article8. Khan A, Bilezikian J. Primary hyperparathyroidism: pathophysiology and impact on bone. CMAJ. 2000; 163:184–187.9. De Crea C, Traini E, Oragano L, Bellantone C, Raffaelli M, Lombardi CP. Are brown tumours a forgotten disease in developed countries? Acta Otorhinolaryngol Ital. 2012; 32:410–415.10. Dekaken A, Gouri A, Bentorki AA, Yakhlef A. Knee brown tumor revealing a primary hyperparathyroidism: a case report. Ann Biol Clin (Paris). 2014; 72:245–248.
Article11. Di Daniele N, Condò S, Ferrannini M, et al. Brown tumour in a patient with secondary hyperparathyroidism resistant to medical therapy: case report on successful treatment after subtotal parathyroidectomy. Int J Endocrinol. 2009; 2009:827652.
Article12. Takeshita T, Takeshita K, Abe S, Takami H, Imamura T, Furui S. Brown tumor with fluid-fluid levels in a patient with primary hyperparathyroidism: radiological findings. Radiat Med. 2006; 24:631–634.
Article13. Vera L, Dolcino M, Mora M, et al. Primary hyperparathyroidism diagnosed after surgical ablation of a costal mass mistaken for giant-cell bone tumor: a case report. J Med Case Rep. 2011; 5:596.
Article14. Fernández-Sanromán J, Antón-Badiola IM, Costas-López A. Brown tumor of the mandible as first manifestation of primary hyperparathyroidism: diagnosis and treatment. Med Oral Patol Oral Cir Bucal. 2005; 10:169–172.15. Vaishya R, Agarwal AK, Singh H, Vijay V. Multiple ‘brown tumors’ masquerading as metastatic bone disease. Cureus. 2015; 7:e431.
Article16. Mundy GR, Cove DH, Fisken R. Primary hyperparathyroidism: changes in the pattern of clinical presentation. Lancet. 1980; 1:1317–1320.
Article17. Yang CJ, Seabold JE, Gurll NJ. Brown tumor of bone: a potential source of false-positive thallium-201 localization. J Nucl Med. 1989; 30:1264–1267.18. Radulescu D, Chis B, Donca V, Munteanu V. Brown tumors of the femur and pelvis secondary to a parathyroid carcinoma: report of one case. Rev Med Chil. 2014; 142:919–923.
Article19. Loya-Solís A, Mendoza-García A, Ceceñas-Falcón L, Rodríguez-Gutiérrez R. Sphenoid brown tumor associated with a parathyroid carcinoma. Case Rep Endocrinol. 2014; 2014:837204.
Article20. Can Ö, Boynueğri B, Gökçe AM, et al. brown tumors: a case report and review of the literature. Case Rep Nephrol Dial. 2016; 6:46–52.
Article21. Aghaghazvini L, Sharifian H, Rasuli B. Primary hyperparathyroidism misdiagnosed as giant cell bone tumor of maxillary sinus: a case report. Iran J Radiol. 2016; 13:e13260.
Article22. Vaishya R, Agarwal AK, Vijay V, Vaish A. A brown tumor of tibial diaphysis masquerading as malignancy. Cureus. 2017; 9:e1319.
Article23. Su AW, Chen CF, Huang CK, Chen PC, Chen WM, Chen TH. Primary hyperparathyroidism with brown tumor mimicking metastatic bone malignancy. J Chin Med Assoc. 2010; 73:177–180.
Article24. Meydan N, Barutca S, Guney E, et al. Brown tumors mimicking bone metastases. J Natl Med Assoc. 2006; 98:950–953.25. Phulsunga RK, Parghane RV, Kanojia RK, et al. Multiple brown tumors caused by a parathyroid adenoma mimicking metastatic bone disease from giant cell tumor. World J Nucl Med. 2016; 15:56–58.
Article26. Mori H, Okada Y, Arao T, Shimaziri S, Tanaka Y. A case of multiple brown tumors with primary hyperparathyroidism. J Bone Miner Metab. 2013; 31:123–127.
Article27. Casteràs A, Darder L, Zafon C, et al. Brown tumor of the jaw after pregnancy and lactation in a MEN1 patient. Endocrinol Diabetes Metab Case Rep. 2016; 2016:16-0111.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Brown Tumor of The Spine with Compression Fracture: A Case Report
- A Case of Brown Tumor of the Hard Palate in Association with Primary Hyperparathyroidism
- Brown Tumor of the Thoracic Spine: First Manifestation of Primary Hyperparathyroidism
- Brown Tumor of the Cervical Spines: A Case Report with Literature Review
- A Case of Brown Tumor of the Mandible Caused by Hyperparathyroidism