J Liver Cancer.
2019 Sep;19(2):165-170. 10.17998/jlc.19.2.165.
Early Onset Polymorphic Post-transplant Lymphoproliferative Disease Mimicking a Solitary Necrotizing Abscess in a Graft Liver
- Affiliations
-
- 1Department of Internal Medicine, Eunpyeong St. Mary's Hospital, Seoul, Korea.
- 2Department of Internal Medicine, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. yoonsk@catholic.ac.kr
- KMID: 2463619
- DOI: http://doi.org/10.17998/jlc.19.2.165
Abstract
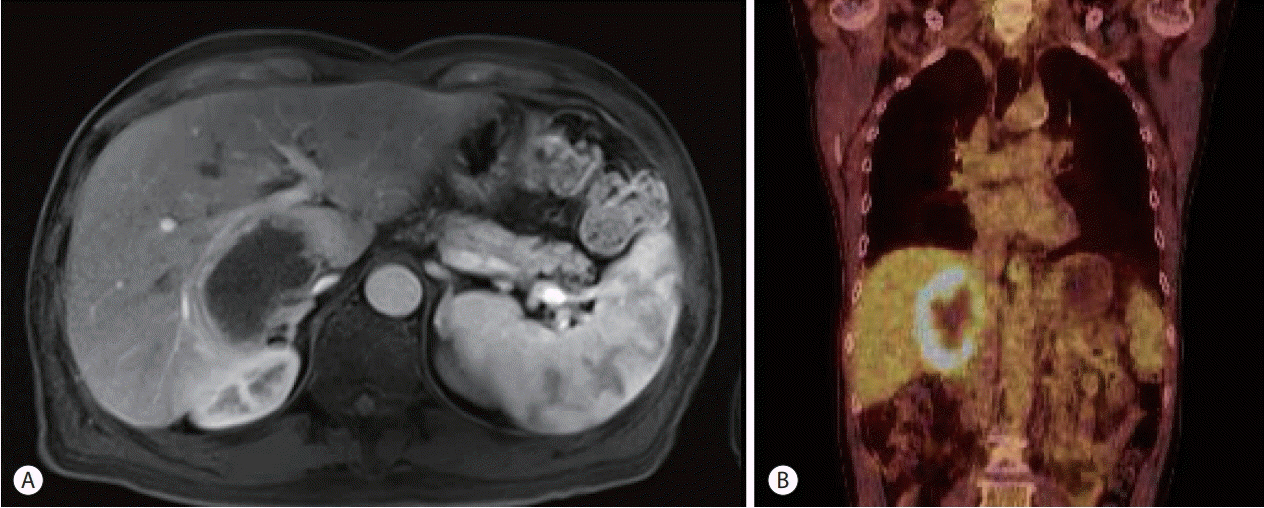
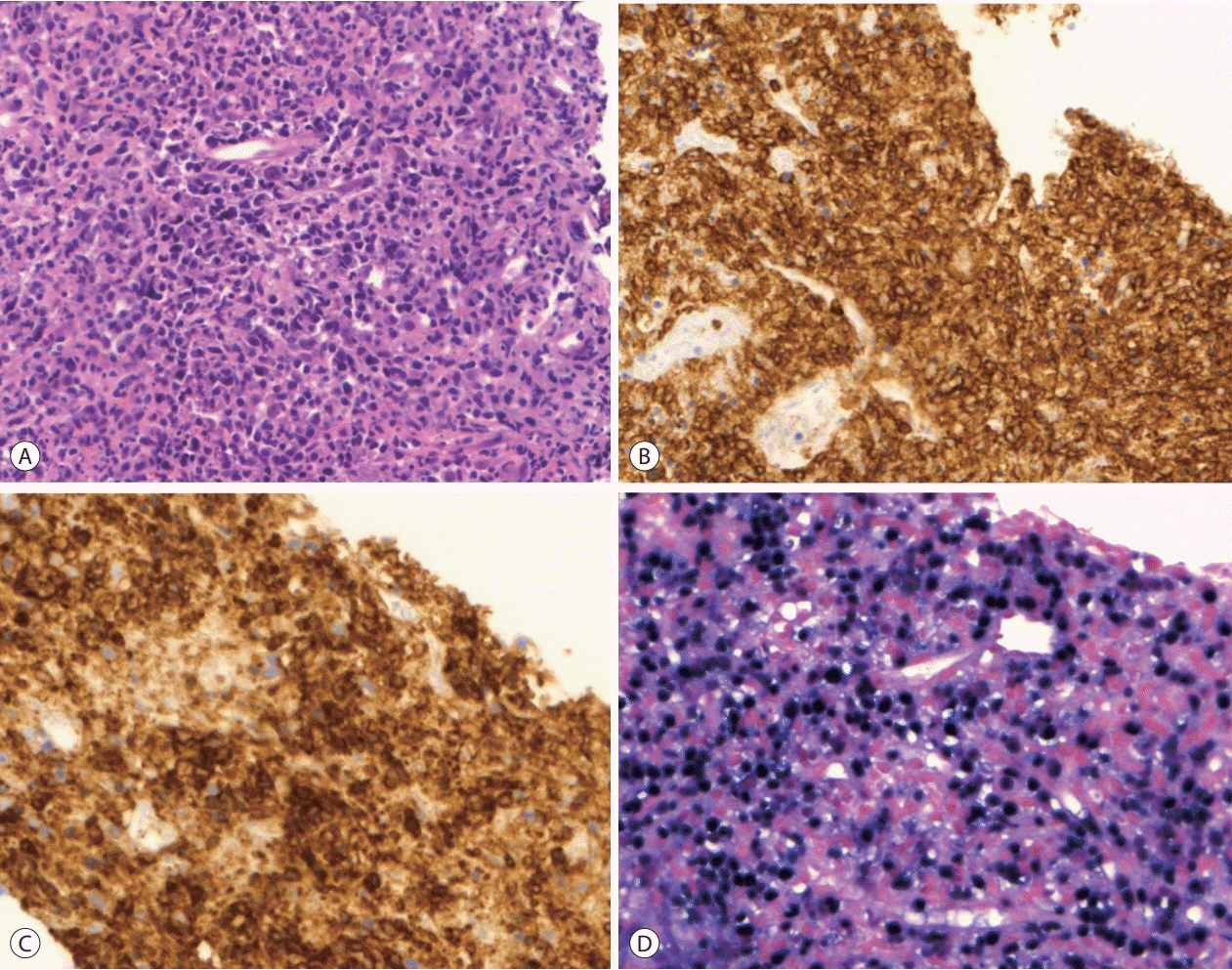
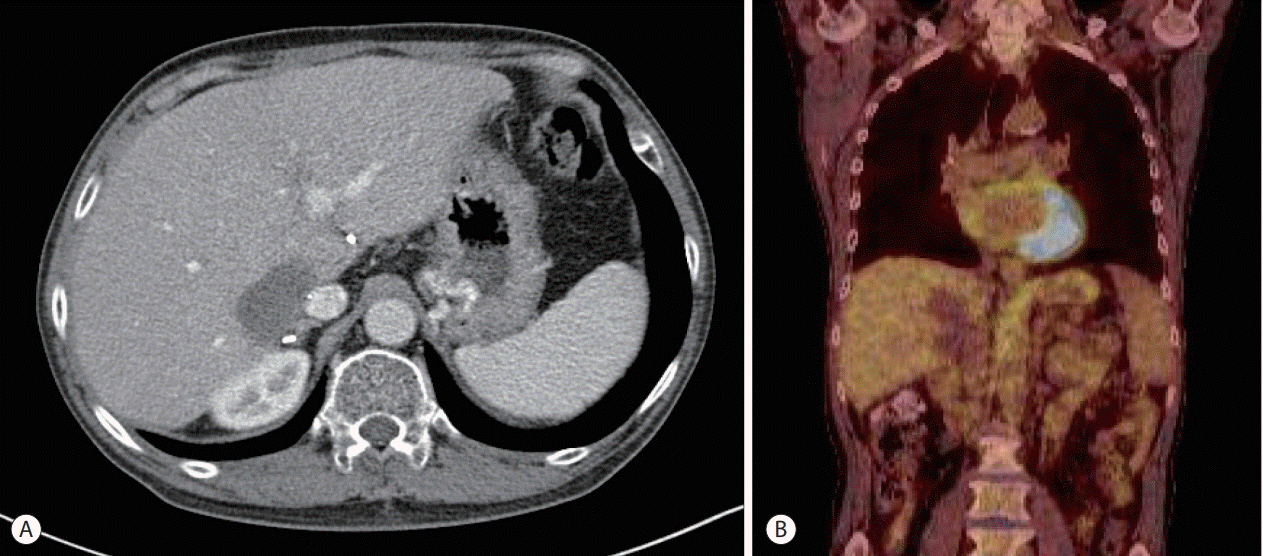
- Although post-transplantation lymphoproliferative disease (PTLD) after liver transplantation is very rare, its prognosis is worse than that of PTLD following other types of solid organ transplantation. Here, we report a rare case of early onset polymorphic PTLD in a graft liver occurring five months after deceased-donor liver transplantation due to hepatocellular carcinoma and hepatitis C virus infection. Initially, findings from contrast-enhanced magnetic resonance imaging mistakenly suspected the lesion was a necrotizing abscess with central necrosis. However, ¹â¸F-fluorodeoxyglucose positron emission tomography and biopsy findings confirmed an Epstein-Barr virus (EBV)-associated, B cell type polymorphic PTLD with central necrosis. Our case suggests regular monitoring of EBV serologic status for liver transplant recipients who were initially in an EBV seronegative state. Although early-onset PTLD is very rare after liver transplantation, PTLD should be suspected when recipients show the seroconversion for EBV proteins and the development of new tumors with various clinical presentations.
Keyword
MeSH Terms
Figure
Reference
-
1. Jiang Y, Villeneuve PJ, Fenton SS, Schaubel DE, Lilly L, Mao Y. Liver transplantation and subsequent risk of cancer: findings from a Canadian cohort study. Liver Transpl. 2008; 14:1588–1597.2. Dierickx D, Cardinaels N. Posttransplant lymphoproliferative disorders following liver transplantation: where are we now? World J Gastroenterol. 2015; 21:11034–11043.3. Hatton O, Martinez OM, Esquivel CO. Emerging therapeutic strategies for Epstein-Barr virus+ post-transplant lymphoproliferative disorder. Pediatr Transplant. 2012; 16:220–229.4. Dierickx D, Tousseyn T, Gheysens O. How I treat posttransplant lymphoproliferative disorders. Blood. 2015; 126:2274–2283.5. Lauro A, Arpinati M, Pinna AD. Managing the challenge of PTLD in liver and bowel transplant recipients. Br J Haematol. 2015; 169:157–172.6. Petrara MR, Giunco S, Serraino D, Dolcetti R, De Rossi A. Posttransplant lymphoproliferative disorders: from epidemiology to pathogenesis-driven treatment. Cancer Lett. 2015; 369:37–44.7. Kim H, Yi NJ, Lee J, Kim J, Moon MR, Jeong J, et al. Safety of reduced dose of mycophenolate mofetil combined with tacrolimus in living-donor liver transplantation. Clin Mol Hepatol. 2014; 20:291–299.8. Jagadeesh D, Woda BA, Draper J, Evens AM. Post transplant lymphoproliferative disorders: risk, classification, and therapeutic recommendations. Curr Treat Options Oncol. 2012; 13:122–136.9. Jain A, Nalesnik M, Reyes J, Pokharna R, Mazariegos G, Green M, et al. Posttransplant lymphoproliferative disorders in liver transplantation: a 20-year experience. Ann Surg. 2002; 236:429–436. ;discussion 436-437.10. Leblond V, Choquet S. Lymphoproliferative disorders after liver transplantation. J Hepatol. 2004; 40:728–735.11. Al-Mansour Z, Nelson BP, Evens AM. Post-transplant lymphoproliferative disease (PTLD): risk factors, diagnosis, and current treatment strategies. Curr Hematol Malig Rep. 2013; 8:173–183.12. Kamdar KY, Rooney CM, Heslop HE. Posttransplant lymphoproliferative disease following liver transplantation. Curr Opin Organ Transplant. 2011; 16:274–280.13. Yoon SO, Yu E, Cho YM, Suh C, Kim KM, Han DJ, et al. Posttransplant lymphoproliferative disorders: clinicopathological analysis of 43 cases in a single center, 1990-2009. Clin Transplant. 2012; 26:67–73.14. Izadi M, Taheri S. Features, predictors and prognosis of lymphoproliferative disorders post-liver transplantation regarding disease presentation time: report from the PTLD. Int. survey. Ann Transplant. 2011; 16:39–47.15. Nieters A, Kallinowski B, Brennan P, Ott M, Maynadié M, Benavente Y, et al. Hepatitis C and risk of lymphoma: results of the European multicenter case-control study EPILYMPH. Gastroenterology. 2006; 131:1879–1886.16. Morton LM, Landgren O, Chatterjee N, Castenson D, Parsons R, Hoover RN, et al. Hepatitis C virus infection and risk of posttransplantation lymphoproliferative disorder among solid organ transplant recipients. Blood. 2007; 110:4599–4605.17. Cazzola M. Introduction to a review series: the 2016 revision of the WHO classification of tumors of hematopoietic and lymphoid tissues. Blood. 2016; 127:2361–2364.18. Parker A, Bowles K, Bradley JA, Emery V, Featherstone C, Gupte G, et al. Diagnosis of post-transplant lymphoproliferative disorder in solid organ transplant recipients - BCSH and BTS Guidelines. Br J Haematol. 2010; 149:675–692.19. Martínez-Calle N, Alfonso A, Rifón J, Herrero I, Errasti P, Rábago G, et al. First-line use of rituximab correlates with increased overall survival in late post-transplant lymphoproliferative disorders: retrospective, single-centre study. Eur J Haematol. 2017; 98:38–43.20. Evens AM, David KA, Helenowski I, Nelson B, Kaufman D, Kircher SM, et al. Multicenter analysis of 80 solid organ transplantation recipients with post-transplantation lymphoproliferative disease: outcomes and prognostic factors in the modern era. J Clin Oncol. 2010; 28:1038–1046.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pediatric Liver Transplantation
- Post-transplant lymphoproliferative disorder presented as small bowel intussusception in adult liver transplant patient
- Post-transplantation Lymphoproliferative Disorder in Transplanted Liver: A Case Report
- Solitary Eosinophilic Liver Abscess Mimicking Hepatocellular Carcinoma
- Cerebral Post-Transplant Lymphoproliferative Disorder Occurring after Renal Transplantation: A Case Report