Korean J Radiol.
2017 Feb;18(1):249-259. 10.3348/kjr.2017.18.1.249.
Diagnosis of Nerve Root Compromise of the Lumbar Spine: Evaluation of the Performance of Three-dimensional Isotropic T2-weighted Turbo Spin-Echo SPACE Sequence at 3T
- Affiliations
-
- 1Department of Radiology, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul 06591, Korea. whjee12@gmail.com
- 2Department of Neurosurgery, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul 06591, Korea.
- 3Department of Orthopedic Surgery, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul 06591, Korea.
- KMID: 2468137
- DOI: http://doi.org/10.3348/kjr.2017.18.1.249
Abstract
OBJECTIVE
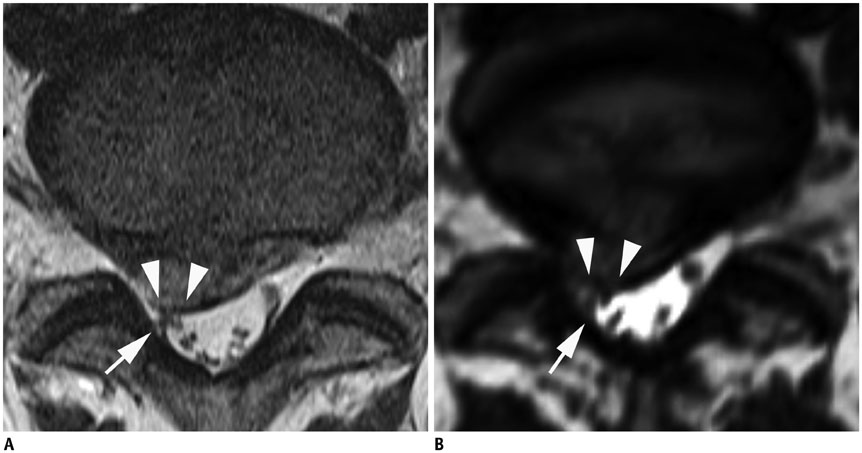
To explore the performance of three-dimensional (3D) isotropic T2-weighted turbo spin-echo (TSE) sampling perfection with application optimized contrasts using different flip angle evolution (SPACE) sequence on a 3T system, for the evaluation of nerve root compromise by disc herniation or stenosis from central to extraforaminal location of the lumbar spine, when used alone or in combination with conventional two-dimensional (2D) TSE sequence.
MATERIALS AND METHODS
Thirty-seven patients who had undergone 3T spine MRI including 2D and 3D sequences, and had subsequent spine surgery for nerve root compromise at a total of 39 nerve levels, were analyzed. A total of 78 nerve roots (48 symptomatic and 30 asymptomatic sites) were graded (0 to 3) using different MRI sets of 2D, 3D (axial plus sagittal), 3D (all planes), and combination of 2D and 3D sequences, with respect to the nerve root compromise caused by posterior disc herniations, lateral recess stenoses, neural foraminal stenoses, or extraforaminal disc herniations; grading was done independently by two readers. Diagnostic performance was compared between different imaging sets using the receiver operating characteristics (ROC) curve analysis.
RESULTS
There were no statistically significant differences (p = 0.203 to > 0.999) in the ROC curve area between the imaging sets for both readers 1 and 2, except for combined 2D and 3D (0.843) vs. 2D (0.802) for reader 1 (p = 0.035), and combined 2D and 3D (0.820) vs. 3D including all planes (0.765) for reader 2 (p = 0.049).
CONCLUSION
The performance of 3D isotropic T2-weighted TSE sequence of the lumbar spine, whether axial plus sagittal images, or all planes of images, was not significantly different from that of 2D TSE sequences, for the evaluation of nerve root compromise of the lumbar spine. Combining 2D and 3D might possibly improve the diagnostic accuracy compared with either one.
Keyword
MeSH Terms
-
Adult
Aged
Area Under Curve
Constriction, Pathologic/*diagnosis/diagnostic imaging
Contrast Media/chemistry
Female
Humans
Image Interpretation, Computer-Assisted
Imaging, Three-Dimensional
Intervertebral Disc Displacement/*diagnosis/diagnostic imaging
Lumbar Vertebrae/*diagnostic imaging
Magnetic Resonance Imaging
Male
Middle Aged
ROC Curve
Young Adult
Figure
Cited by 2 articles
-
Age of Data in Contemporary Research Articles Published in Representative General Radiology Journals
Ji Hun Kang, Dong Hwan Kim, Seong Ho Park, Jung Hwan Baek
Korean J Radiol. 2018;19(6):1172-1178. doi: 10.3348/kjr.2018.19.6.1172.Revalidating Pfirrmann's Magnetic Resonance Image-Based Grading of Lumbar Nerve Root Compromise by Calculating Reliability among Orthopaedic Residents
Arun-Kumar Kaliya-Perumal, Senthil-Kumar Ariputhiran-Tamilselvam, Chi-An Luo, Sivaharivelan Thiagarajan, Udhayakumar Selvam, Raj-Prabhakar Sumathi-Edirolimanian
Clin Orthop Surg. 2018;10(2):210-215. doi: 10.4055/cios.2018.10.2.210.
Reference
-
1. Naraghi A, White LM. Three-dimensional MRI of the musculoskeletal system. AJR Am J Roentgenol. 2012; 199:W283–W293.2. Lichy MP, Wietek BM, Mugler JP 3rd, Horger W, Menzel MI, Anastasiadis A, et al. Magnetic resonance imaging of the body trunk using a single-slab, 3-dimensional, T2-weighted turbo-spin-echo sequence with high sampling efficiency (SPACE) for high spatial resolution imaging: initial clinical experiences. Invest Radiol. 2005; 40:754–760.3. Gold GE, Busse RF, Beehler C, Han E, Brau AC, Beatty PJ, et al. Isotropic MRI of the knee with 3D fast spin-echo extended echo-train acquisition (XETA): initial experience. AJR Am J Roentgenol. 2007; 188:1287–1293.4. Stevens KJ, Busse RF, Han E, Brau AC, Beatty PJ, Beaulieu CF, et al. Ankle: isotropic MR imaging with 3D-FSE-cube--initial experience in healthy volunteers. Radiology. 2008; 249:1026–1033.5. Jung JY, Yoon YC, Kwon JW, Ahn JH, Choe BK. Diagnosis of internal derangement of the knee at 3.0-T MR imaging: 3D isotropic intermediate-weighted versus 2D sequences. Radiology. 2009; 253:780–787.6. Kijowski R, Davis KW, Woods MA, Lindstrom MJ, De Smet AA, Gold GE, et al. Knee joint: comprehensive assessment with 3D isotropic resolution fast spin-echo MR imaging--diagnostic performance compared with that of conventional MR imaging at 3.0 T. Radiology. 2009; 252:486–495.7. Choo HJ, Lee SJ, Kim OH, Seo SS, Kim JH. Comparison of three-dimensional isotropic T1-weighted fast spin-echo MR arthrography with two-dimensional MR arthrography of the shoulder. Radiology. 2012; 262:921–931.8. Jung JY, Jee WH, Park MY, Lee SY, Kim YS. SLAP tears: diagnosis using 3-T shoulder MR arthrography with the 3D isotropic turbo spin-echo space sequence versus conventional 2D sequences. Eur Radiol. 2013; 23:487–495.9. Kwon JW, Yoon YC, Choi SH. Three-dimensional isotropic T2-weighted cervical MRI at 3T: comparison with two-dimensional T2-weighted sequences. Clin Radiol. 2012; 67:106–113.10. Meindl T, Wirth S, Weckbach S, Dietrich O, Reiser M, Schoenberg SO. Magnetic resonance imaging of the cervical spine: comparison of 2D T2-weighted turbo spin echo, 2D T2*weighted gradient-recalled echo and 3D T2-weighted variable flip-angle turbo spin echo sequences. Eur Radiol. 2009; 19:713–721.11. Rodegerdts EA, Boss A, Riemarzik K, Lichy M, Schick F, Claussen CD, et al. 3D imaging of the whole spine at 3T compared to 1.5T: initial experiences. Acta Radiol. 2006; 47:488–493.12. Tins B, Cassar-Pullicino V, Haddaway M, Nachtrab U. Three-dimensional sampling perfection with application-optimised contrasts using a different flip angle evolutions sequence for routine imaging of the spine: preliminary experience. Br J Radiol. 2012; 85:e480–e489.13. Blizzard DJ, Haims AH, Lischuk AW, Arunakul R, Hustedt JW, Grauer JN. 3D-FSE isotropic MRI of the lumbar spine: novel application of an existing technology. J Spinal Disord Tech. 2015; 28:152–157.14. Fu MC, Buerba RA, Neway WE 3rd, Brown JE, Trivedi M, Lischuk AW, et al. Three-dimensional isotropic MRI of the cervical spine: a diagnostic comparison with conventional MRI. Clin Spine Surg. 2016; 29:66–71.15. Lee S, Jee WH, Jung JY, Lee SY, Ryu KS, Ha KY. MRI of the lumbar spine: comparison of 3D isotropic turbo spin-echo SPACE sequence versus conventional 2D sequences at 3.0 T. Acta Radiol. 2015; 56:174–181.16. Lee GY, Lee JW, Choi HS, Oh KJ, Kang HS. A new grading system of lumbar central canal stenosis on MRI: an easy and reliable method. Skeletal Radiol. 2011; 40:1033–1039.17. Schizas C, Theumann N, Burn A, Tansey R, Wardlaw D, Smith FW, et al. Qualitative grading of severity of lumbar spinal stenosis based on the morphology of the dural sac on magnetic resonance images. Spine (Phila Pa 1976). 2010; 35:1919–1924.18. Lee S, Lee JW, Yeom JS, Kim KJ, Kim HJ, Chung SK, et al. A practical MRI grading system for lumbar foraminal stenosis. AJR Am J Roentgenol. 2010; 194:1095–1098.19. Bartynski WS, Lin L. Lumbar root compression in the lateral recess: MR imaging, conventional myelography, and CT myelography comparison with surgical confirmation. AJNR Am J Neuroradiol. 2003; 24:348–360.20. Pfirrmann CW, Dora C, Schmid MR, Zanetti M, Hodler J, Boos N. MR image-based grading of lumbar nerve root compromise due to disk herniation: reliability study with surgical correlation. Radiology. 2004; 230:583–588.21. Tong HC, Haig AJ, Yamakawa KS, Miner JA. Specificity of needle electromyography for lumbar radiculopathy and plexopathy in 55- to 79-year-old asymptomatic subjects. Am J Phys Med Rehabil. 2006; 85:908–912. quiz 913-915, 934.22. Landis JR, Koch GG. An application of hierarchical kappa-type statistics in the assessment of majority agreement among multiple observers. Biometrics. 1977; 33:363–374.23. Mikhael MA, Ciric I, Tarkington JA, Vick NA. Neuroradiological evaluation of lateral recess syndrome. Radiology. 1981; 140:97–107.24. Busse RF, Hariharan H, Vu A, Brittain JH. Fast spin echo sequences with very long echo trains: design of variable refocusing flip angle schedules and generation of clinical T2 contrast. Magn Reson Med. 2006; 55:1030–1037.25. Genevay S, Atlas SJ. Lumbar spinal stenosis. Best Pract Res Clin Rheumatol. 2010; 24:253–265.26. Beattie PF, Meyers SP, Stratford P, Millard RW, Hollenberg GM. Associations between patient report of symptoms and anatomic impairment visible on lumbar magnetic resonance imaging. Spine (Phila Pa 1976). 2000; 25:819–828.27. Weishaupt D, Zanetti M, Hodler J, Boos N. MR imaging of the lumbar spine: prevalence of intervertebral disk extrusion and sequestration, nerve root compression, end plate abnormalities, and osteoarthritis of the facet joints in asymptomatic volunteers. Radiology. 1998; 209:661–666.28. Modic MT, Obuchowski NA, Ross JS, Brant-Zawadzki MN, Grooff PN, Mazanec DJ, et al. Acute low back pain and radiculopathy: MR imaging findings and their prognostic role and effect on outcome. Radiology. 2005; 237:597–604.29. Siebert E, Prüss H, Klingebiel R, Failli V, Einhäupl KM, Schwab JM. Lumbar spinal stenosis: syndrome, diagnostics and treatment. Nat Rev Neurol. 2009; 5:392–403.30. Lee IS, Kim HJ, Lee JS, Moon TY, Jeon UB. Extraforaminal with or without foraminal disk herniation: reliable MRI findings. AJR Am J Roentgenol. 2009; 192:1392–1396.31. Mamisch N, Brumann M, Hodler J, Held U, Brunner F, Steurer J. Lumbar Spinal Stenosis Outcome Study Working Group Zurich. Radiologic criteria for the diagnosis of spinal stenosis: results of a Delphi survey. Radiology. 2012; 264:174–179.32. Andreisek G, Hodler J, Steurer J. Uncertainties in the diagnosis of lumbar spinal stenosis. Radiology. 2011; 261:681–684.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnosis of Rotator Cuff Tears with Non-Arthrographic MR Imaging: 3D Fat-Suppressed Isotropic Intermediate-Weighted Turbo Spin-Echo Sequence versus Conventional 2D Sequences at 3T
- Usefulness of Fluid Attenuated Inve rsion Re c overy(FLAIR) Image
- The Comparison between Single Shot Turbo Spin Echo and B-FFE (Balanced Turbo Field-echo) in the Differentiation of Focal Liver Lesions
- Utility of Two Types of MR Cisternography for Patency Evaluation of Aqueduct and Third Ventriculostomy Site: Three Dimensional Sagittal Fast Spin Echo Sequence and Steady-State Coherent Fast Gradient Echo Sequence
- Usefulness of CISS Technique in the MR Imaging Diagnosis of Intraocular Lesions