Infect Chemother.
2019 Dec;51(4):376-385. 10.3947/ic.2019.51.4.376.
The Cefazolin Inoculum Effect and the Presence of type A blaZ Gene according to agr Genotype in Methicillin-Susceptible Staphylococcus aureus Bacteremia
- Affiliations
-
- 1Department of Internal Medicine, Pusan National University School of Medicine and Medical Research Institute, Pusan National University Hospital, Busan, Korea. ebenezere.lee@gmail.com
- KMID: 2466470
- DOI: http://doi.org/10.3947/ic.2019.51.4.376
Abstract
- BACKGROUND
Recent data suggests the inoculum effect of methicillin-susceptible Staphylococcus aureus (MSSA) against beta-lactam antibiotics and their association with functionality or genotypic variation of agr locus.
METHODS
MSSA blood isolates were collected at a tertiary care hospital in Korea from June 2014 to December 2017. The functionality of the agr operon was measured by δ-hemolysin assays. Multiplex PCR was performed to determine the agr genotype. The cefazolin minimum inhibitory concentrations (MICs) at a high inoculum concentration (~5 × 10ⷠCFU/ml) were compared to the MICs at a standard inoculum concentration (~5 × 10ⵠCFU/ml) to identify strains with the cefazolin inoculum effect (CIE). The DNA sequencing of blaZ gene was performed to classify the blaZ genotype.
RESULTS
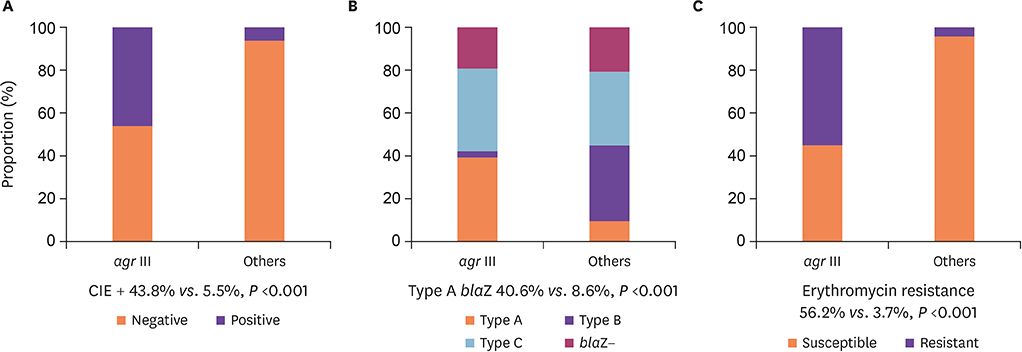
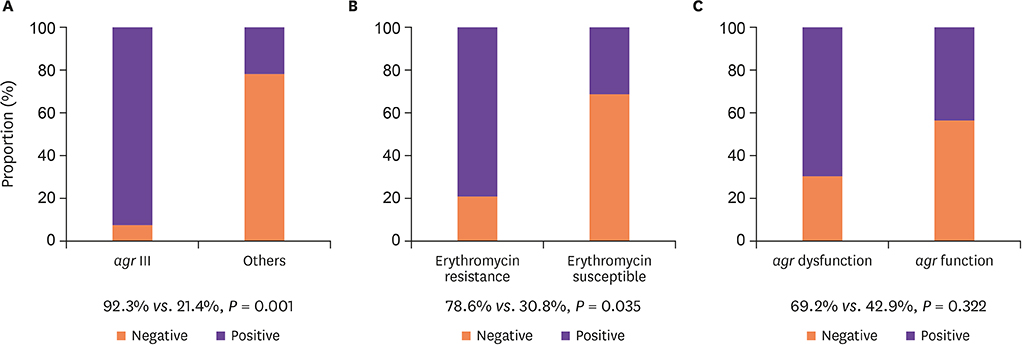
Among the 195 MSSA blood isolates, agr genotype I was most common (68.2%), followed by type III (16.4%), type IV (9.2%), and type II (6.2%). Sixty-seven (34.3%) MSSA isolates had dysfunctional agr, but neither CIE nor blaZ genotype was associated with dysfunctional agr. The MSSA with agr type III genotype exhibited significantly higher CIE positivity (agr III 43.8% vs. non-agr III 5.5%, P <0.01) and erythromycin/clindamycin resistance. In the subgroup analysis of type A blaZ possessing MSSA, almost all of the agr III MSSA isolates exhibited CIE, while only 20% of non-agr III isolates had CIE (P <0.01).
CONCLUSION
In MSSA blood isolates, CIE might be associated with agr genotype rather than with dysfunctional agr.
MeSH Terms
Figure
Reference
-
1. Nannini EC, Singh KV, Murray BE. Relapse of type A beta-lactamase-producing Staphylococcus aureus native valve endocarditis during cefazolin therapy: revisiting the issue. Clin Infect Dis. 2003; 37:1194–1198.
Article2. Brook I. Inoculum effect. Rev Infect Dis. 1989; 11:361–368.
Article3. Nannini EC, Stryjewski ME, Singh KV, Bourgogne A, Rude TH, Corey GR, Fowler VG Jr, Murray BE. Inoculum effect with cefazolin among clinical isolates of methicillin-susceptible Staphylococcus aureus: frequency and possible cause of cefazolin treatment failure. Antimicrob Agents Chemother. 2009; 53:3437–3441.
Article4. Lee S, Kwon KT, Kim HI, Chang HH, Lee JM, Choe PG, Park WB, Kim NJ, Oh MD, Song DY, Kim SW. Clinical implications of cefazolin inoculum effect and beta-lactamase type on methicillin-susceptible Staphylococcus aureus bacteremia. Microb Drug Resist. 2014; 20:568–574.
Article5. Nannini EC, Singh KV, Arias CA, Murray BE. In vivo effect of cefazolin, daptomycin, and nafcillin in experimental endocarditis with a methicillin-susceptible Staphylococcus aureus strain showing an inoculum effect against cefazolin. Antimicrob Agents Chemother. 2013; 57:4276–4281.
Article6. Shin HH, Han S, Yim DS, Lee DG, Park C, Kim SH, Kwon JC, Hong KW, Park SH, Choi SM, Choi JH, Yoo JH. Efficacy of vancomycin against Staphylococcus aureus according to inoculum size in a neutropenic mouse infection model. Infect Chemother. 2011; 43:251–257.
Article7. Lee S, Choe PG, Song KH, Park SW, Kim HB, Kim NJ, Kim EC, Park WB, Oh MD. Is cefazolin inferior to nafcillin for treatment of methicillin-susceptible Staphylococcus aureus bacteremia? Antimicrob Agents Chemother. 2011; 55:5122–5126.
Article8. Oh WS, Moon C, Chung JW, Choo EJ, Kwak YG, Kim SH, Ryu SY, Park SY, Kim BN. Antibiotic treatment of vertebral osteomyelitis caused by methicillin-susceptible Staphylococcus aureus: a focus on the use of oral beta-lactams. Infect Chemother. 2019; 51:284–294.
Article9. Painter KL, Krishna A, Wigneshweraraj S, Edwards AM. What role does the quorum-sensing accessory gene regulator system play during Staphylococcus aureus bacteremia? Trends Microbiol. 2014; 22:676–685.
Article10. Singh R, Ray P. Quorum sensing-mediated regulation of staphylococcal virulence and antibiotic resistance. Future Microbiol. 2014; 9:669–681.
Article11. Fowler VG Jr, Sakoulas G, McIntyre LM, Meka VG, Arbeit RD, Cabell CH, Stryjewski ME, Eliopoulos GM, Reller LB, Corey GR, Jones T, Lucindo N, Yeaman MR, Bayer AS. Persistent bacteremia due to methicillin-resistant Staphylococcus aureus infection is associated with agr dysfunction and low-level in vitro resistance to thrombin-induced platelet microbicidal protein. J Infect Dis. 2004; 190:1140–1149.
Article12. Kang CK, Cho JE, Choi YJ, Jung Y, Kim NH, Kim CJ, Kim TS, Song KH, Choe PG, Park WB, Bang JH, Kim ES, Park KU, Park SW, Kim NJ, Oh MD, Kim HB. agr dysfunction affects staphylococcal cassette chromosome mec type-dependent clinical outcomes in methicillin-resistant Staphylococcus aureus bacteremia. Antimicrob Agents Chemother. 2015; 59:3125–3132.
Article13. Park SY, Chong YP, Park HJ, Park KH, Moon SM, Jeong JY, Kim MN, Kim SH, Lee SO, Choi SH, Woo JH, Kim YS. agr Dysfunction and persistent methicillin-resistant Staphylococcus aureus bacteremia in patients with removed eradicable foci. Infection. 2013; 41:111–119.
Article14. Schweizer ML, Furuno JP, Sakoulas G, Johnson JK, Harris AD, Shardell MD, McGregor JC, Thom KA, Perencevich EN. Increased mortality with accessory gene regulator (agr) dysfunction in Staphylococcus aureus among bacteremic patients. Antimicrob Agents Chemother. 2011; 55:1082–1087.
Article15. Castón JJ, González-Gasca F, Porras L, Illescas S, Romero MD, Gijón J. High vancomycin minimum inhibitory concentration is associated with poor outcome in patients with methicillin-susceptible Staphylococcus aureus bacteremia regardless of treatment. Scand J Infect Dis. 2014; 46:783–786.
Article16. San-Juan R, Viedma E, Chaves F, Lalueza A, Fortún J, Loza E, Pujol M, Ardanuy C, Morales I, de Cueto M, Resino-Foz E, Morales-Cartagena A, Rico A, Romero MP, Orellana MÁ, López-Medrano F, Fernández-Ruiz M, Aguado JM. High MICs for vancomycin and daptomycin and complicated catheter-related bloodstream infections with methicillin-sensitive Staphylococcus aureus . Emerg Infect Dis. 2016; 22:1057–1066.
Article17. Sullivan SB, Austin ED, Stump S, Mathema B, Whittier S, Lowy FD, Uhlemann AC. Reduced vancomycin susceptibility of methicillin-susceptible Staphylococcus aureus has no significant impact on mortality but results in an increase in complicated infection. Antimicrob Agents Chemother. 2017; 61:pii: e00316-17.18. Viedma E, Sanz F, Orellana MA, San Juan R, Aguado JM, Otero JR, Chaves F. Relationship between agr dysfunction and reduced vancomycin susceptibility in methicillin-susceptible Staphylococcus aureus causing bacteraemia. J Antimicrob Chemother. 2014; 69:51–58.
Article19. Kok EY, Vallejo JG, Sommer LM, Rosas L, Kaplan SL, Hulten KG, McNeil JC. Association of vancomycin MIC and molecular characteristics with clinical outcomes in methicillin-susceptible Staphylococcus aureus acute hematogenous osteoarticular infections in children. Antimicrob Agents Chemother. 2018; 62:e00084–18.20. Wi YM, Park YK, Moon C, Ryu SY, Lee H, Ki HK, Cheong HS, Son JS, Lee JS, Kwon KT, Kim JM, Ha YE, Kang CI, Ko KS, Chung DR, Peck KR, Song JH. The cefazolin inoculum effect in methicillin-susceptible Staphylococcus aureus blood isolates: their association with dysfunctional accessory gene regulator (agr). Diagn Microbiol Infect Dis. 2015; 83:286–291.
Article21. Clinical and Laboratory Standards Institute (CLSI). Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically; approved standard. 7th ed. Wayne, PA: CLSI;2008.22. Kernodle DS, McGraw PA, Stratton CW, Kaiser AB. Use of extracts versus whole-cell bacterial suspensions in the identification of Staphylococcus aureus beta-lactamase variants. Antimicrob Agents Chemother. 1990; 34:420–425.
Article23. Song KH, Jung SI, Lee S, Park S, Kiem SM, Lee SH, Kwak YG, Kim YK, Jang HC, Kim YS, Kim HI, Kim CJ, Park KH, Kim NJ, Oh MD, Kim HB; The Korea INfectious Diseases (KIND) study group. Characteristics of cefazolin inoculum effect-positive methicillin-susceptible Staphylococcus aureus infection in a multicentre bacteraemia cohort. Eur J Clin Microbiol Infect Dis. 2017; 36:285–294.
Article24. Voladri RK, Kernodle DS. Characterization of a chromosomal gene encoding type B beta-lactamase in phage group II isolates of Staphylococcus aureus . Antimicrob Agents Chemother. 1998; 42:3163–3168.
Article25. Sakoulas G, Eliopoulos GM, Moellering RC Jr, Wennersten C, Venkataraman L, Novick RP, Gold HS. Accessory gene regulator (agr) locus in geographically diverse Staphylococcus aureus isolates with reduced susceptibility to vancomycin. Antimicrob Agents Chemother. 2002; 46:1492–1502.
Article26. Lina G, Boutite F, Tristan A, Bes M, Etienne J, Vandenesch F. Bacterial competition for human nasal cavity colonization: role of Staphylococcal agr alleles. Appl Environ Microbiol. 2003; 69:18–23.
Article27. Livorsi DJ, Crispell E, Satola SW, Burd EM, Jerris R, Wang YF, Farley MM. Prevalence of blaZ gene types and the inoculum effect with cefazolin among bloodstream isolates of methicillin-susceptible Staphylococcus aureus . Antimicrob Agents Chemother. 2012; 56:4474–4477.
Article28. Lee SH, Park WB, Lee S, Park S, Kim SW, Lee JM, Chang HH, Kwon KT, Choe PG, Kim NJ, Kim HB, Oh MD. Association between type A blaZ gene polymorphism and cefazolin inoculum effect in methicillin-susceptible Staphylococcus aureus . Antimicrob Agents Chemother. 2016; 60:6928–6932.
Article29. Aguado JM, San-Juan R, Lalueza A, Sanz F, Rodriguez-Otero J, Gómez-Gonzalez C, Chaves F. High vancomycin MIC and complicated methicillin-susceptible Staphylococcus aureus bacteremia. Emerg Infect Dis. 2011; 17:1099–1102.
Article30. Mirani ZA, Aziz M, Khan MN, Lal I, Hassan NU, Khan SI. Biofilm formation and dispersal of Staphylococcus aureus under the influence of oxacillin. Microb Pathog. 2013; 61-62:66–72.
Article31. Pillai SK, Wennersten C, Venkataraman L, Eliopoulos GM, Moellering RC, Karchmer AW. Development of reduced vancomycin susceptibility in methicillin-susceptible Staphylococcus aureus . Clin Infect Dis. 2009; 49:1169–1174.
Article32. Cervera C, Castañeda X, de la Maria CG, del Rio A, Moreno A, Soy D, Pericas JM, Falces C, Armero Y, Almela M, Ninot S, Pare JC, Mestres CA, Gatell JM, Marco F, Miro JM; Hospital Clinic Endocarditis Study Group. Effect of vancomycin minimal inhibitory concentration on the outcome of methicillin-susceptible Staphylococcus aureus endocarditis. Clin Infect Dis. 2014; 58:1668–1675.
Article33. Holmes NE, Turnidge JD, Munckhof WJ, Robinson JO, Korman TM, O'Sullivan MV, Anderson TL, Roberts SA, Warren SJ, Coombs GW, Tan HL, Gao W, Johnson PD, Howden BP. Genetic and molecular predictors of high vancomycin MIC in Staphylococcus aureus bacteremia isolates. J Clin Microbiol. 2014; 52:3384–3393.
Article34. Ji G, Beavis R, Novick RP. Bacterial interference caused by autoinducing peptide variants. Science. 1997; 276:2027–2030.
Article35. Jarraud S, Mougel C, Thioulouse J, Lina G, Meugnier H, Forey F, Nesme X, Etienne J, Vandenesch F. Relationships between Staphylococcus aureus genetic background, virulence factors, agr groups (alleles), and human disease. Infect Immun. 2002; 70:631–641.
Article36. Jarraud S, Lyon GJ, Figueiredo AM, Lina G, Vandenesch F, Etienne J, Muir TW, Novick RP. Exfoliatin-producing strains define a fourth agr specificity group in Staphylococcus aureus . J Bacteriol. 2000; 182:6517–6522.
Article37. Rincón S, Reyes J, Carvajal LP, Rojas N, Cortés F, Panesso D, Guzmán M, Zurita J, Adachi JA, Murray BE, Nannini EC, Arias CA. Cefazolin high-inoculum effect in methicillin-susceptible Staphylococcus aureus from South American hospitals. J Antimicrob Chemother. 2013; 68:2773–2778.
Article38. Zygmunt DJ, Stratton CW, Kernodle DS. Characterization of four beta-lactamases produced by Staphylococcus aureus . Antimicrob Agents Chemother. 1992; 36:440–445.
Article39. Wright JS 3rd, Jin R, Novick RP. Transient interference with staphylococcal quorum sensing blocks abscess formation. Proc Natl Acad Sci U S A. 2005; 102:1691–1696.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prevalence and Molecular Characteristics of Methicillin-resistant Staphylococcus aureus Isolates in a Neonatal Intensive Care Unit
- Accessory Gene Regulator Polymorphism and Vancomycin Minimum Inhibitory Concentration in Methicillin-Resistant Staphylococcus aureus
- Impact of Community-Onset Methicillin-Resistant Staphylococcus aureus on Staphylococcus aureus Bacteremia in a Central Korea Veterans Health Service Hospital
- Prevalence of blaZ Gene and Performance of Phenotypic Tests to Detect Penicillinase in Staphylococcus aureus Isolates from Japan
- Detection of mecA, blaZ and aac(6')-aph(2") gene of staphylococci by PCR