Clin Endosc.
2019 Sep;52(5):472-478. 10.5946/ce.2018.152.
Effectiveness of Autologous Platelet-Rich Plasma for the Healing of Ulcers after Endoscopic Submucosal Dissection
- Affiliations
-
- 1Digestive Disease Center, CHA Bundang Medical Center, CHA University, Seongnam, Korea. cjy6695@dreamwiz.com
- 2Alanya Alaaddin Keykubat University, School of Medicine Department of Gastroenterology and Hepatology, Antalya, Turkey.
- KMID: 2464669
- DOI: http://doi.org/10.5946/ce.2018.152
Abstract
- BACKGROUND/AIMS
Platelet-rich plasma (PRP) has been used for wound healing in various medical fields. The aim of this study was to evaluate the clinical efficacy and safety of local PRP injections after endoscopic submucosal dissection (ESD).
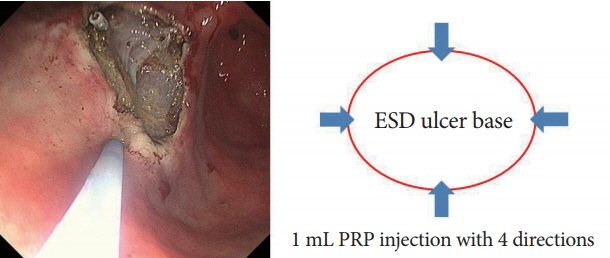
METHODS
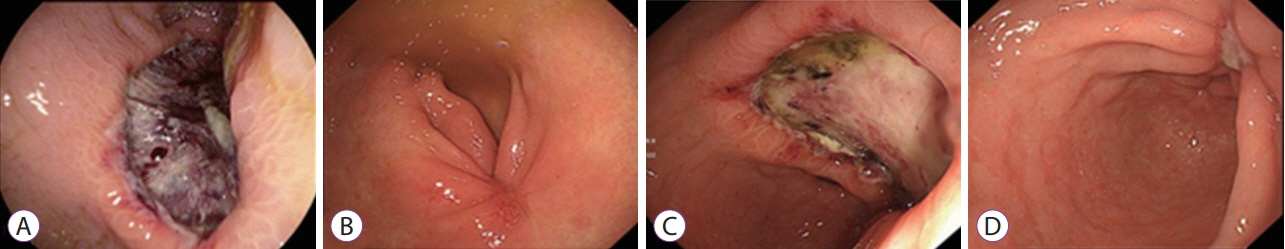
Patients were non-randomly divided into the following two groups: (1) control group in which patients were administered only an intravenous proton pump inhibitor (PPI), and (2) a study group in which patients were administered an intravenous PPI and a topical PRP injection. We assessed the reduction in the ulcer area and stage of the ulcer after the procedure (24 hours, 48 hours, and 28 days after endoscopic surgery).
RESULTS
We enrolled 7 study and 7 control patients. In the study group, the rate of ulcer reduction was 59% compared to 52% in the control group (p=0.372), 28 days after ESD. There were 5 patients in the S stage and 2 patients in the H stage in the study group compared to no patient in the S stage and 7 patients in the H stage in the control group (p=0.05), 28 days after ESD. There were no serious complications in either group.
CONCLUSIONS
The local injection of PRP is a safe and effective procedure for ulcer healing after ESD.
Figure
Cited by 2 articles
-
The Additive Effect of Platelet-Rich Plasma in the Treatment of Actively Bleeding Peptic Ulcer
Waseem M. Seleem, Amr Shaaban Hanafy
Clin Endosc. 2021;54(6):864-871. doi: 10.5946/ce.2021.004.Endless Challenges in Overcoming Complications Associated with Endoscopic Submucosal Dissection
Satoshi Ono, Shun Ito, Kenji Ogata
Clin Endosc. 2019;52(5):395-396. doi: 10.5946/ce.2019.137.
Reference
-
1. Kim DS, Jung Y, Rhee HS, et al. Usefulness of the forrest classification to predict artificial ulcer rebleeding during second-look endoscopy after endoscopic submucosal dissection. Clin Endosc. 2016; 49:273–281.
Article2. Oda I, Nonaka S, Abe S, Suzuki H, Yoshinaga S, Saito Y. Is there a need to shield ulcers after endoscopic submucosal dissection in the gastrointestinal tract? Endosc Int Open. 2015; 3:E152–E153.
Article3. Ono H, Kondo H, Gotoda T, et al. Endoscopic mucosal resection for treatment of early gastric cancer. Gut. 2001; 48:225–229.
Article4. Lee SY, Kim JJ, Lee JH, et al. Healing rate of EMR-induced ulcer in relation to the duration of treatment with omeprazole. Gastrointest Endosc. 2004; 60:213–217.
Article5. Kakushima N, Yahagi N, Fujishiro M, et al. The healing process of gastric artificial ulcers after endoscopic submucosal dissection. Dig Endosc. 2004; 16:327–331.
Article6. Park JH, Baek EK, Choi CH, et al. Comparison of the efficacy of 4- and 8-week lansoprazole treatment for ESD-induced gastric ulcers: a randomized, prospective, controlled study. Surg Endosc. 2014; 28:235–241.
Article7. Ye BD, Cheon JH, Choi KD, et al. Omeprazole may be superior to famotidine in the management of iatrogenic ulcer after endoscopic mucosal resection: a prospective randomized controlled trial. Aliment Pharmacol Ther. 2006; 24:837–843.
Article8. Takao T, Takegawa Y, Shinya N, Tsudomi K, Oka S, Ono H. Tissue shielding with polyglycolic acid sheets and fibrin glue on ulcers induced by endoscopic submucosal dissection in a porcine model. Endosc Int Open. 2015; 3:E146–E151.
Article9. Takimoto K, Toyonaga T, Matsuyama K. Endoscopic tissue shielding to prevent delayed perforation associated with endoscopic submucosal dissection for duodenal neoplasms. Endoscopy. 2012; 44 Suppl 2 UCTN:E414–E415.
Article10. Takimoto K, Imai Y, Matsuyama K. Endoscopic tissue shielding method with polyglycolic acid sheets and fibrin glue to prevent delayed perforation after duodenal endoscopic submucosal dissection. Dig Endosc. 2014; 26 Suppl 2:46–49.
Article11. Marx RE. Platelet-rich plasma (PRP): what is PRP and what is not PRP? Implant Dent. 2001; 10:225–228.
Article12. Molloy T, Wang Y, Murrell G. The roles of growth factors in tendon and ligament healing. Sports Med. 2003; 33:381–394.
Article13. Akimoto M, Hashimoto H, Maeda A, Shigemoto M, Yamashita K. Roles of angiogenic factors and endothelin-1 in gastric ulcer healing. Clin Sci (Lond). 2002; 103 Suppl 48:450S–454S.
Article14. Luo JC, Shin VY, Liu ES, et al. Dexamethasone delays ulcer healing by inhibition of angiogenesis in rat stomachs. Eur J Pharmacol. 2004; 485:275–281.
Article15. Perini R, Wallace JL, Ma L. Roles of platelets and proteinase-activated receptors in gastric ulcer healing. Dig Dis Sci. 2005; 50 Suppl 1:S12–S15.
Article16. A Hamid MS, Mohamed Ali MR, Yusof A, George J, Lee LP. Platelet-rich plasma injections for the treatment of hamstring injuries: a randomized controlled trial. Am J Sports Med. 2014; 42:2410–2418.17. Carter MJ, Fylling CP, Parnell LK. Use of platelet rich plasma gel on wound healing: a systematic review and meta-analysis. Eplasty. 2011; 11:e38.18. Chicharro-Alcántara D, Rubio-Zaragoza M, Damiá-Giménez E, et al. Platelet rich plasma: new insights for cutaneous wound healing management. J Funct Biomater. 2018; 9:E10.
Article19. Hammond JW, Hinton RY, Curl LA, Muriel JM, Lovering RM. Use of autologous platelet-rich plasma to treat muscle strain injuries. Am J Sports Med. 2009; 37:1135–1142.
Article20. Kazakos K, Lyras DN, Verettas D, Tilkeridis K, Tryfonidis M. The use of autologous PRP gel as an aid in the management of acute trauma wounds. Injury. 2009; 40:801–805.
Article21. Lacci KM, Dardik A. Platelet-rich plasma: support for its use in wound healing. Yale J Biol Med. 2010; 83:1–9.22. Mehrannia M, Vaezi M, Yousefshahi F, Rouhipour N. Platelet rich plasma for treatment of nonhealing diabetic foot ulcers: a case report. Can J Diabetes. 2014; 38:5–8.
Article23. Picard F, Hersant B, Bosc R, Meningaud JP. Should we use platelet-rich plasma as an adjunct therapy to treat “acute wounds,” “burns,” and “laser therapies”: a review and a proposal of a quality criteria checklist for further studies. Wound Repair Regen. 2015; 23:163–170.
Article24. Samani MK, Saberi BV, Ali Tabatabaei SM, Moghadam MG. The clinical evaluation of platelet-rich plasma on free gingival graft’s donor site wound healing. Eur J Dent. 2017; 11:447–454.
Article25. Suthar M, Gupta S, Bukhari S, Ponemone V. Treatment of chronic non-healing ulcers using autologous platelet rich plasma: a case series. J Biomed Sci. 2017; 24:16.
Article26. Sakita T, Fukutomi H. Endoscopic diagnosis. In : Yoshitoshi Y, editor. Ulcer of stomach and duodenum. Tokyo: Nankodo;1971. p. 198–208.27. Baniya R, Upadhaya S, Khan J, et al. Carbon dioxide versus air insufflation in gastric endoscopic submucosal dissection: a systematic review and meta-analysis of randomized controlled trials. Clin Endosc. 2017; 50:464–472.
Article28. Lee HJ, Lee YJ, Lee JY, et al. Characteristics of synchronous and metachronous multiple gastric tumors after endoscopic submucosal dissection of early gastric neoplasm. Clin Endosc. 2018; 51:266–273.
Article29. Ma L, Elliott SN, Cirino G, Buret A, Ignarro LJ, Wallace JL. Platelets modulate gastric ulcer healing: role of endostatin and vascular endothelial growth factor release. Proc Natl Acad Sci U S A. 2001; 98:6470–6475.
Article30. Hwang DL, Lev-Ran A, Yen CF, Sniecinski I. Release of different fractions of epidermal growth factor from human platelets in vitro: preferential release of 140 kDa fraction. Regul Pept. 1992; 37:95–100.
Article31. O’Reilly MS, Boehm T, Shing Y, et al. Endostatin: an endogenous inhibitor of angiogenesis and tumor growth. Cell. 1997; 88:277–285.
Article32. Wartiovaara U, Salven P, Mikkola H, et al. Peripheral blood platelets express VEGF-C and VEGF which are released during platelet activation. Thromb Haemost. 1998; 80:171–175.
Article33. Yamaguchi N, Anand-Apte B, Lee M, et al. Endostatin inhibits VEGF-induced endothelial cell migration and tumor growth independently of zinc binding. EMBO J. 1999; 18:4414–4423.
Article34. Salarinia R, Sadeghnia HR, Alamdari DH, Hoseini SJ, Mafinezhad A, Hosseini M. Platelet rich plasma: effective treatment for repairing of spinal cord injury in rat. Acta Orthop Traumatol Turc. 2017; 51:254–257.
Article35. Ronci C, Ferraro AS, Lanti A, et al. Platelet-rich plasma as treatment for persistent ocular epithelial defects. Transfus Apher Sci. 2015; 52:300–304.
Article36. Ghoddusi J, Maghsudlu A, Jafarzadeh H, Jafarian A, Forghani M. Histological evaluation of the effect of platelet-rich plasma on pulp regeneration in nonvital open apex teeth: an animal study. J Contemp Dent Pract. 2017; 18:1045–1050.37. Tambella AM, Attili AR, Dupré G, et al. Platelet-rich plasma to treat experimentally-induced skin wounds in animals: a systematic review and meta-analysis. PLoS One. 2018; 13:e0191093.
Article38. Lorenzo-Zúñiga V, Boix J, Moreno de Vega V, Bon I, Marín I, Bartolí R. Efficacy of platelet-rich plasma as a shielding technique after endoscopic mucosal resection in rat and porcine models. Endosc Int Open. 2016; 4:E859–E864.
Article39. Chahla J, Cinque ME, Piuzzi NS, et al. A call for standardization in platelet-rich plasma preparation protocols and composition reporting: a systematic review of the clinical orthopaedic literature. J Bone Joint Surg Am. 2017; 99:1769–1779.40. Bernuzzi G, Tardito S, Bussolati O, et al. Platelet gel in the treatment of cutaneous ulcers: the experience of the Immunohaematology and Transfusion Centre of Parma. Blood Transfus. 2010; 8:237–247.41. Leitner GC, Gruber R, Neumüller J, et al. Platelet content and growth factor release in platelet-rich plasma: a comparison of four different systems. Vox Sang. 2006; 91:135–139.
Article42. Kim SA, Ryu HW, Lee KS, Cho JW. Application of platelet-rich plasma accelerates the wound healing process in acute and chronic ulcers through rapid migration and upregulation of cyclin A and CDK4 in HaCaT cells. Mol Med Rep. 2013; 7:476–480.
Article43. Liou E. The development of submucosal injection of platelet rich plasma for accelerating orthodontic tooth movement and preserving pressure side alveolar bone. APOS trends in orthodontics. 2016; 6:5–11.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Platelet-rich Plasma on Burn Wounds according to Time of Application: An Experimental Study on Rats
- Therapeutic Trial of Platelet-rich Plasma for Superficial Ulcers Caused by Herpes Zoster
- Recalcitrant Cutaneous Ulcer of Comorbid Patient Treated with Platelet Rich Plasma: A Case Report
- Use of Platelet-rich Plasma
- The Effect of Platelet Rich Plasma Dosage on the Tendon Healing in Rabbits