J Korean Neurosurg Soc.
2019 Jul;62(4):450-457. 10.3340/jkns.2019.0008.
Risk Factors of Allogenous Bone Graft Collapse in Two-Level Anterior Cervical Discectomy and Fusion
- Affiliations
-
- 1Department of Neurosurgery, Pusan National University Yangsan Hospital, Yangsan, Korea. sondongwuk@gmail.com
- 2Research Institute for Convergence of Biomedical Science and Technology, Pusan National University Yangsan Hospital, Yangsan, Korea.
- 3Department of Neurosurgery, Pusan National University School of Medicine, Yangsan, Korea.
- KMID: 2463676
- DOI: http://doi.org/10.3340/jkns.2019.0008
Abstract
OBJECTIVE
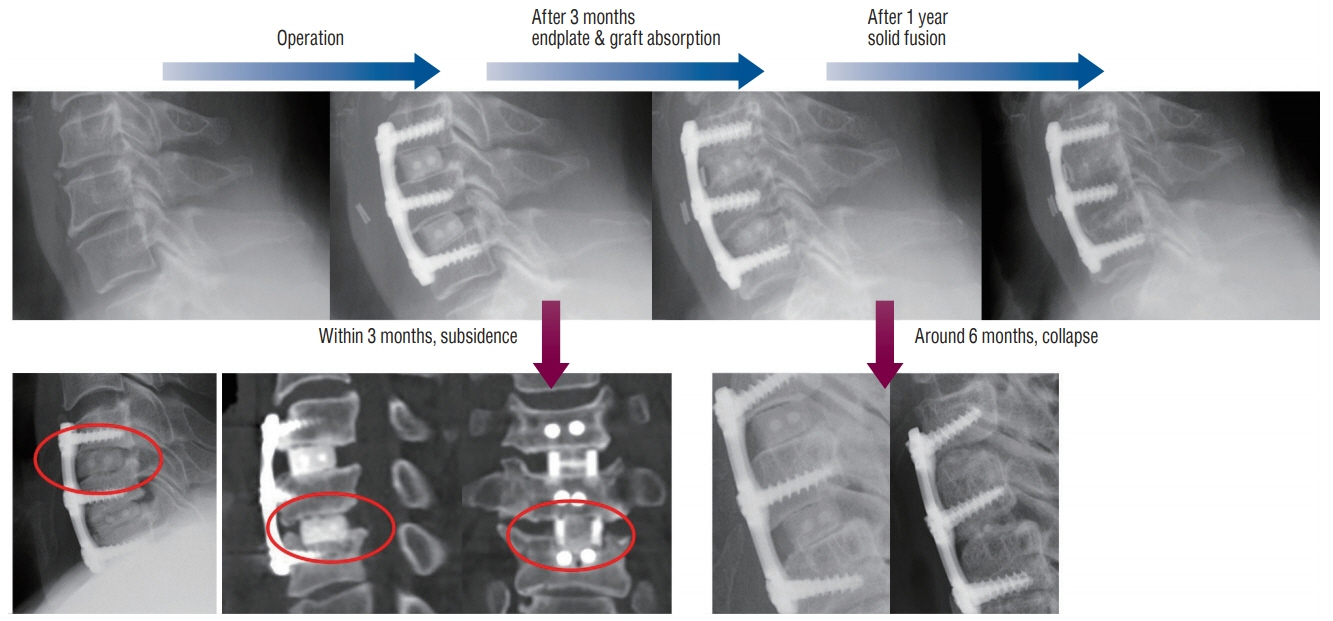
Anterior cervical discectomy and fusion (ACDF) is commonly used surgical procedure for cervical degenerative disease. Among the various intervertebral spacers, the use of allografts is increasing due to its advantages such as no harvest site complications and low rate of subsidence. Although subsidence is a rare complication, graft collapse is often observed in the follow-up period. Graft collapse is defined as a significant graft height loss without subsidence, which can lead to clinical deterioration due to foraminal re-stenosis or segmental kyphosis. However, studies about the collapse of allografts are very limited. In this study, we evaluated risk factors associated with graft collapse.
METHODS
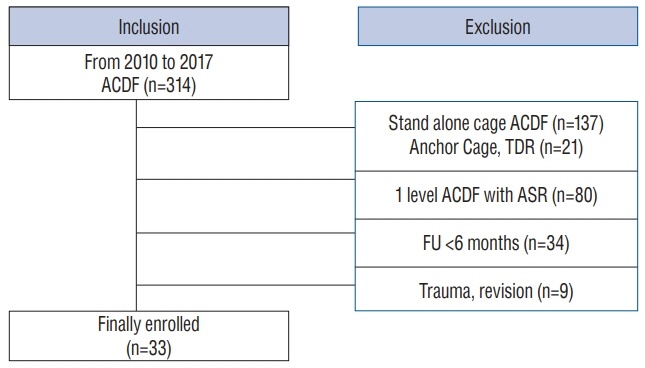
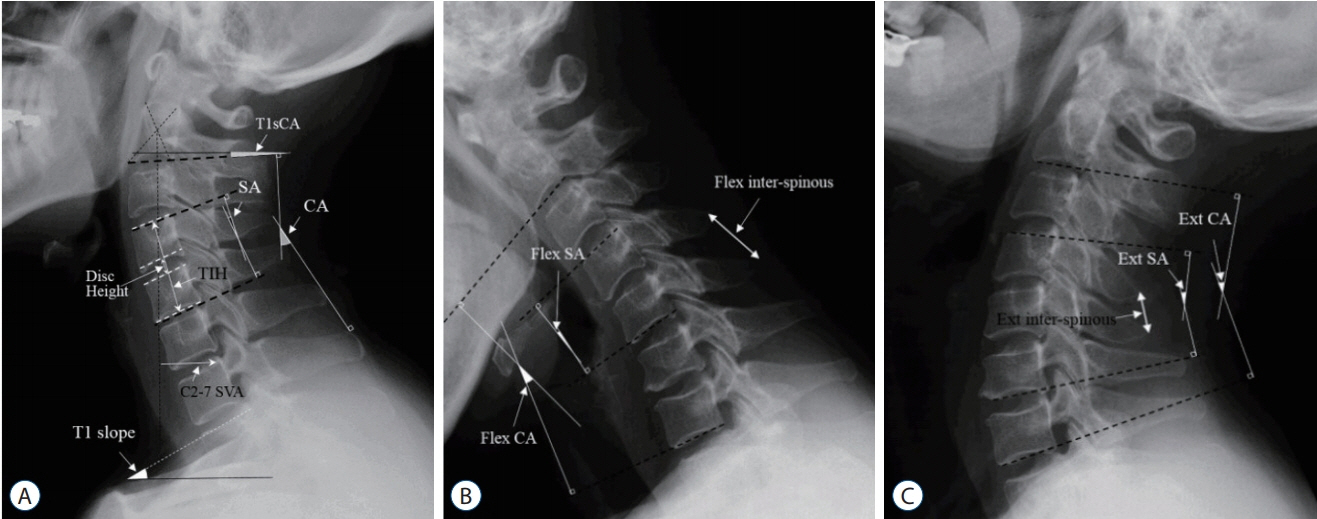
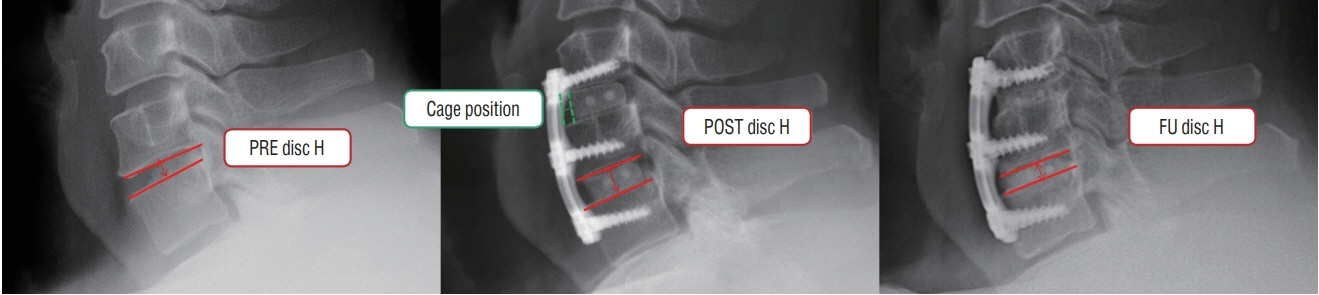
We retrospectively reviewed 33 patients who underwent two level ACDF with anterior plating using allogenous bone graft from January 2013 to June 2017. Various factors related to cervical sagittal alignment were measured preoperatively (PRE), postoperatively (POST), and last follow-up. The collapse was defined as the ratio of decrement from POST disc height to follow-up disc height. We also defined significant collapses as disc heights that were decreased by 30% or more after surgery. The intraoperative distraction was defined as the ratio of increment from PRE disc height to POST disc height.
RESULTS
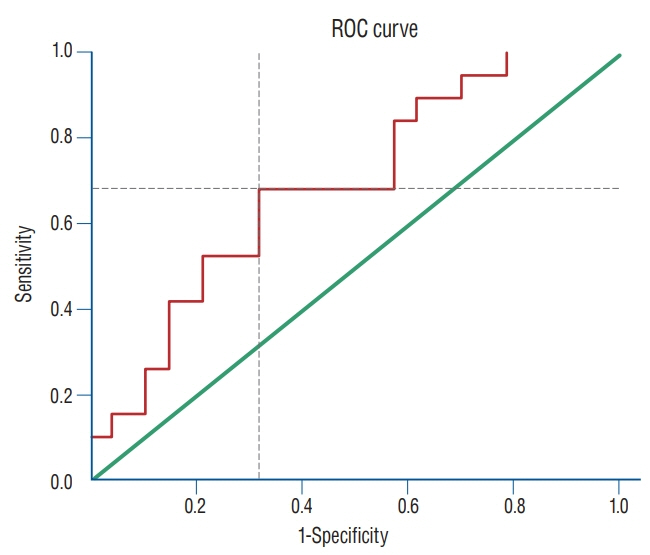
The subsidence rate was 4.5% and graft collapse rate was 28.8%. The pseudarthrosis rate was 16.7% and there was no association between pseudarthrosis and graft collapse. Among the collapse-related risk factors, pre-operative segmental angle (p=0.047) and intra-operative distraction (p=0.003) were significantly related to allograft collapse. The cut-off value of intraoperative distraction ≥37.3% was significantly associated with collapse (p=0.009; odds ratio, 4.622; 95% confidence interval, 1.470-14.531). The average time of events were as follows: collapse, 5.8±5.7 months; subsidence, 0.99±0.50 months; and instrument failure, 9.13±0.50 months.
CONCLUSION
We experienced a higher frequency rate of collapse than subsidence in ACDF using an allograft. Of the various pre-operative factors, intra-operative distraction was the most predictable factor of the allograft collapse. This was especially true when the intraoperative distraction was more than 37%, in which case the occurrence of graft collapse increased 4.6 times. We also found that instrument failure occurs only after the allograft collapse.
MeSH Terms
Figure
Reference
-
References
1. Barsa P, Suchomel P. Factors affecting sagittal malalignment due to cage subsidence in standalone cage assisted anterior cervical fusion. Eur Spine J. 16:1395–1400. 2007.
Article2. Bartels RH, Donk RD, Feuth T. Subsidence of stand-alone cervical carbon fiber cages. Neurosurgery. 58:502–508. 2006.
Article3. Bishop RC, Moore KA, Hadley MN. Anterior cervical interbody fusion using autogeneic and allogeneic bone graft substrate: a prospective comparative analysis. J Neurosurg. 85:206–210. 1996.
Article4. Brown MD, Malinin TI, Davis PB. A roentgenographic evaluation of frozen allografts versus autografts in anterior cervical spine fusions. Clin Orthop Relat Res. 231–236. 1976.
Article5. Cowan JA Jr, Dimick JB, Wainess R, Upchurch GR Jr, Chandler WF, La Marca F. Changes in the utilization of spinal fusion in the United States. Neurosurgery. 59:15–20. 2006.6. Fernyhough JC, Schimandle JJ, Weigel MC, Edwards CC, Levine AM. Chronic donor site pain complicating bone graft harvesting from the posterior iliac crest for spinal fusion. Spine (Phila Pa 1976). 17:1474–1480. 1992.
Article7. Francke EI, Demetropoulos CK, Agabegi SS, Truumees E, Herkowitz HN. Distractive force relative to initial graft compression in an in vivo anterior cervical discectomy and fusion model. Spine (Phila Pa 1976). 35:526–530. 2010.
Article8. Gercek E, Arlet V, Delisle J, Marchesi D. Subsidence of stand-alone cervical cages in anterior interbody fusion: warning. Eur Spine J. 12:513–516. 2003.
Article9. Gore DR, Sepic SB. Anterior cervical fusion for degenerated or protruded discs. A review of one hundred forty-six patients. Spine (Phila Pa 1976). 9:667–671. 1984.10. Hu R, Hearn T, Yang J. Bone graft harvest site as a determinant of iliac crest strength. Clin Orthop Relat Res. 252–256. 1995.
Article11. Kurz LT, Garfin SR, Booth RE Jr. Harvesting autogenous iliac bone grafts. A review of complications and techniques. Spine (Phila Pa 1976). 14:1324–1331. 1989.12. Lee SH, Lee JS, Sung SK, Son DW, Lee SW, Song GS. A lower T1 slope as a predictor of subsidence in anterior cervical discectomy and fusion with stand-alone cages. J Korean Neurosurg Soc. 60:567–576. 2017.
Article13. Lee SH, Son DW, Lee JS, Kim DH, Sung SK, Lee SW, et al. Differences in cervical sagittal alignment changes in patients undergoing laminoplasty and anterior cervical discectomy and fusion. Neurospine. 15:91–100. 2018.
Article14. Lim TH, Kwon H, Jeon CH, Kim JG, Sokolowski M, Natarajan R, et al. Effect of endplate conditions and bone mineral density on the compressive strength of the graft-endplate interface in anterior cervical spine fusion. Spine (Phila Pa 1976). 26:951–956. 2001.
Article15. McGuire KJ, Harrast J, Herkowitz H, Weinstein JN. Geographic variation in the surgical treatment of degenerative cervical disc disease: American Board of Orthopedic Surgery Quality Improvement Initiative; part II candidates. Spine (Phila Pa 1976). 37:57–66. 2012.
Article16. Miller LE, Block JE. Safety and effectiveness of bone allografts in anterior cervical discectomy and fusion surgery. Spine (Phila Pa 1976). 36:2045–2050. 2011.
Article17. Park JY, Choi KY, Moon BJ, Hur H, Jang JW, Lee JK. Subsidence after single-level anterior cervical fusion with a stand-alone cage. J Clin Neurosci. 33:83–88. 2016.
Article18. Pelker RR, Friedlaender GE, Markham TC. Biomechanical properties of bone allografts. Clin Orthop Relat Res. 54–57. 1983.
Article19. Rajaee SS, Bae HW, Kanim LE, Delamarter RB. Spinal fusion in the United States: analysis of trends from 1998 to 2008. Spine (Phila Pa 1976). 37:67–76. 2012.20. Sasso RC, LeHuec JC, Shaffrey C; Spine Interbody Research Group. Iliac crest bone graft donor site pain after anterior lumbar interbody fusion: a prospective patient satisfaction outcome assessment. J Spinal Disord Tech. 18 Suppl:S77–S81. 2005.21. Schmieder K, Wolzik-Grossmann M, Pechlivanis I, Engelhardt M, Scholz M, Harders A. Subsidence of the wing titanium cage after anterior cervical interbody fusion: 2-year follow-up study. J Neurosurg Spine. 4:447–453. 2006.
Article22. Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am. 40-A:607–624. 1958.
Article23. Suchomel P, Barsa P, Buchvald P, Svobodnik A, Vanickova E. Autologous versus allogenic bone grafts in instrumented anterior cervical discectomy and fusion: a prospective study with respect to bone union pattern. Eur Spine J. 13:510–515. 2004.
Article24. Tuchman A, Brodke DS, Youssef JA, Meisel HJ, Dettori JR, Park JB, et al. Autograft versus allograft for cervical spinal fusion: a systematic review. Global Spine J. 7:59–70. 2017.25. Yang JJ, Yu CH, Chang BS, Yeom JS, Lee JH, Lee CK. Subsidence and nonunion after anterior cervical interbody fusion using a stand-alone polyetheretherketone (PEEK) cage. Clin Orthop Surg. 3:16–23. 2011.
Article26. Zdeblick TA, Ducker TB. The use of freeze-dried allograft bone for anterior cervical fusions. Spine (Phila Pa 1976). 16:726–729. 1991.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anterior Cervical Fusion with or without Plates after Discectomy in Cervical Spondylosis
- Comparative Study of Clinical Outcomes of Anterior Cervical Discectomy and Fusion Using Autobone Graft or Cage with Bone Substitute
- An Early Comparative Analysis of the Use of Autograft Versus Allograft in Anterior Cervical Discectomy and Fusion
- Analysis of Noninstrumented Anterior Cervical Discectomy and Interbody Fusion in Degenerative Cervical Disease
- Anterior Discectomy and Fusion with Plate Fixation for Cervical Disc Herniation